In late October and early November of 2003 wildfires ravaged large sections of Southern California. Burning an area roughly the size of Rhode Island and destroying more than 3,700 homes, the California firestorms were one of the most expensive natural disasters in state history. An estimated 100,000 persons faced mandatory emergency evacuation under harrowing circumstances (
1 ). Although a cataclysmic event for California, these firestorms are not isolated occurrences. From 2002 to 2004, for example, wildland-urban interface fires destroyed more than 9,000 structures (
2 ). Moreover, mass exposure to wildfires has become an increasingly common public health problem, because millions of residents have moved into the wildland-urban interface areas that were formerly wilderness (
3 ). By one estimate, nearly 40% of new home construction in the Western United States occurs in or adjacent to the wildland-urban interface (
4 ).
Despite its emerging importance, little relevant research has addressed the mental health consequences of exposure to wildland-urban interface fires. The scientific literature on adjustment to wildfire disasters has focused primarily on firefighters and rescue workers (
5,
6,
7,
8,
9,
10 ). Although these studies elucidate factors associated with mental health consequences of occupational exposure for professional emergency service providers, the relevance of these data for ordinary community-dwelling survivors of wildfire disaster is unclear. A few investigations have examined the impact of fire disasters in the wildland-urban interface on the exposed public (
11,
12,
13 ). However, this research has not studied disaster survivors until weeks or months after fire exposure, thus limiting the value of these investigations for public health emergency planning. Similarly, these studies have not attempted to assess the prevalence of trauma-related psychopathology among survivors of wildland-urban interface fires.
Effective public health planning for fire disasters in the wildland-urban interface requires collecting basic information about the mental health consequences of exposure to fire in these areas during or immediately after the disaster. In particular, it is essential to understand the mental health needs of persons who are affected by fire disasters in the wildland-urban interface to such a degree that they seek disaster-related assistance at government aid agencies or the American Red Cross. Recognizing their needs is critical for at least two reasons. Persons who seek disaster-related services are likely to include many persons most affected by the fires as well as those who have fewer resources than their counterparts who do not seek aid, thus increasing their vulnerability to psychopathology. In addition, from a pragmatic standpoint, disaster-assistance centers appear to be a logical location for identification, triage, and preventive treatment for persons at high risk of fire-related psychopathology.
At this juncture in the development of public health planning for fire disasters in the wildland-urban interface it would be useful to estimate the prevalence of trauma-related psychopathology in settings that provide disaster relief services to the affected community. Moreover, because large numbers of people seek such services from these agencies, any effective prevention or intervention strategy would benefit from an easily administered short screener for early identification of persons at elevated risk of trauma-related psychopathology. Although many people may experience symptoms of distress in the hours and days after trauma exposure, most individuals will recover without intervention (
14,
15,
16 ). Therefore, an efficient public health response during or immediately after a disaster may be to screen for individuals who are at elevated risk of future psychopathology, rather than for persons who are experiencing high levels of current distress.
The goals of the study presented here were twofold: to estimate the prevalence of two commonly occurring posttraumatic psychiatric disorders (major depression and posttraumatic stress disorder [PTSD]) among individuals who had sought disaster services or shelter as a result of a wildland-urban interface fire three months previously and to evaluate whether a short, easy-to-use, and relatively nonintrusive screener—administered within hours or days of the disaster—might aid in identification of persons at elevated risk of subsequent posttraumatic psychopathology.
Methods
Participants
A total of 357 individuals who were subjected to mandatory evacuation in response to the California wildfires in October 2003 participated in this study. Study participants were recruited from two adjacent facilities that provided emergency disaster services: an American Red Cross center offering temporary shelter and other assistance (N=224) and a government assistance center housing federal, state, and county aid agencies (N=133).
Sampling and procedures
All adults in or leaving the two recruitment sites between the hours of 10 a.m. and 6 p.m. over the course of several days were invited to participate by a member of the research team. Staff members fully explained study procedures, answered questions, obtained written informed consent, and distributed and collected self-administered questionnaires. The research protocol was reviewed and approved by the RAND Institutional Review Board. A single, randomly selected adult from each household was invited to complete the survey. Of the 402 households approached to participate, 357 persons completed the questionnaire, yielding a baseline response rate of 89%. Insufficient information about initial nonrespondents was available to assess whether nonrespondents differed from respondents at baseline, although the low level of nonresponse limits the potential bias.
At follow-up, a multistep procedure was followed to recontact participants: questionnaires were mailed to the last known address as well as to the addresses of friends and family provided by the respondent, phone calls were made to participants whose questionnaires were returned as undeliverable, and Internet search services were used to obtain updated contact information. Both the initial and follow-up questionnaires, which were written in English, took approximately 15 to 20 minutes to complete.
Of the 357 participants at baseline, 234 (66%) returned a completed three-month follow-up survey through the mail. To adjust for the effects of study attrition, a logistic regression model was built to assess differences between participants who completed the follow-up survey and those who did not. We considered demographic characteristics, degree of fire exposure, exposure to prior traumatic events, initial reactions, and measures of social support as candidate predictors of attrition. Variables associated with nonresponse with bivariate p values of less than .20 were included in the multivariate logistic regression model. This model was used to generate inverse-probability attrition weights employed in all analyses that predicted follow-up outcomes from baseline measures. All weighted analyses incorporated the variance inflation attributable to the use of weights.
Measures
Demographic information. Participants provided information about their gender, age, marital status, race or ethnicity, household income, work status, and education.
Objective severity of fire exposure. Items using a response format of "yes," "no," and "don't know" measured severity of fire exposure. In selecting items, we drew upon other questionnaires on fire exposure (
12 ) and included items such as whether the respondents' house was damaged or destroyed by the fire, whether they were able to see the flames of the fire from their home or neighborhood, whether they had difficulty breathing because of smoke or ashes, and whether they were physically injured because of the fires. Respondents were also asked to indicate whether they had stayed at a temporary shelter at any time since the fires started. In the reported analyses, we combined the "no" and "don't know" response options into one category.
Initial reactions. A series of items using a "yes, very much," "yes, a little," and "no, not at all" response format assessed the extent to which participants had experienced fear for their life, fear for the life of a loved one, fear that their home or property was in danger, feeling helpless, and feeling terrified. Items were modeled after a survey by Brewin and colleagues (
17 ). For the purpose of the analyses reported here, we created dichotomous yes and no variables by combining the "yes, very much" and "yes, a little" response options.
Posttraumatic stress symptom severity. The Posttraumatic Symptom Checklist (PCL) was used as a screener to assess probable PTSD at the three-month follow-up (
18 ). This instrument contains 17 symptom items keyed directly to the
DSM-IV (
19 ). By using a time frame of the past two weeks, respondents answered each item with respect to the fire on a 5-point scale reflecting symptom severity. The scale was used to derive a probable diagnosis of PTSD following guidelines provided by Weathers and colleagues (
18 ). Specifically, the PCL was scored by using the
DSM-IV symptom cluster algorithm, and symptoms were counted as present if they were rated as moderately, quite a bit, or extremely bothersome to the respondent. The PCL has been used in various traumatized populations and has been found to possess solid psychometric properties and construct validity in diverse samples (
20,
21,
22 ).
Depressive symptoms. Depressive symptoms were assessed at follow-up by using the eight-item version (PHQ-8) of the nine-item Patient Health Questionnaire (PHQ-9) (
23,
24 ). The PHQ-9 is well validated and widely used as a brief screening measure for major depression (
24 ). The PHQ-8 consists of the criteria on which a
DSM-IV diagnosis of major depression is based, excluding suicidality, and can be used as a screener to determine a probable diagnosis of major depressive disorder. Responses are provided with respect to the frequency with which symptoms were experienced in the past two weeks, by using a 4-point scale ranging from 1, not at all, to 4, every day. Persons with summed scores greater than 9 were classified as being depressed (
23 ).
Statistical analysis
The mean and standard deviation of age were calculated for baseline respondents. For all other baseline demographic characteristics and fire exposure measures, proportions and their 95% margins of error were calculated. The prevalence and comorbidity of probable PTSD and major depression at the three-month follow-up were calculated by using attrition weights, as were the corresponding 95% confidence intervals.
Logistic regression was used to calculate bivariate odds ratios for the association between baseline measures of fire exposure and the presence of either probable PTSD or major depression at the three-month follow-up. In addition, adjusted odds ratios for each fire exposure measure were derived from logistic regressions that controlled for age, gender, race or ethnicity, education, employment status, and income.
For predictive purposes, we used best-subsets regression to identify fire exposure and subjective reaction measures that were statistically significant predictors of psychopathology. This method involves assessing all models created from all possible combinations of predictor variables, using R 2 as the criterion to determine best fit. We first examined all possible two-item combinations and then proceeded to examine additional items for their contribution to improved fit. We evaluated alternative scoring rules for the selected items and calculated the positive and negative predictive values of the resulting scores.
Results
Characteristics of the baseline sample
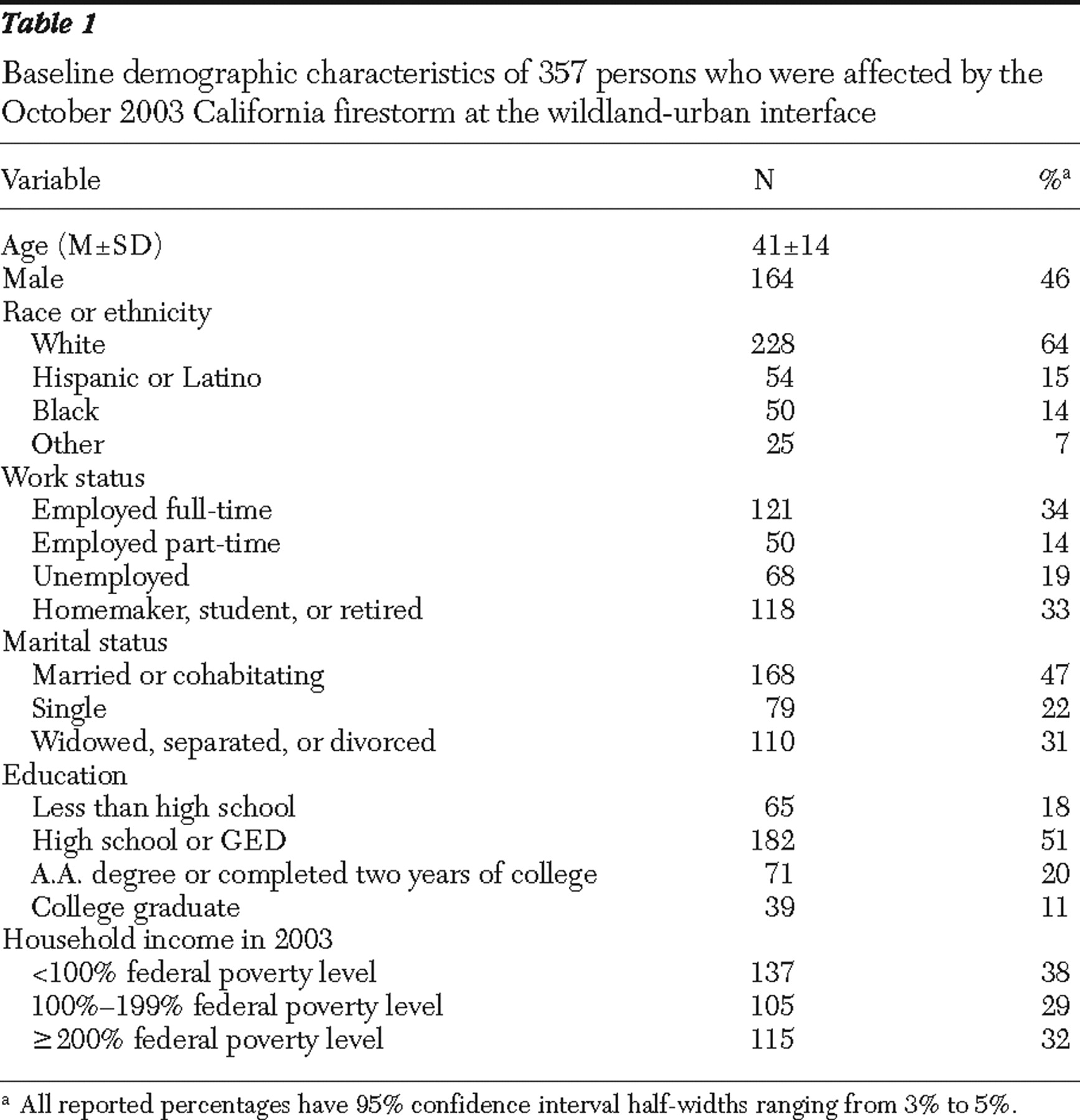
The demographic characteristics of our baseline sample are displayed in
Table 1 . Our sample included approximately equal numbers of men and women, individuals who were married or cohabitating and those who were single, and persons who were employed and those who were not. Thirty-eight percent of the sample had annual household incomes below the federal poverty level.
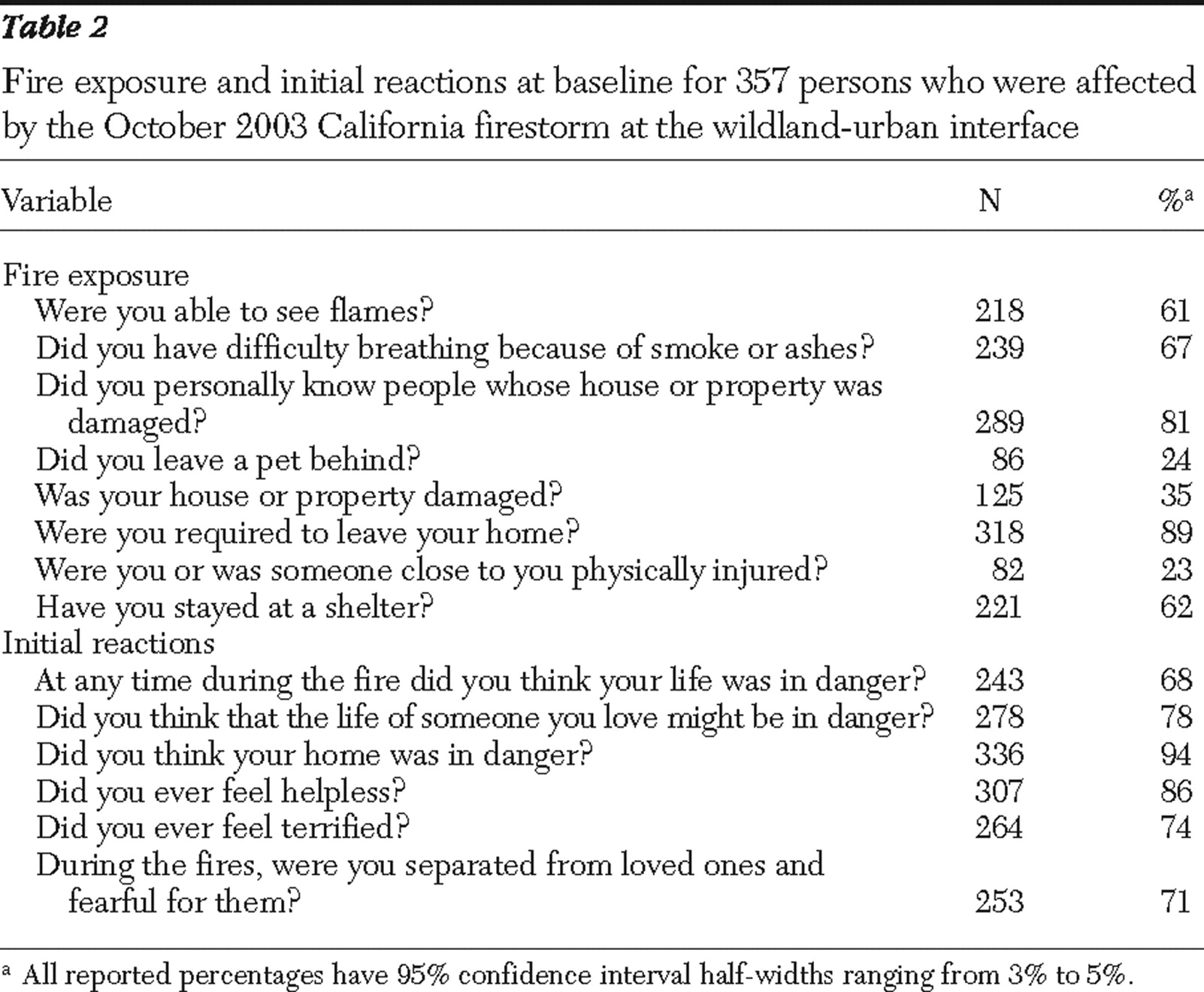
Participants reported high levels of fire exposure (
Table 2 ). Participants' responses to items inquiring about initial reactions to the fires revealed that more than two-thirds of participants experienced fear for their well-being or that of a loved one. Ninety-four percent indicated that they had feared that their home was in danger.
Results of the attrition model
Fifteen measures were retained for the multivariate model predicting attrition: three demographic characteristics (age, gender, and marital status), nine measures of fire exposure, a prior traumatic events exposure count, a social support scale, and a scale of initial reactions to the fire. The overall attrition model was statistically significant, ( χ 2 =32.44, df=15, p=.006) and predicted attrition reasonably well (concordance=.67). Participants lost to follow up were younger and had more severe fire exposure.
Prevalence and comorbid psychopathology at follow-up
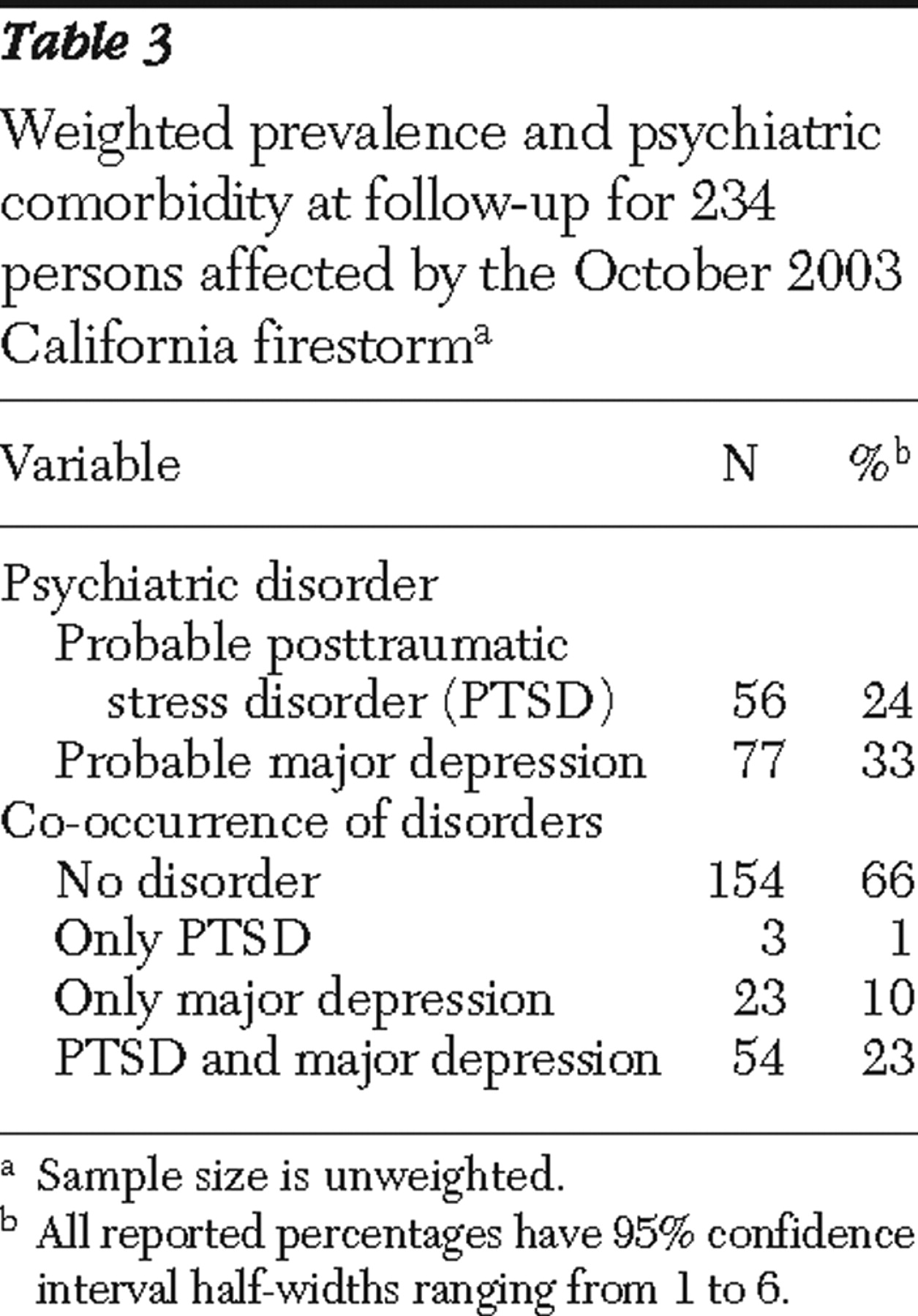
As shown in
Table 3, participants reported significant levels of psychopathology three months after the fires, as reflected by the percentages of people meeting probable diagnoses for PTSD or major depression. Furthermore, the co-occurrence of probable depression and PTSD was striking (
Φ =.74, p<.001).
Because of the high co-occurrence of probable major depression and PTSD, as well as preliminary analyses that showed a similar pattern of associations involving probable depression and PTSD with baseline predictors, we focused subsequent analyses on the dichotomous outcome variable, PTSD or depression. This index reflected whether a participant met criteria for either disorder at follow-up.
Predictors of psychopathology at follow-up
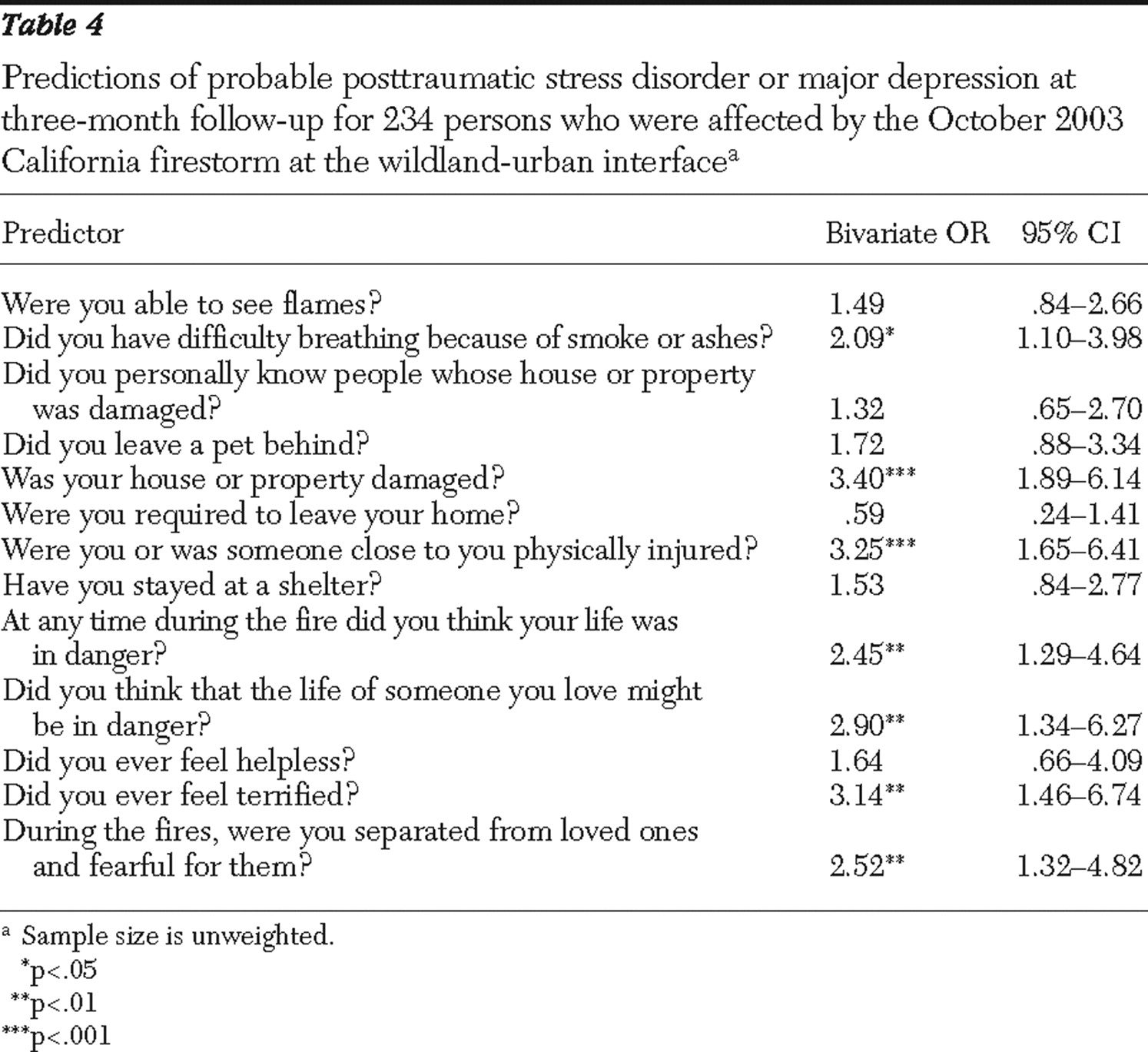
The bivariate associations between demographic factors and the dichotomous index reflecting the probable presence of either PTSD or depression at follow up were small; none were statistically significant at the p<.05 level. As displayed in
Table 4, however, several measures of participants' fire exposure and initial reactions to the fire showed significant bivariate associations with psychopathology at follow-up. Difficulty breathing because of smoke or ashes, house or property damage, and physical injury to the respondent or a loved one were predictive of a probable diagnosis. In terms of participants' initial reactions to the fire, fear that one's own life was in danger, fear that the life of a loved one was in danger, feeling terrified, and being separated from loved ones and being fearful for them increased the risk of psychopathology at follow-up. Demographically adjusted multivariate analyses revealed odds ratios and levels of statistical significance that were virtually identical to unadjusted results. Only the association between "difficulty breathing because of smoke or ashes" and any psychopathology was no longer significant after the analysis adjusted for demographic characteristics.
Best-subset regression revealed a two-item model predicting any psychopathology. These items were house or property damage and physical injury to oneself or a loved one ( χ 2 =27.76, df=2, p<.001). No additional items provided a significant incremental improvement in prediction. This two-item index displayed adequate properties for use as a screener for future psychopathology. Of the 49% of our sample who endorsed at least one of these items at baseline, 47% had a probable disorder at follow-up (71% sensitivity, 63% specificity, 47% positive predictive value, and 81% negative predictive value). Of the 11% who endorsed both items, 69% had a probable disorder (22% sensitivity, 95% specificity, 69% positive predictive value, and 70% negative predictive value). Finally, among those who endorsed neither risk factor, 19% had a probable disorder at follow-up.
Discussion
Fires in the wildland-urban interface constitute a growing public health problem, particularly in the Western United States (
3 ). The toll on public mental health and suffering exacted by these fires has not, however, attracted commensurate attention. This study examined issues relevant to the mental health needs of persons seeking disaster aid after exposure to these fires.
The first goal was to estimate the prevalence of common trauma-related psychopathology in a disaster relief-seeking sample in the weeks after fire exposure. We found high levels of probable PTSD and major depression, with 34% of participants meeting screening criteria for at least one of the disorders three months after the fire. Moreover, considerable comorbidity was observed for the two conditions, with nearly one-quarter of our sample meeting screening criteria for both disorders at follow-up. A growing body of research now recognizes the frequent comorbidity of PTSD and depression (
25,
26,
27 ). Indeed, some research has suggested that PTSD and depression may reflect a common vulnerability to experience posttraumatic distress (
25 ). The rate of co-occurrence in the study presented here appears somewhat higher than that found in other studies. Insofar as no other research has examined this issue in a fire-exposed sample, additional research is needed.
With respect to our second objective, we identified two items that possessed good ability to identify persons who subsequently met criteria for probable PTSD or major depression. Composed of unobtrusive questions about property damage and physical injury to oneself or a loved one, these items could serve as a potential screener to provide an easy-to-administer, relatively nonintrusive tool to triage persons at elevated risk of subsequent postdisaster psychopathology after fires occurring at the wildland-urban interface. Two possible cutoff points for this screener were evaluated. The more lenient scoring algorithm did a better job of balancing sensitivity with specificity. In view of the large number of persons affected in a mass disaster and limited mental health resources, however, the higher cutoff point (that is, requiring "yes" answers to both screening questions) may possess greater utility. Additional research is needed to determine the value of these items for use as a screener in other samples exposed to fire at the wildland-urban interface.
Early identification of at-risk disaster survivors is a widely recognized, but elusive, goal. A recent review of more than 160 early postdisaster intervention programs has concluded that early intervention for trauma survivors is important (
15 ). These authors also observed that early identification poses a very significant challenge (
28 ). To the degree that our findings are generalizable to survivors of other wildland-urban interface fires, this brief screener may provide information needed to efficiently allocate scarce mental health resources after this type of disaster. No other tools are currently available to triage disaster-exposed adults at risk of future psychopathology.
These data should not be taken as evidence that these items would be appropriate for use as predictors of postdisaster psychopathology in other contexts. At the same time, the transparent nature and seeming relevance of these two items (that is, "property damage" and "physical injury to oneself or a loved one") to various natural and human-caused mass disasters suggest that these items might have predictive utility in other settings. At the very least these data point toward a potentially promising avenue of research aimed at identifying brief screeners for early identification of persons at elevated risk of trauma-related psychopathology.
In interpreting our findings, one should be mindful of certain limitations. Perhaps most important, this research was not intended to directly assess a representative sample of all persons affected by the California wildfires. We deliberately chose to sample at a location that naturally congregates individuals who are most likely to benefit from mental health services, thereby addressing critical policy questions about the feasibility and need of postdisaster mental health services. Moreover, we employed diagnostic screeners rather than full diagnostic instruments. Thus our prevalence rates might overestimate the actual numbers of individuals who would meet full criteria for PTSD or major depression at follow-up. In particular, screeners do not adequately measure all criteria required for an actual diagnosis—for example, functional impairment.
In addition, rates of major depression in this sample at follow-up substantially exceed past-12-month prevalence rates in a nationally representative sample, suggesting fire exposure as a proximate cause (
29 ). Nonetheless, the possibility remains that some persons had been experiencing an episode of major depression either before the fire or for reasons entirely unrelated to the disaster. Thus our estimates of the relationship between fire exposure and major depression may also be somewhat inflated. Finally, although a three-month follow-up period seems reasonable for purposes of identifying individuals who might benefit from treatment, additional research might fruitfully examine survivors over an even longer period.
Conclusions
These findings document that individuals seeking disaster relief after wildland-urban interface fires are at heightened risk of subsequent psychopathology. Emergency relief centers constitute not only convenient locations for mental health triage but also important sites for such services. Moreover, early identification of individuals at risk of future psychopathology in these settings seems to be feasible by using easily administered, relatively nonintrusive questions about objective fire exposure. Finally, the generic nature of the items that emerged as the best set of predictors of posttraumatic psychopathology raises the possibility of their utility in other trauma contexts, although this prospect awaits further study.
Acknowledgments and disclosures
This research was supported by grant R01-MH-056122 from the National Institute of Mental Health and the RAND Corporation. The authors thank the RAND Survey Research Group for their assistance with data collection and Annie Zhou, M.S., for her help with data analysis. The authors also acknowledge H. Frank Chew, Ph.D., for his assistance with data collection logistics. The authors are indebted to the study participants. The views expressed in this article are those of the authors and do not necessarily reflect the opinions of the National Institute of Mental Health or the RAND Corporation.
The authors report no competing interests.