When developing evidence-based treatments, it is important to ensure that the treatment is effective for all individuals, regardless of their ethnicity. Complicated grief is a prolonged grief disorder that occurs among 10%–20% of bereaved individuals and is associated with negative mental and physical health consequences. Core symptoms include persistent inability to accept the death and intense longing for, yearning for, and preoccupation with the person who died, as well as intrusive thoughts or images related to the death, avoidance of reminders of the loss, and feelings of estrangement from close friends and family (
1 ).
To examine whether ethnic differences occur in the presentation of patients with complicated grief or their treatment outcome, we analyzed data from a randomized controlled trial, comparing a novel psychotherapy for complicated grief (complicated grief therapy) to interpersonal psychotherapy. We report results for 19 African-American participants and 19 Caucasian-American participants who were matched on age, sex, and intensity of grief at baseline. Possible differences in baseline severity of anxiety, depression, and functional impairment were examined, and treatment alliance, treatment completion, and treatment outcomes were compared. We hypothesized that because African Americans often report more—and more severe—somatic symptoms than Caucasian Americans (
2 ), they would show greater baseline severity of insomnia, appetite loss, and concerns about their physical health. Furthermore, because African Americans report less satisfaction with health care in general (
3 ), we predicted that they would have lower scores on therapeutic alliance, a higher rate of treatment dropout, and a lower rate of treatment response.
Methods
The study design is described in detail elsewhere (
1 ). Briefly, participants were recruited from and treated at a university-based outpatient research clinic and a satellite clinic in a low-income African-American community. They were randomly assigned to receive standard interpersonal psychotherapy or interpersonal psychotherapy enhanced with focused complicated grief components. Each group was provided treatment in approximately 16 sessions over 16 to 20 weeks. Nine of the African Americans were assigned to interpersonal therapy, and ten were assigned to the enhanced therapy. Thirteen of the Caucasian Americans were assigned to interpersonal therapy, and six were assigned to the enhanced therapy. Posttreatment assessment was obtained by evaluators blinded to treatment assignment and by self-report questionnaires. Because of the small sample, analyses were done by ethnicity, combining participants across the two treatments.
The study was approved by the University of Pittsburgh Institutional Review Board. Participants were enrolled, after written informed consent was obtained, between April 2001 and April 2004. Deidentified data were used in this secondary data analysis that included all 19 African-American participants and 19 Caucasian-American participants matched on sex, age, and baseline grief intensity.
Inclusion in the study required a score greater than 30 on the Inventory of Complicated Grief (
4 ) at least six months after the death of a loved one and a judgment by the research team that complicated grief was the most important clinical problem. Persons with a current substance use disorder, a current or past psychotic disorder, suicidality requiring hospitalization, or a pending lawsuit or disability claim related to the death or who were receiving ongoing psychotherapy were excluded. Stable dosages of psychotropic medication were permitted.
Evaluators, trained to reliability, conducted assessments before and after treatment, blind to treatment assignment. Pretreatment evaluators utilized a structured clinical interview for the assessment of complicated grief (available from the last author) and the Structured Clinical Interview for DSM-IV (
5 ). Posttreatment evaluation included these instruments and the Clinical Global Impressions scale (CGI) (
6 ). Response to treatment was defined as a final CGI score of 1 or 2 (much or very much improved). Self-report measures, including the Beck Depression Inventory (BDI) (
7 ) and the Beck Anxiety Inventory (BAI) (
8 ), were completed before and after treatment. The Working Alliance Inventory (WAI) (
9 ) was completed at treatment sessions 4, 8, and 12.
We used McNemar's test to compare treatment response as measured by a final CGI score of 1 or 2, dropout, and endorsement of sleep disturbance, weight or appetite loss, and preoccupation with health items from the BDI (dichotomized to any versus none) at baseline. Paired t tests on the matched pairs compared total BAI scores at baseline. Fisher's exact test compared rates of baseline diagnoses. Signed-rank tests compared values on the WAI between racial groups. The Wilcoxon test was used for the alliance measures for African-American participants by site (all therapist-patient dyads with African-American participants were at the satellite clinic). All tests were considered significant at the .05 significance level (two-tailed).
Results
African-American and Caucasian-American participants exhibited no difference in pretreatment scores on the BAI or in rates of insomnia, appetite loss, weight loss, or health preoccupation. No significant differences were found in current or lifetime comorbid DSM-IV diagnoses. Diagnoses were as follows: current depressive disorder, 11 (58%) Caucasians and eight (42%) African Americans; lifetime depressive disorder, 16 (84%) Caucasians and 12 (63%) African Americans; current anxiety disorder, 14 (74%) Caucasians and 16 (84%) African Americans; lifetime anxiety disorder, 15 (79%) Caucasians and 16 (84%) African Americans; current somatoform disorder, no Caucasians and three (16%) African Americans; lifetime somatoform disorder, no Caucasians and three (16%) African Americans; current alcohol or drug use disorder, no Caucasians or African Americans; and lifetime alcohol or drug use disorder, three (16%) Caucasians and eight (42%) African Americans. No significant difference was found in antidepressant medication use between the two ethnic groups; ten (53%) Caucasians and six (32%) African Americans were taking antidepressants.
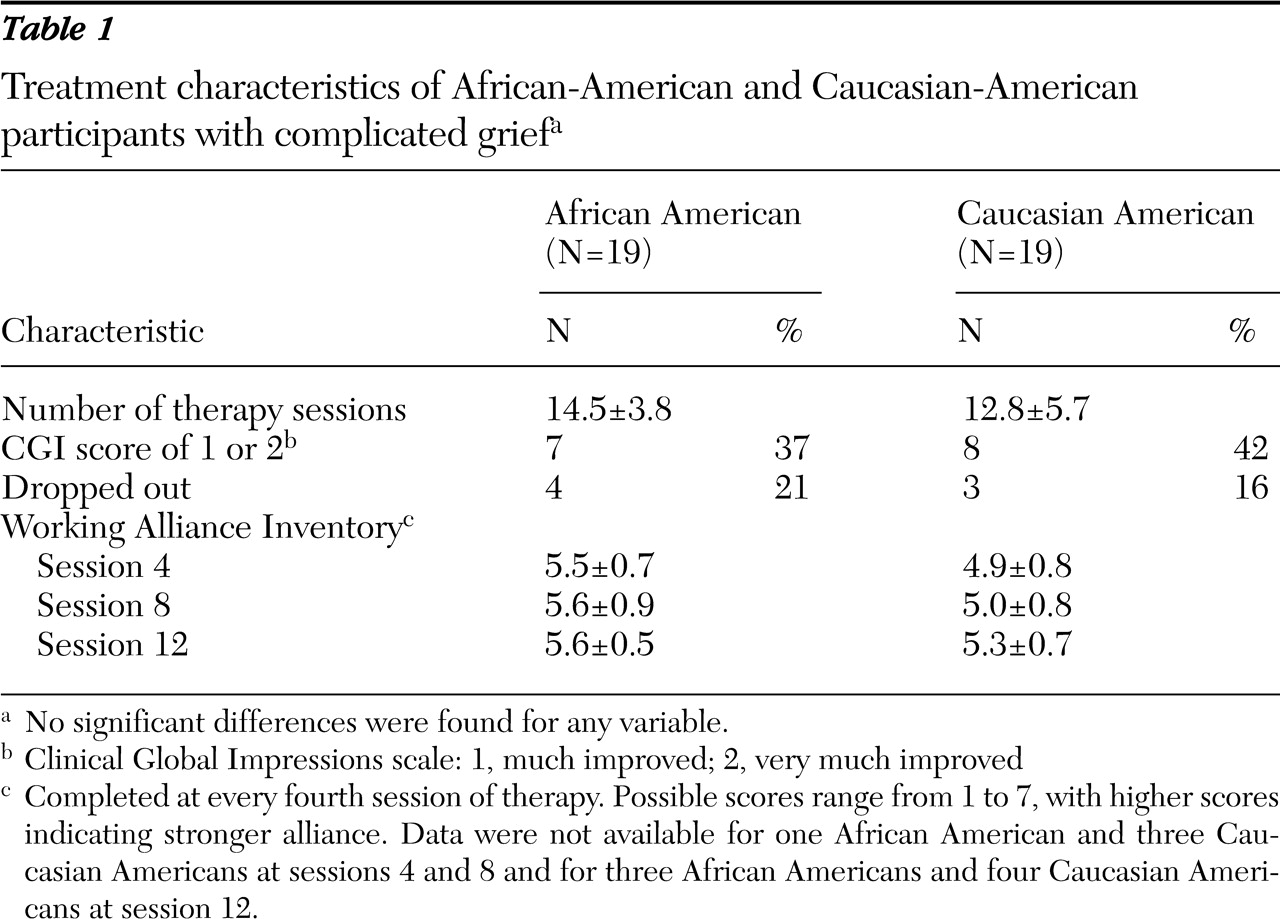
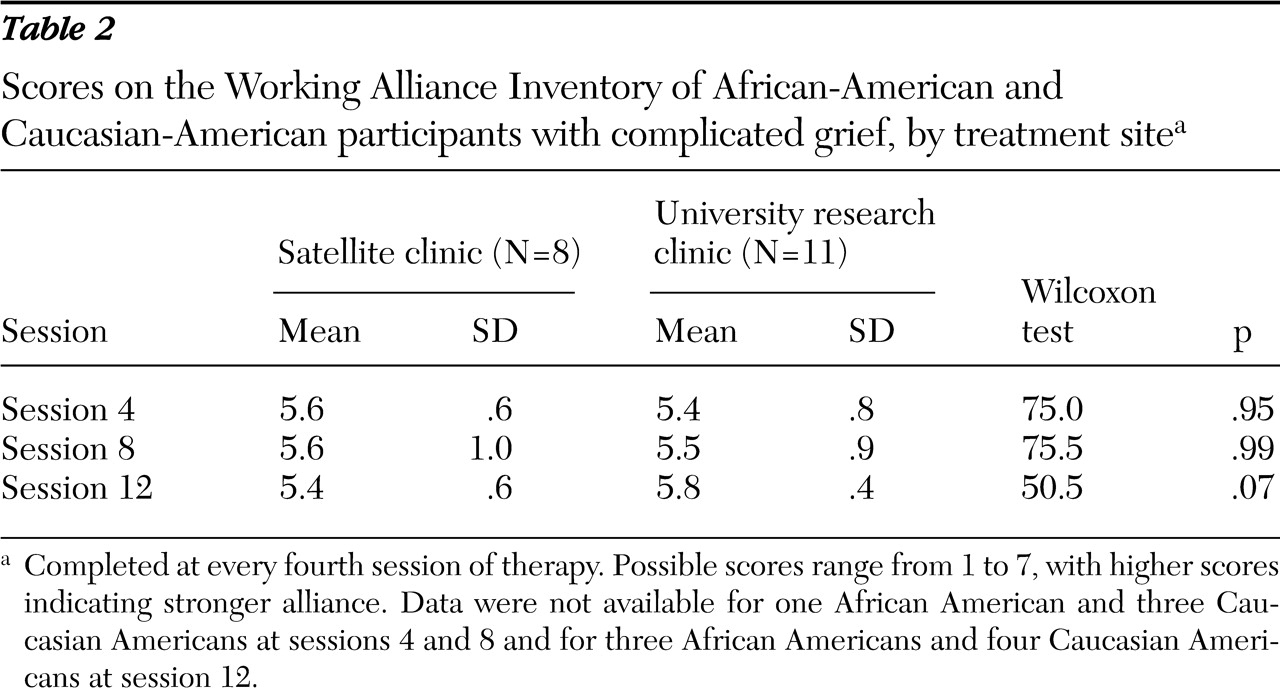
Data in
Tables 1 and
2 show that the groups did not differ in any of the treatment-related variables. Notably this was true for the subgroup of eight African Americans treated in the satellite clinic as well as for African Americans treated in the university clinic (
Table 2 ).
Discussion
Although few people in need of mental health treatment receive it, persons from ethnic minority groups are among those least likely to receive services appropriate to their needs. How mental health systems are financed and organized appears to interact with cultural factors to produce wide-ranging variation in rates of access (
10 ). However, even when barriers to accessing care are lifted, ethnic disparities in treatment outcome persist (
11 ). This study's intent was to identify early on in the development of complicated grief therapy the intrinsic ethnic-cultural differences between grieving African Americans and Caucasian Americans in their presentation and in treatment processes and outcomes. Identified differences would then be used to tailor complicated grief therapy to improve its acceptability and treatment response rates for grieving African Americans.
We found no differences between ethnic groups with complicated grief in baseline severity of symptoms of anxiety or depression. In addition, no differences were found in treatment engagement or response. Our study is limited by a small sample, and we cannot exclude the possibility of a type II error. In particular, there was a suggestion of higher anxiety, more health concerns, and more somatization among the African Americans. African Americans in this study also endorsed higher rates of lifetime substance use disorders. Thus we cannot rule out the possibility that anxiety or somatic symptoms—or both—may be culturally acceptable reasons to seek mental health treatment or that such symptoms are related to folk idioms of distress (
12 ). We made a concerted effort to recruit African-American participants, including the addition of a site that serves a low-income clientele. As a result, eight of 19 African Americans (42%) and none of the Caucasian Americans were recruited from the low-income neighborhood clinic.
Several of our therapists were African American, a fact that might have contributed to the good working alliance and low dropout rate. However, we found no alliance differences in mixed-ethnicity therapist-patient dyads compared with same-ethnicity dyads. This may be related to discussions of cultural sensitivity that were regularly included in supervision sessions. Notably, treatment alliance scores, completion rates, and outcome were high, even though African Americans in this study were more likely to have low income, a low level of education, and substance use disorders—factors that usually produce greater illness severity and poorer outcome.
These findings are similar to those in a recent study of panic disorder that found no difference in response to standard treatment in a low-income population (
13 ). This study adds to the growing body of literature that several evidenced-based treatments are appropriate for individuals from ethnic minority groups (
14 ).
Conclusions
We conclude that there is no reason to expect clinically important differences between African-American and Caucasian-American individuals with complicated grief related to clinical presentation or to treatment engagement or outcome.
Acknowledgments and disclosures
This research was supported by grants R01-MH-60783, P30-MH-30915, P30-MH-52247, K23-MH-07152001-A1, and R25-MH-60473 from the National Institute of Mental Health and by grant P60-MD-000-207 from the National Center for Minority Health and Health Disparities of the National Institutes of Health.
Dr. Reynolds has received research support from GlaxoSmithKline, Forest Laboratories, Bristol-Myers Squibb, Eli Lilly and Company, and Pfizer Pharmaceutical Company. Dr. Frank has received grant support from Forest Research Institute, Pfizer Pharmaceutical Company, Eli Lilly and Company, and Novartis Pharmaceuticals. She is on advisory boards for Pfizer Pharmaceutical Company, Eli Lilly and Company, and Servier. Dr. Shear has received support from Forest Laboratories and is a consultant for Pfizer Pharmaceutical Company. The other authors report no competing interests.