Over the past decade a series of reports and campaigns on mental health have put stigma at the forefront of mental health concerns (
1,
2,
3,
4,
5,
6 ). Stigma is "a chief enemy" (
7 ), the "most formidable obstacle" (
1 ), and a "perpetual impediment" (
3 ). For children, stigma and the "culture of suspicion" (
3 ) it creates are credited as fundamental reasons for the continued, pervasive level of unaddressed mental health needs (
8 ).
Partly fueling concerns for children's mental health treatment is the dramatic rise in the use of psychiatric medications over the past three decades in the United States (
9,
10,
11,
12 ). Although actual rates are contested (
13,
14,
15,
16 ), a long-term increase in the use of psychostimulants began in the early 1970s. Between 1990 and 1995 prescriptions more than doubled among children of ages five to 18 (
11 ) and tripled among preschoolers (
17,
18 ), and prescriptions continued to grow significantly through 2003 (
19 ). This shift toward medication-based outpatient treatment holds for state-funded and privately insured programs and has been coupled with a striking increase in medication expenditures for children (
19,
20 ). Although some researchers claim little evidence of overprescription, others contend that current practices signal a problem for children and families (
18,
21 ).
The general stigma attached to mental health treatment and specific concerns about the use of psychiatric medications for children challenge clinicians' efforts to provide appropriate and effective treatment to children and adolescents. As Jensen (
22 ) pointed out, services cannot be effective for families concerned about stigma because these families are unlikely to access available resources or accept recommended treatment options. As modified labeling theory argues, the perceptions, beliefs, and attitudes that compose the larger cultural context can be as powerful as the actual existence of prejudice and discrimination (
23 ). Both shape individuals' responses to the onset of mental health problems as well as the advice individuals receive regarding recognition, treatment, and recovery (
24 ).
By using the National Stigma Study-Children (NSS-C), we focused on four general stigma concerns: a child's "outsider" status, later ramifications, confidentiality, and parent self-blame. We also targeted four concerns about psychiatric medications: overmedication, long-term effects, medicating "real" problems (that is, behavior problems), and personality blunting. Finally, because of the lack of previous research on stigma attached to children's mental health problems and treatment, we asked whether stigmatizing attitudes are widespread or located in specific, traditional, subcultural groups thought to hold more conservative values and views. That is, we drew from past studies to examine whether respondents' characteristics (gender, race, age, and education) are associated with their perceptions of stigma for children. Past research has suggested that white and younger individuals, women, those with more education, those who live in urban areas or outside of the South, and those who are affiliated with more liberal religions are more tolerant of difference, in general, and sometimes more tolerant of stigma. Research specifically focused on mental illness has also suggested that individuals who have had previous contact with persons with mental illness tend to report less stigma (
25,
26,
27,
28,
29,
30 ). In addition, because of the special case of children, we also considered the potential influence of marital and parental status on perceptions of stigma and reactions to mental health problems among children and adolescents (
10 ). Finally, trust in physicians and evaluations of the efficacy of psychiatric medication have been found to be important in acceptance of psychiatric medications (
31 ).
Methods
Sample
Data came from the NSS-C module of the 2002 General Social Survey, a nationally representative sample described in the introduction to this special section (
32 ). The sample used in this analysis was self-weighting. Institutional review board approval for the General Social Survey was provided by the University of Chicago, and approval for secondary data analysis was given by Indiana University. Per standard protocol for in-person surveys, oral informed consent was secured at the time of the interviews.
Taking into account missing values for both the dependent and independent variables considered here, the target sample was reduced from 1,393 to 1,062 but did not differ in overall profile from the full sample. About one-fifth of this subsample (231, or 22%) were from racial or ethnic minority groups: 156 were African American (15%), 31 were Hispanic (3%), 29 were Asian or Pacific Islander (3%), 14 were American Indian or Alaskan Native (1%), and one was from another group. Respondents ranged from 18 to 89 years old, and more than half were female (606 women, or 57%). More than half attended at least one year of college or vocational school (605, or 57%), about half worked full-time (542, or 51%), slightly less than half were married at the time of the study (514, or 48%), and more than two-thirds were parents (755, or 71%).
Dependent variables
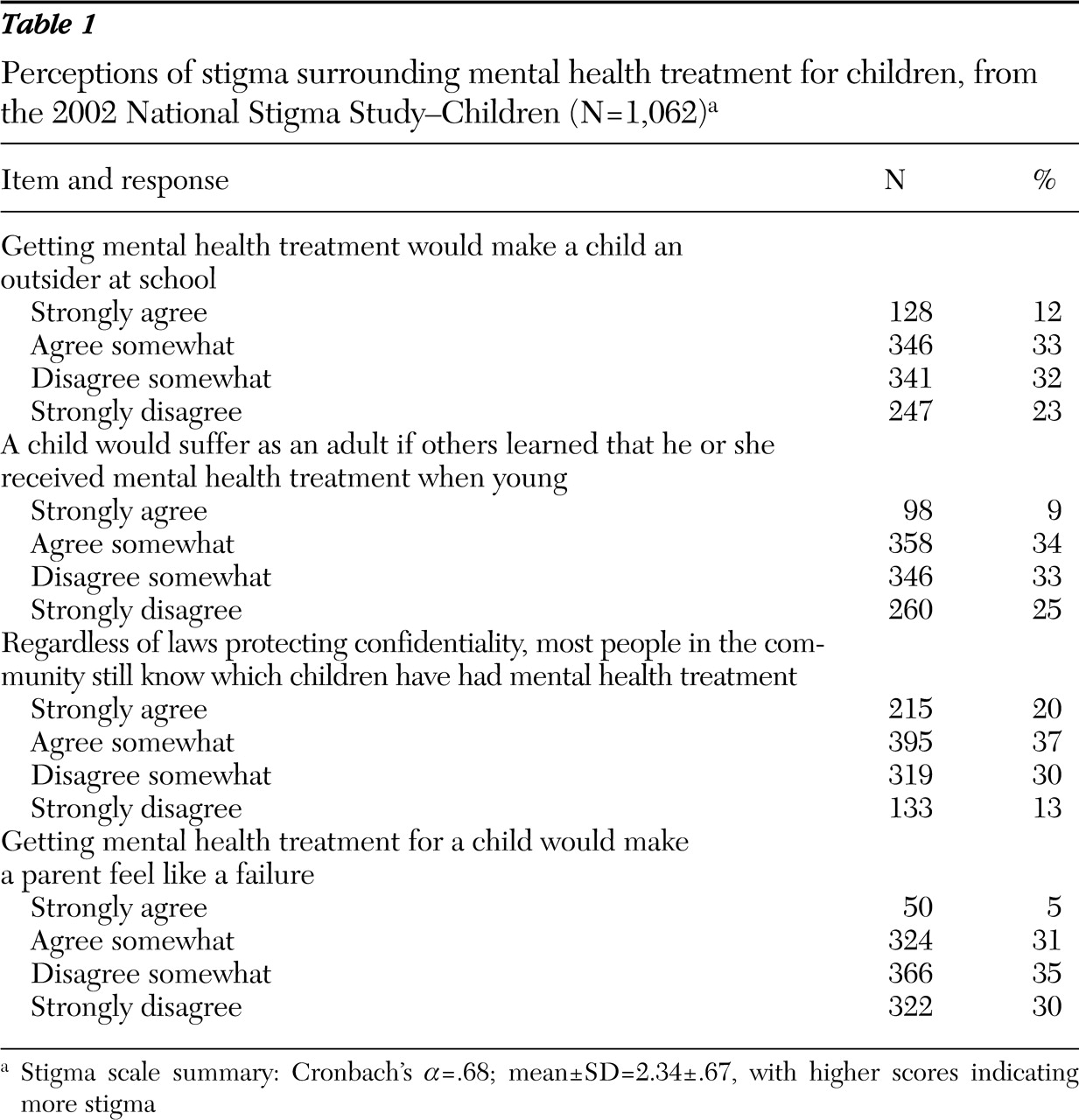
Four items measured perceptions of stigma associated with mental health treatment (
Table 1 ). Response categories were strongly agree, agree somewhat, disagree somewhat, and strongly disagree. Items were recoded from 1 to 4, with higher values indicating more stigma. For the multivariate analyses, items were combined into a cumulative, ordinal scale measuring perceptions of stigma surrounding mental health treatment for children. Items were summed, and the total was divided by the number of items, which ranged from one to four (mean±SD=2.34±.67; Cronbach's
α =.68).
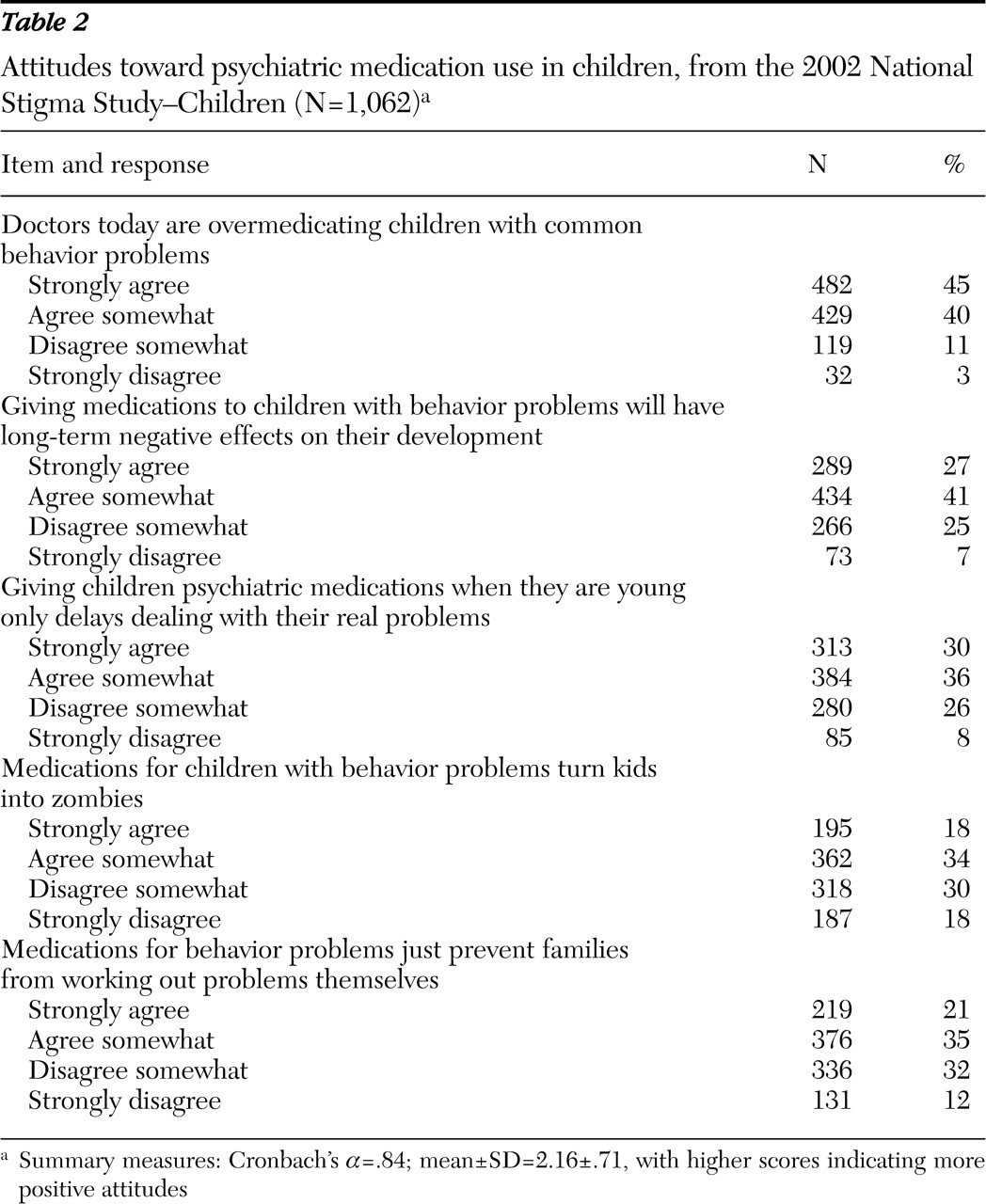
Five questions about psychiatric medication use for children targeted overmedication, long-term negative effects, medicating real individual and family problems, and personality blunting (see
Table 2 for item wording). Response categories were coded from strongly agree (coded 1) to strongly disagree (coded 4) and were recoded with higher values indicating more negative attitudes toward psychiatric medications. The five individual items were also combined into an ordinal scale, attitudes toward psychiatric medication use among children, expressed as the mean of up to four component items for each individual (mean 2.16±.71; Cronbach's
α =.84). For both scales, there were no major differences in correlates when items were analyzed separately. No other psychometric properties have been established.
Independent variables
Respondents' age and years of schooling were measured in years. Binary variables were included for gender (female, 1; male, 0), race (African American, 1; others, 0), employment status (works full-time, 1; works part-time or not at all, 0), marital status (married, 1; otherwise, 0), parental status (a parent, 1; not a parent, 0), religious affiliation (liberal religion, such as Episcopalian or Unitarian, 1; moderate or conservative religion, such as Southern Baptist or Seventh-Day Adventist, 0). A variable asking how often respondents attend religious services (recoded from nine ordinal categories to days per year) was also included. Binary variables for the South (coded 1; otherwise, coded 0) and rural residence (coded 1; otherwise, coded 0) were included.
Trust in physicians was measured as a five-item scale. Individual items such as "I trust my doctor's judgments about my medical care" and "I doubt my doctor really cares about me as a person" were originally coded strongly agree (coded 5) to strongly disagree (coded 1). Up to five items were coded or recoded and were summed as described above, with higher values indicating more trust (mean 4.10±.79; Cronbach's α =.80). Evaluated efficacy of psychiatric medications was measured as a four-item scale; individual items included "These medications help people control their symptoms" and "These medications often have unacceptable side effects" (mean 2.55±.51; Cronbach's α =.54).
Contact with people with mental health problems was measured with three binary variables. Two indicated whether the respondent knew someone who had received mental health treatment, who had been in a psychiatric hospital, or both. Previous analyses of these variables in research and our preliminary analyses indicated that there is considerable overlap of these contact variables and that a broader, combined variable eliminated the confounding influence of historically bound treatment modalities. The third binary variable tapped the influence of mental health problems: the response was coded 1 if the problems caused the relationship to become worse or to end (14%) and coded 0 if they made the relationship stronger, had no effect, or if the respondent had no contact. Unfortunately, an error in the sequencing of questions, coupled with a small number of nonresponses, reduced the subsample to 734 participants for this part of the analysis.
Analyses
We report frequency distributions for items that compose the stigma scales for mental health treatment and psychiatric medications. Ordinary least-squares regression models were used to estimate the influence of the correlates of respondent characteristics with stigmatizing attitudes. Given the skip-pattern error noted above, the ordinary least-squares specification for respondents who had data on the attention-deficit hyperactivity disorder issues was reestimated to assess potential bias. Because there was little difference in the results, we present only the findings with the contact variables included (details on request). A significance level of .05 and two-tailed tests were used in all analyses.
Results
Stigma associated with treatment
Almost half of the sample agreed somewhat (346 respondents, or 33%) or strongly (128 respondents, or 12%) that receiving mental health treatment would make a child an outsider at school and suffer as an adult (
Table 1 ). More were skeptical about confidentiality, with over half reporting that people in the community knew, despite confidentiality protections, which children had been or were currently in treatment (610 respondents, or 57%). However, fewer (about one-third; 374 respondents, or 36%) agreed that getting mental health treatment for a child would make the parent feel like a failure.
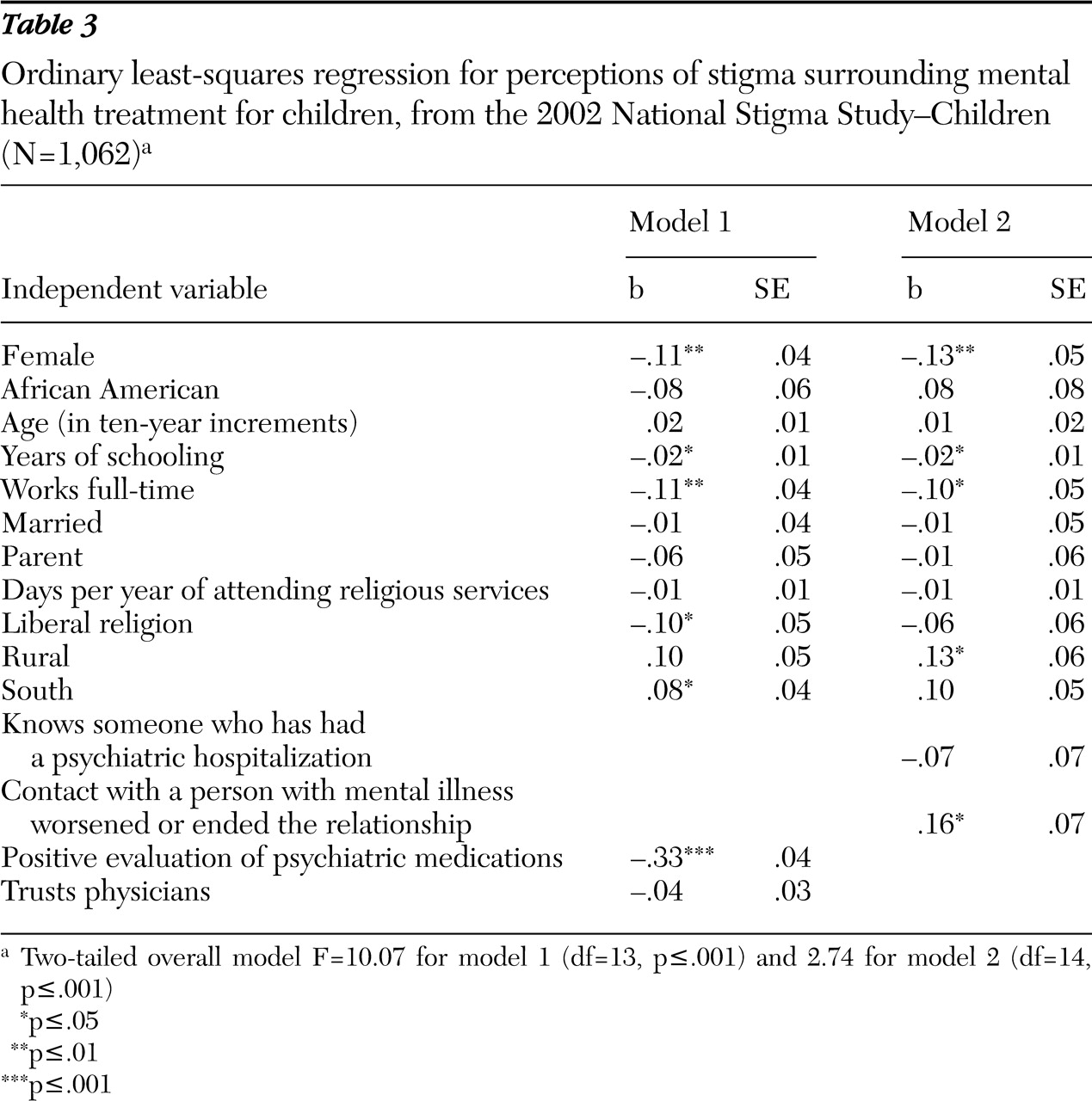
Estimates of the correlates of treatment-based stigma (
Table 3 ) suggest that women perceived less stigma than men (model 1). More educated respondents, full-time workers, and individuals who belonged to a liberal religion were significantly less likely to see treatment as stigmatizing. Also, individuals with more positive perceptions of the efficacy of psychiatric medication perceived less stigma attached to mental health treatment for children. Being married or a parent had no effect. Individuals in the South were more likely to see treatment as stigmatizing.
Model 2 used the reduced subsample. In analyses not presented in this article, a replication of model 1 showed that most effects remained the same in direction and magnitude, although the effects of living in the South and belonging to a liberal religion became nonsignificant. Model 2 results indicated that knowing someone who has seen a mental health professional or who has had a psychiatric hospitalization did not shape perceptions of stigma surrounding children's mental health treatment. However, the nature of the contact with that person did. Respondents who experienced deterioration or termination of a relationship because of another person's mental health problem were significantly more likely to perceive stigma associated with treatment for childhood mental health problems.
Attitudes toward psychiatric medications for children
Most respondents strongly agreed (482 respondents, or 45%) or agreed somewhat (429 respondents, or 40%) that physicians overmedicate children with common behavior problems (
Table 2 ). Most also agreed that giving medications to children with behavior problems has long-term negative, developmental effects (723 respondents, or 68%). Well over half (697 respondents, or 66%) reported that giving children psychiatric medications when they are young only delays dealing with their real problems. Finally, over half agreed that medications for children with behavior problems blunt their personalities (turn children into "zombies") and prevent families from working out problems (557 and 595 respondents, or 52% and 56%, respectively).
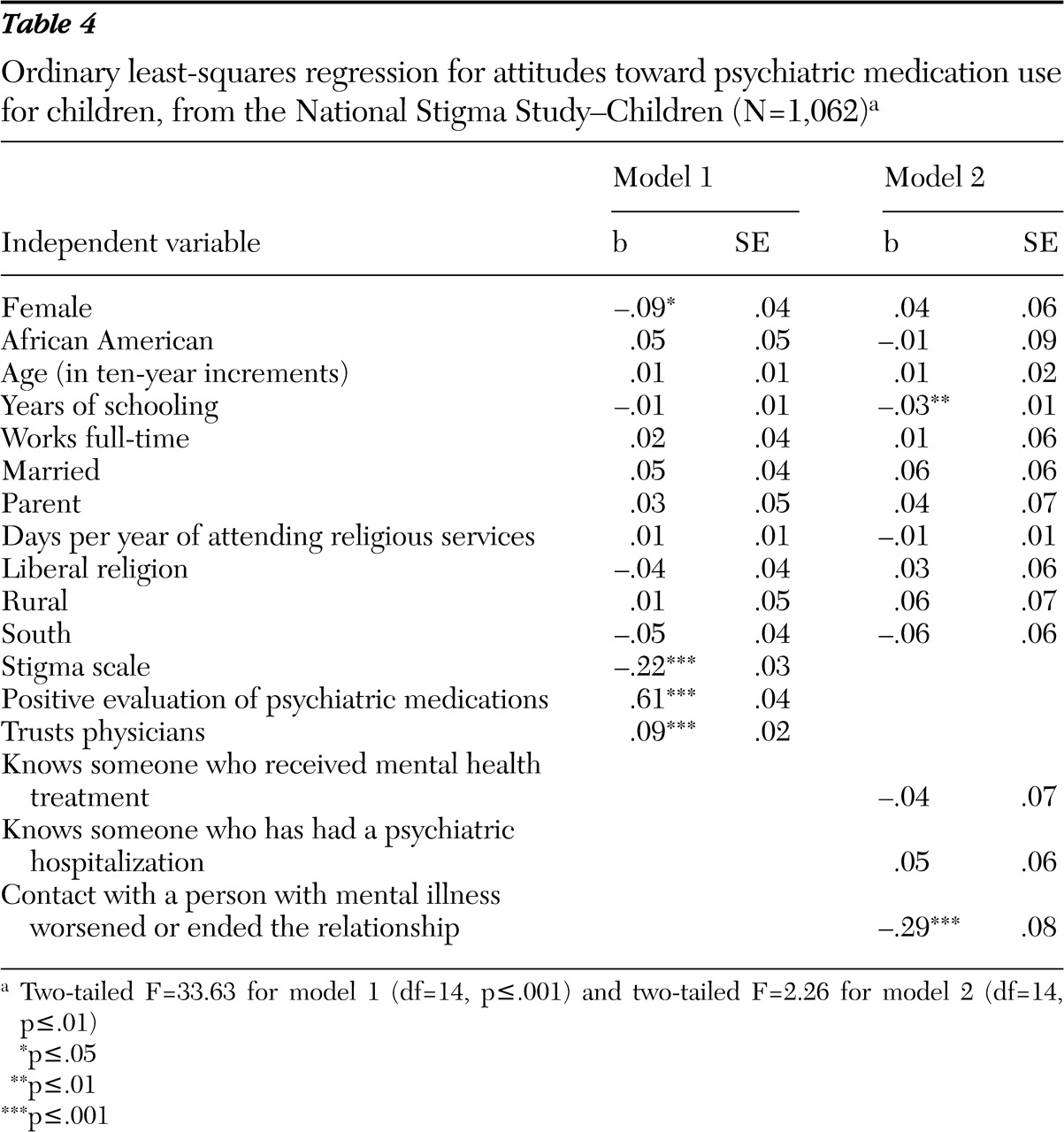
As shown in
Table 4, only women emerged as significantly less likely to hold more positive attitudes than other subgroups. However, other relevant attitudes significantly affected attitudes toward psychiatric medication use for children. Specifically, individuals who perceived more stigma attached to mental health treatment were less likely to support psychiatric medication use for children, whereas those who had more trust in physicians had more favorable attitudes. Furthermore, having more positive attitudes toward psychiatric medication generally was associated with support for medications for children. Finally, in results not presented here, the absence of effects of sociodemographic characteristics held regardless of additional attitudes included in the specification. Only education was associated with more positive attitudes, and the effect disappeared once other attitudes were considered (details on request).
The results of model 2, which included contact variables, suggested that knowing someone who has received treatment does not significantly predict support for psychiatric medication use for children. However, the nature of that contact matters. Respondents who had negative experiences were significantly less likely to support psychiatric medications for childhood mental health problems.
Discussion
Given the resurgence in interest and concern about stigma (
31,
32,
33 ), what is most surprising is the near absence of stigma research on children and adolescents. Here we bring national data to bear on the debate about stigma surrounding children's mental health treatment generally and one treatment more specifically—psychiatric medications.
The overall cultural climate for recognizing and accessing treatment for children and adolescents is bifurcated, with the sample almost evenly split in their opinions about the stigmatizing effects of mental health treatment. Further, stigma remains an important barrier for many cultural subgroups, including those who traditionally have been underutilizers of mental health treatment. Men, persons with lower levels of education, those who live in rural areas or in the South, those from moderate or conservative religions, and those whose contact with persons with mental illness has led to bad relational outcomes all perceived that more stigma will be aimed at children who receive mental health services. Surprisingly, race had no influence.
More important, many participants reported stigmatizing attitudes regarding the use of psychiatric medication for children. Most respondents believed that children are being overmedicated, that these medications have long-term negative developmental impact, that they turn children into "zombies," and that they get in the way of "real" solutions to the child's behavior problems. Unlike the cultural climate surrounding treatment, sociodemographic characteristics of respondents had little influence on attitudes toward using psychiatric medications for children. The only subgroup reporting more negative attitudes toward psychiatric mediations was women. However, those who perceived stigma resulting from treatment or who reported a negative relational experience with persons with mental illness did the same. On the other hand, trust in medical providers and seeing psychiatric medications as efficacious can counter these cultural prejudices.
This study had three limitations. First, our analyses targeted the perception of stigma. They did not indicate which respondents were more likely to discriminate against children with mental health problems. Yet, as modified labeling theory argues, the existence of perceptions of stigma alone may be enough to prevent parents or caregivers from recognizing mental health problems and seeking treatment for their children (
23 ). Second, this first national study targeted at children's mental health problems asked individuals to respond to the general idea of "children with mental health problems." Research on mental illness in adulthood has moved past this point, finding important differences in societal responses to depression, schizophrenia, and addiction problems (
27 ). Finally, the results for the stigma and medication items included on the NSS-C were all in the negative direction. Positive assessments, also likely to be critical in recognition and service use, may modify the effects presented here. All of these limitations suggest important areas for future research.
Conclusions
The results of the first nationally representative survey on child and adolescent mental health support concerns about stigma as a barrier to care and provide even stronger evidence that apprehension about medication treatment strategies will confront mental health service providers. These findings are consistent with work by Pappadopulos and colleagues (
34 ), which indicated that more parents preferred school-based services and counseling for behavioral problems, even though such services were typically unavailable. Thus individuals are most reluctant to use the treatment options that are most available and most effective (
35 ).
With these findings in mind, the assertion of the President's New Freedom Commission (
6 ) that "a personal understanding of the facts" will lessen stigma and increase utilization may seem overly optimistic for two reasons. First, in light of the cultural context, parents and other "gateway providers" will confront deep and pervasive stigmatizing attitudes about mental health treatment (
36 ). Second, efforts to assure the public of the long-term safety and eventual positive social or developmental impacts of mental health treatments will take time. However, our results suggest that education regarding the efficacy of psychiatric medications and establishing relationships between providers and parents may offer the best strategies to decrease the stigma associated with treating children's mental health problems.
Acknowledgments and disclosures
The authors acknowledge project support by the National Science Foundation to the National Opinion Research Center; Eli Lilly and Company; the Office of the Vice President for Research, Indiana University; and grant K02-MH-012989 from the National Institutes of Health and National Institute of Mental Health to Dr. Pescosolido, principal investigator. The authors thank Tom Smith and staff members of the Indiana Consortium for Mental Health Services Research, Schuessler Institute for Social Research, Indiana University.
The authors report no competing interests.