Previous studies have shown that depression tends to be seriously undertreated, although effective treatments have been available for decades (
9 ). Results from the National Comorbidity Survey Replication, for example, indicate that, in 2001–2003, only 37.5% of people with major depression received adequate conventional treatment for their disorder (
10 ). The cost to individuals, families, and society of this undertreatment is substantial (
9,
11,
12 ).
A number of community studies have been conducted concerning the factors affecting use of complementary and alternative medicine (
13,
14,
16,
17,
21,
22 ), and many of these have found that sociodemographic factors—such as age (
17,
20,
22,
23,
24 ), race or ethnicity (
15,
22,
23,
25,
26,
27,
28,
29 ), education (
19,
20,
24,
26,
27,
28,
30 ), marital status (
23 ), and geographic region (
19,
24,
26,
31 )—as well as having poor physical health or one or more long-term medical conditions (
19,
20,
23,
26,
29 ) are associated with use of complementary and alternative medicine in general (
15,
17,
19,
20,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31 ). Few of these studies, however, have specifically examined the relationships between use of complementary and alternative medicine and particular types of health conditions, such as psychiatric problems (
18,
24,
32 ). Research on women with depression is particularly important because of their high rate of use of complementary and alternative medicine (
18 ).
Some studies have also inquired about users' own perceptions of their reasons for using complementary and alternative therapies. Astin (
16 ) found that a major motivating factor was having the sense that complementary and alternative therapies were in harmony with the users' values and "philosophical orientations towards health and life"; Unützer and colleagues (
19 ) found high rates of use of complementary and alternative medicine among individuals who were relatively dissatisfied with conventional health care services, including mental health care services. In these studies, however, the particular types of complementary and alternative therapies these users chose for themselves were not examined in relation to these motivational factors.
This study examined the types of complementary and alternative therapies used by women with depression and examined the use of these various types of therapies in relation to sociodemographic factors and reasons or motivations for using these therapies. We aimed to enhance knowledge about the patterns of use of complementary and alternative medicine among women with depression, so that mental health professionals employing conventional methods may better understand the health-related practices of their patients and improve their communication with these patients about the benefits and the potential risks associated with alternative therapy use, either alone or in conjunction with conventional medical treatments.
Methods
Sample and data
The data used in our analyses are from a cross-sectional telephone survey of women aged 18 and older living in the United States (
33 ). The study was designed to provide nationally representative data on women's use of complementary and alternative medicine within the past year, as well as on use of complementary and alternative medicine among women in several specific ethnic minority groups. The study design and methodology are described elsewhere (
33,
34,
35 ). The interviews were conducted in 2001 in English, Spanish, or Chinese (Mandarin or Cantonese), according to respondents' preferences. Data were weighted to account for each respondent's probability of being selected given the number of potential respondents in her household. The unweighted sample consisted of 3,068 women (
33 ). The weighted sample size of the total sample is 3,921; of these women, 19% were non-Hispanic white, 28% were African American, 27% were Mexican American, and 26% were Chinese American. For this article, a subsample consisting of the 220 women who reported past-year medically diagnosed depression was used in the analyses (weighted N=282).
Measures
Use of complementary and alternative medicine. Respondents were asked about their use, for a particular health problem or concern, of any of a number of categories of complementary and alternative therapies, during the past year.
Of the nine major categories of complementary/alternative therapies covered, the three most popularly cited (each cited by 15% or more of the sample) were chiropractic or other manual therapies (such as massage or acupressure), medicinal herbs and teas, and vitamins and nutritional supplements.
For the purposes of the study reported here, specific dichotomous variables covering each of these three popular types of complementary and alternative therapies are used in our analyses. We also used a dichotomous summary variable, "any use," indicating whether respondents used any of the nine major categories of complementary and alternative therapies in the past year; these nine categories include the three mentioned above and the six less popular categories, which were techniques such as yoga, meditation, or tai chi; acupuncture; remedies or practices associated with a particular culture, such as Chinese medicine, Ayurveda, Native American healing, or curanderismo; a special diet such as a whole foods, macrobiotic, or other vegetarian diet; homeopathic remedies; and energy therapies like Reiki or therapeutic touch.
Although the respondents also cited, fairly frequently, another category of complementary and alternative therapies, namely "spirituality, religion or prayer for health reasons" (
34 ), it has been excluded from our analyses, because this study aimed to examine complementary and alternative therapies other than religion or prayer.
Reasons for use. Respondents who reported use of complementary and alternative medicine were asked about their reasons for use. The response options offered in the questionnaire included four related to respondents' experiences with conventional treatment: "I couldn't afford conventional treatment," "I tried a conventional medical treatment and it did not work," "I tried a conventional medical treatment and it had side effects that I did not like," and "My doctor recommended it." The response items also offered four more general reasons: "Using these types of remedies and treatments is consistent with my beliefs," "I wanted a natural approach to treatment," "When I was growing up family members or other people who were close to me used these types of remedies," and "I read something or heard something on TV or on the radio that convinced me to use them."
Demographics and socioeconomic status. Respondents were asked about their age, employment status, marital status, years of education, and total household income in the past year. Information was also recorded on race or ethnicity and geographic region.
Other measures. Respondents were also asked whether they had been born in the United States, how long they had lived in the United States, and about their perceived health status.
Analysis
Descriptive statistics are presented for the sample characteristics and the respondents' patterns of use of complementary and alternative medicine. After examining bivariate associations between use of specific types of complementary and alternative medicine, sociodemographic and socioeconomic factors, and perceived health status, we conducted multiple logistic regression analyses for each of the four binary outcome variables representing use of complementary and alternative medicine to examine the association between a given outcome and a given factor, when the other variables were adjusted for in the model. Finally, among the 110 women in this subsample (weighted N=151) who reported using any complementary and alternative medicine, we examined bivariate associations between the reasons for use and the particular types of therapies used.
Results
More than half the sample (54%) reported using complementary and alternative medicine for specific health reasons in the year before the interview; 26% reported use of manual therapies, 20% reported use of herbal therapies, and 16% reported use of vitamins and nutritional supplements.
Bivariate analyses
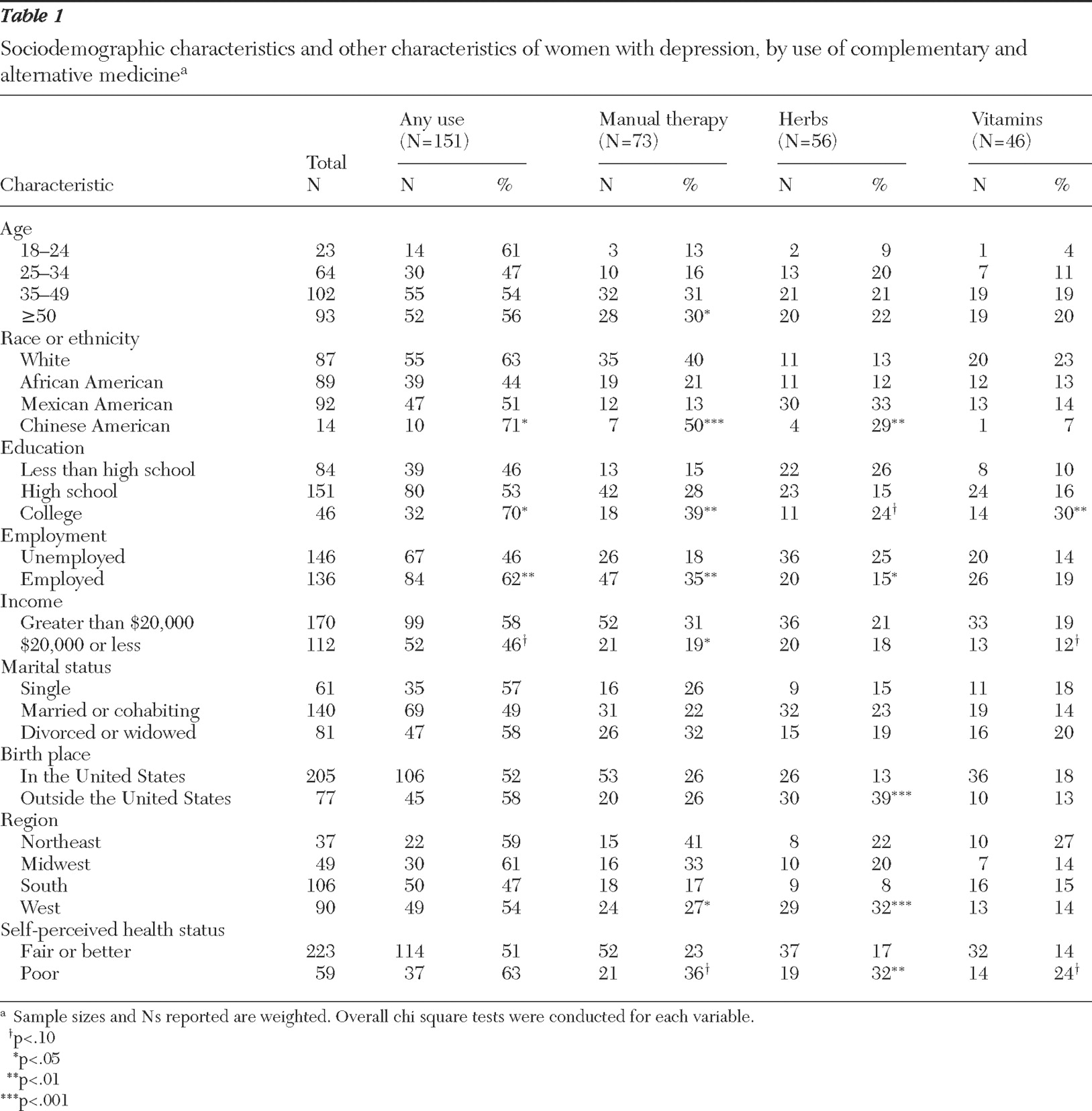
Table 1 displays the reported rates of any use of complementary and alternative medicine and rates of use of each of the three popular categories of complementary and alternative medicine (manual therapies, herbs, and vitamins), by sociodemographic and socioeconomic categories and by perceived health status.
Any use was significantly associated with race or ethnicity, education, and employment status. Among the four ethnic groups, the prevalence of any use was lowest in the African-American group and highest in the Chinese-American group. Rates of any use increased with education level. Unemployed women were less likely than employed women to use any complementary and alternative medicine. Low-income women appeared to be less likely than those with higher incomes to use these therapies. However, the difference was only marginally significant.
Use of manual therapies was significantly associated with age, race or ethnicity, education, employment status, income, and geographical region. Women aged 35 and older were about twice as likely as those younger than 35 to use manual therapies. Among the four ethnic groups, Mexican Americans had the lowest rate of use of manual therapies, whereas Chinese Americans had the highest rate. Similar to the findings for any use, the proportion using manual therapies increased with education, employment, and income.
There were significant regional differences in use of manual therapies, with rates ranging from 17% in the South to 41% in the Northeast. Use of manual therapies was somewhat more prevalent among those perceiving themselves to be in poor health, compared with those reporting fair, good, or excellent health.
Use of herbs was significantly associated with race or ethnicity, employment status, birthplace, region, and perceived health and was marginally associated with education. Among the ethnic groups, the rate of use of herbs was lowest among African Americans, relatively low among non-Hispanic whites, and high among Mexican Americans and Chinese Americans. Respondents were significantly more likely to use herbs if they were unemployed or were immigrants. Also, the regional prevalence of herb use was highest in the West, a prevalence that was more than three times higher than in the South.
Use of vitamin-based therapies increased significantly with education level. Its associations with income and poor perceived health were only marginally significant.
Multiple logistic regression analyses
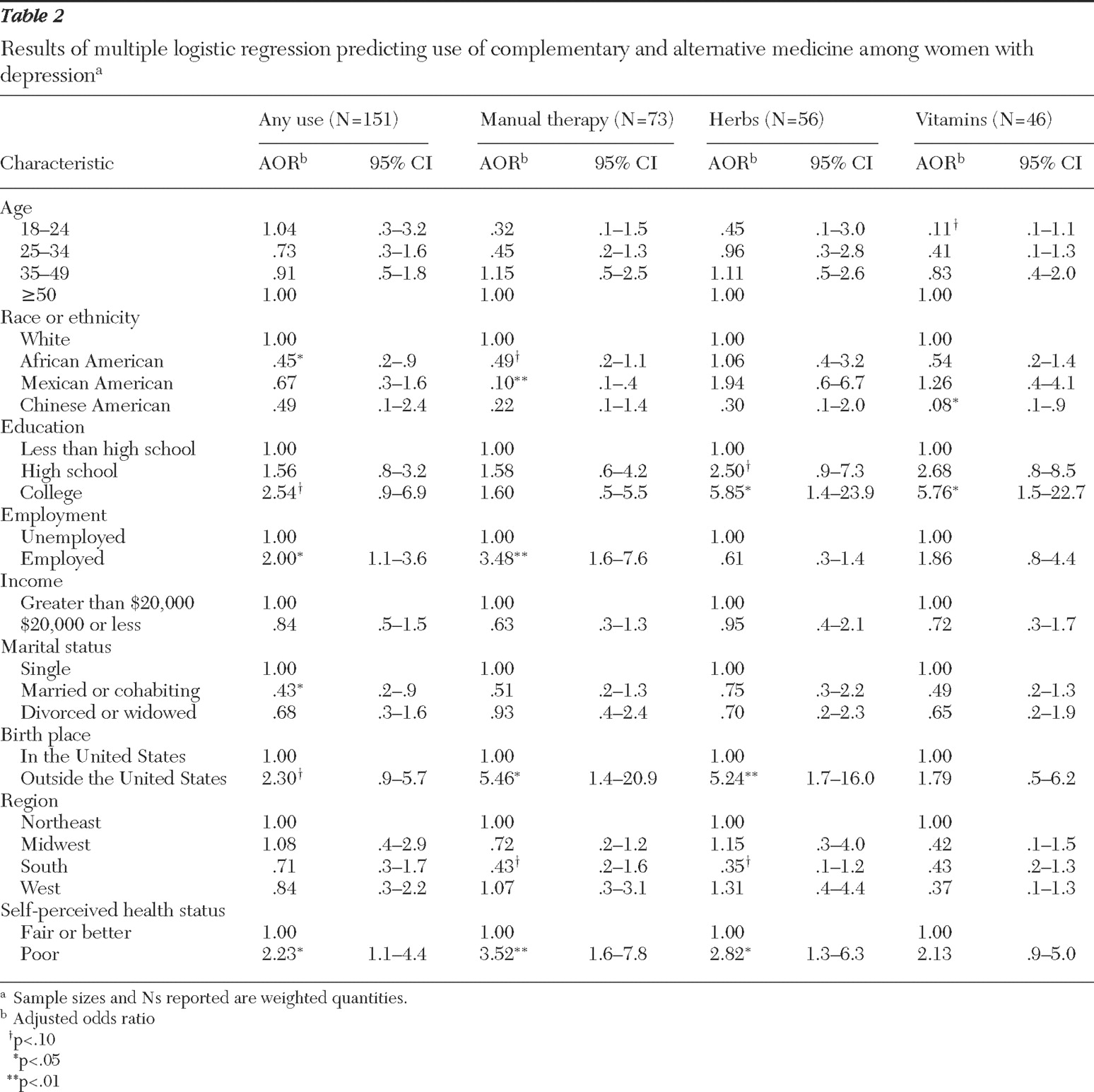
Sociodemographic and socioeconomic factors are often significantly associated with each other. We conducted multiple logistic regression analyses to reveal the unique contribution of each factor on the use outcome variables, and the analyses adjusted for other factors. The results are summarized in
Table 2 .
Non-Hispanic whites remained significantly more likely than African Americans to use complementary and alternative medicine in general, after the analyses controlled for the other sociodemographic factors. The other interethnic differences in general use were not significant.
As with the results of the bivariate analyses, results of the multivariate analyses showed any use to be associated with employment status and to have a positive association with education level, although this finding was no longer significant. Married women were significantly less likely than unmarried women to use complementary and alternative therapies. Perceived poor health significantly predicted any use.
Some interesting differences were found for use of the three individually examined types of complementary and alternative medicine (manual therapies, herbs, and vitamins). Mexican Americans differed from the other ethnic groups in being the least likely to use manual therapies, significantly less so than non-Hispanic whites. Chinese Americans were the least likely to use vitamin-based therapies, significantly less so than non-Hispanic whites. College-educated respondents were more likely than those who had not completed high school to use herbs and vitamins. Employment status was significantly associated only with use of manual therapies. Immigrants were more likely than those born in the United States to use manual therapies and herbs. Finally, perceived poor health was associated with the use of manual therapies and herbs.
Reasons for using complementary and alternative medicine
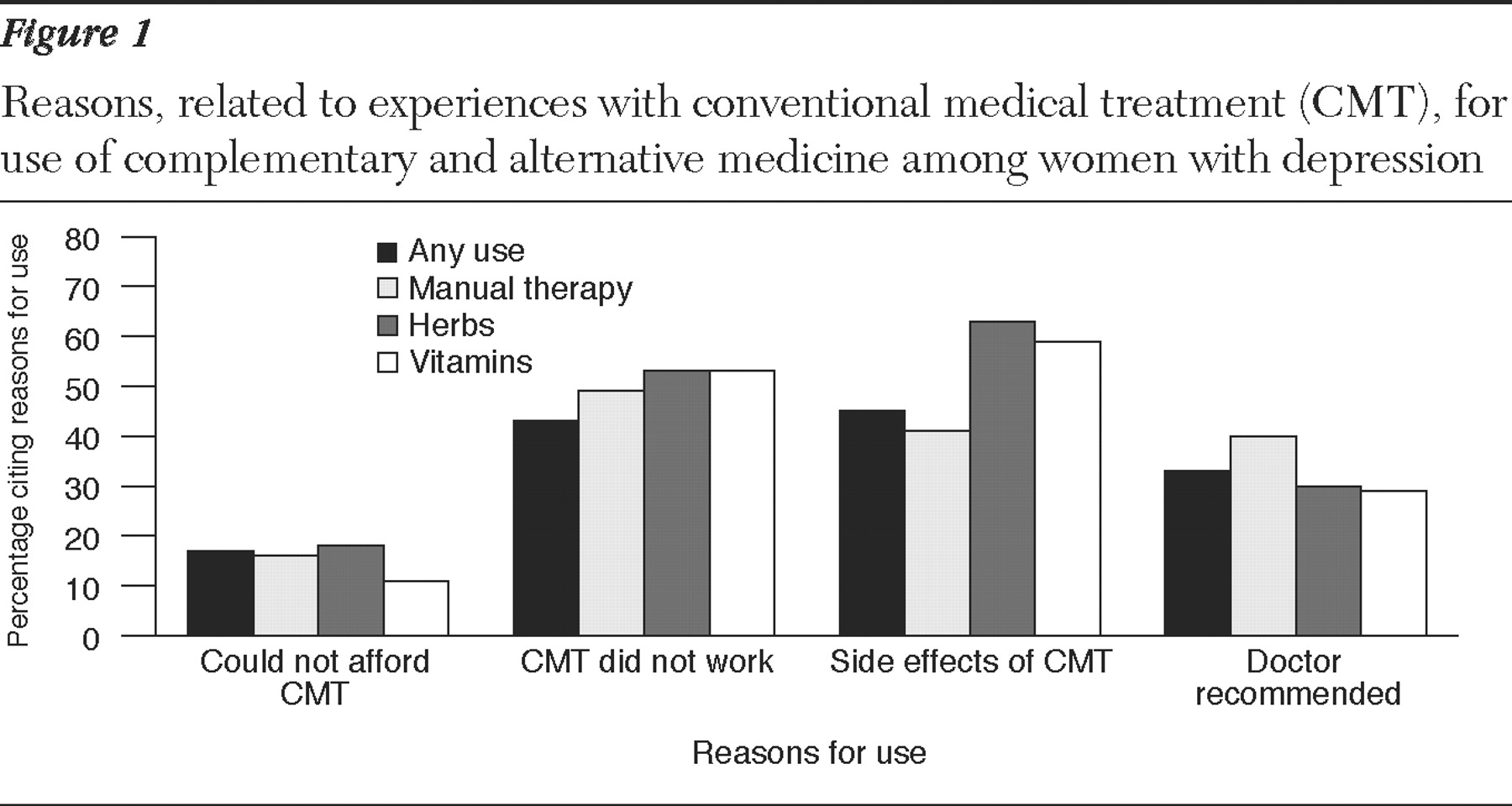
Users of complementary and alternative medicine were asked about their reasons for using complementary and alternative therapies. Four of the response options offered had to do with experiences with conventional treatment.
Figure 1 shows the proportions citing each of these four reasons, by type of therapy used.
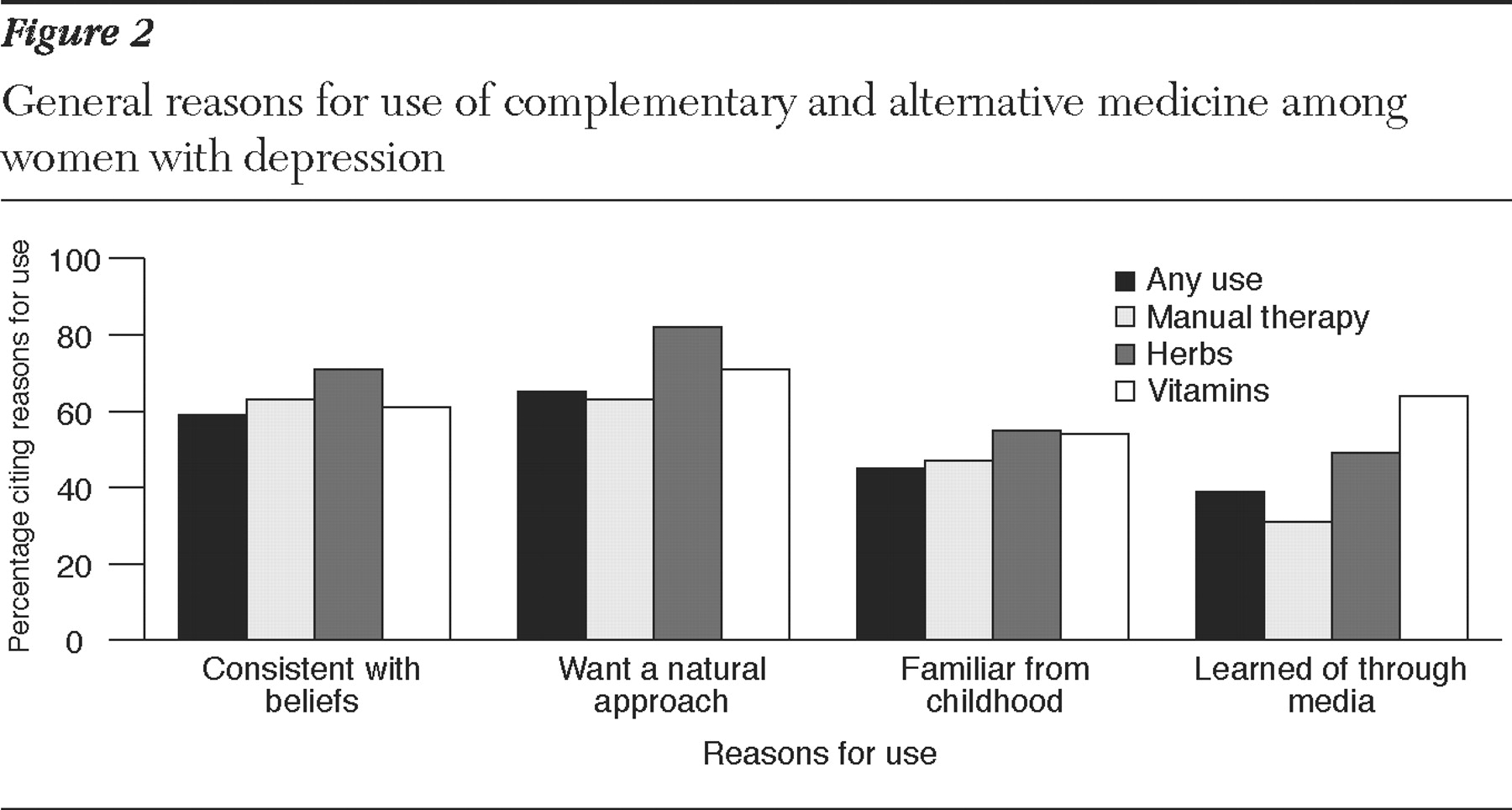
Figure 2 shows the corresponding results for the other frequently cited reasons for use of these therapies.
Forty-five percent of the users of complementary and alternative medicine cited unpleasant side effects of conventional medical treatment as a reason for use of complementary and alternative medicine; a similar proportion (43%) said that they had "tried a conventional medical treatment and it didn't work." Thirty-three percent reported that a doctor had recommended a complementary or alternative therapy to them, and 17% reported that they had used complementary and alternative medicine because they "couldn't afford conventional medical treatment."
In some instances, use of a particular type of complementary and alternative medicine was significantly associated with a particular reason. For example, side effects of conventional treatment were significantly more likely to be cited as a reason by herbal medicine users (odds ratio [OR]=3.1, p=.001) and vitamin users (OR=2.2, p=.026), compared with users of the other types of complementary and alternative medicine.
Among the four other reasons for use (
Figure 2 ), the most frequently cited reason for any use was "wanted a natural approach" (65%), followed by "consistent with my beliefs" (59%). Forty-five percent said they had become familiar with the complementary and alternative remedies in childhood because family members and friends had used them, and 39% had read something or heard something on TV or on radio that convinced them to use them.
The specific types of complementary and alternative therapies associated with this second set of reasons were herbal medicines and vitamins. Thus both vitamin users and herb users were more likely than others to cite information from the media as a reason (OR=4.8, p=.001, and OR=3.6, p=.001, respectively); herb users were also significantly more likely than other users to say that they wanted a natural approach (OR=3.6, p=.001), or that use was consistent with their beliefs (OR=2.3, p=.021), or that they were familiar with such approaches from childhood (OR=2.0, p=.042).
Discussion
Because rates of use of complementary and alternative medicine are relatively high among people with depression (
18 ) and because rates of both use of complementary and alternative medicine and depression are relatively high among women (
19,
20,
24,
26,
28 ), a study such as this, elucidating patterns of use of these therapies among women with depression, is of importance for health professionals concerned with issues related to depression and use of complementary and alternative medicine.
Findings from our study support previous research showing high rates of use of complementary and alternative medicine among people with mood disorders in the United States (
14,
18 ). More than half of our sample of women with depression reported using complementary and alternative medicine in the year before the survey, highlighting the importance of studying patterns of use of complementary and alternative medicine in this population.
Several sociodemographic variables were found to be related to use of complementary and alternative medicine in our study. In our logistic regression analyses, African Americans were found to be significantly less likely than whites to use these therapies, employed women were significantly more likely to use these therapies than those who were not employed, and married women were significantly more likely to be users than those who were unmarried. Having a college education and being an immigrant were significant predictors of use of some types of complementary and alternative therapies. These findings are similar to those of a number of previous studies on use of complementary and alternative medicine in the general population (
15,
19,
20,
22,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30 ). However, a study by Kessler and colleagues (
18 )—which in some ways was more similar to ours than the studies cited above, because it focused on people with depression drawn from a community survey—did not find any sociodemographic factors to be significant predictors of use. That these factors emerged as significant in our study and not in the study by Kessler and colleagues may be related to the fact that our study sample was somewhat larger and had been oversampled for members of minority groups; our sample was also all female, and it may be that some of these associations hold more strongly for women than men.
Many of the previous studies that have examined the relationships between use of complementary and alternative medicine and sociodemographic factors have not generally differentiated between specific types of complementary and alternative therapies in their analyses (
19,
29,
36 ). Our study, in addition to looking at general use of complementary and alternative medicine, examined the relationships between sociodemographic factors and use of three particular types of such medicine.
Comparing these three types of complementary and alternative medicine yielded interesting findings. In terms of racial or ethnic differences, although the rate of any use was higher among non-Hispanic whites compared with African Americans and Mexican Americans, the highest rate of use of herbal medicines was found among Mexican Americans. This is similar to findings from a previous community study of residents of Florida (
23 ). Further analyses indicated that being an immigrant also contributed significantly to the use of herbal medicines. Our findings also suggest high use of complementary and alternative medicine among Chinese-American women, but because very few of the Chinese-American women in the original study reported being depressed, we did not have enough statistical power to form conclusions about this group. Educational level had a significant impact on use of certain types of complementary and alternative medicine—that is, herbs and vitamins but not manual therapies. Finally, perceived poor health was associated with use of manual therapies and herbs but not use of vitamin-based therapies.
Similar to previous studies (
16 ), our study found that many of the women with depression who used complementary and alternative therapies saw these therapies as congruent with their own values, beliefs, and philosophical orientations toward health and life. This was especially true for users of herbal medicines.
Our findings on reasons for use of complementary and alternative medicine among women with depression are of considerable importance for conventional mental health professionals and policy makers. For example, as found in other studies (
16,
19 ), the users in this sample very frequently cited dissatisfaction with conventional medical treatment as a reason for use of complementary and alternative medicine. About half of the users overall—and an even higher proportion of those using herb- and vitamin-based therapies—reported that the ineffectiveness or unpleasant side effects of a conventional medical treatment had been a motivating factor in their decisions.
Inability to afford conventional medical treatment was the least commonly cited reason for use of complementary and alternative medicine in our study, and recommendation by a physician was also a relatively uncommon reason. Our findings suggest, indirectly, that conventional medical doctors are somewhat likely to suggest the use of manual therapies to their patients with depression but are less likely to suggest using herbs and vitamins, indicating their greater familiarity with, or confidence in, manual therapies, compared with other complementary and alternative methods.
The role of the media in people's use of complementary and alternative medicine is also worth mentioning. More than 60% of the vitamin users and about half of the herb users cited having "read or heard something on TV or on radio that convinced me to use" a complementary or alternative therapy. Health information obtained from such sources may sometimes be helpful, but it may also be very unreliable or difficult for ordinary consumers to interpret (
37,
38 ). Clear communication between patients and health professionals would help ensure greater safety for patients, although it may be necessary for the clinician to approach the subject somewhat delicately. It seems self-evident that if a clinician is knowledgeable about the effectiveness or potential hazards of a particular complementary and alternative therapy, that knowledge should be shared with patients who are using or considering using those therapies. However, many of the folk remedies and other methods that are used have not yet been examined in scientifically reliable studies. If a patient is using remedies about which such scientific information is unavailable, it may be best for the clinician to take a neutral stance with regard to these remedies. Warnings offered by a clinician against the use of remedies derived from a patient's native or ancestral culture may backfire, because they may be interpreted as being disrespectful toward that culture.
Our findings on the differences between ethnic groups and the relatively high use of herbal medicines among immigrant women suggest that physicians and other health care professionals working with immigrant populations would do well to acquire basic knowledge about the particular health care traditions of the nations or regions from which their patients originate.
The study presented here was limited by the fact that the questionnaire used in the original study did not include a diagnostic instrument for assessing depression. Instead, it simply asked whether respondents had been medically diagnosed with depression. Thus it is likely that some of the respondents from the original study had depression in the past year, but they were not included in our sample because they had never technically been diagnosed as such. Future studies using psychiatric assessment tools will help us to better understand the use of these therapies not only as supplements to conventional mental health and medical treatments but also as alternatives.
Because our analyses were based on survey data and on participants' reports of complementary and alternative medicine for any health condition, rather than for depression specifically, they cannot provide information pertinent to assessing the efficacy of any particular complementary and alternative therapy for treating depression. Further research in this important area is needed.