Mental illness is common among hospitalized medical-surgical patients (
1 ). The physical and psychological manifestations of mental illness, as well as side effects of psychotropic medications, may delay the detection of complications and cause unnecessary deaths (
2 ). Many patients with serious mental illness are treated on general surgical floors of acute care hospitals, where providers may be unfamiliar or uncomfortable with the care of psychiatric patients. In addition to presenting a higher risk of adverse events, the care of patients with serious mental illness involves greater use of hospital resources and higher costs because their hospital stays are longer (
3 ).
Registered nurses act as a surveillance system for patients and are essential to early detection of complications and adverse events; surveillance is supported by adequate staffing and an appropriately educated workforce (
4 ). Lower patient-to-nurse ratios (
5 ) and higher proportions of baccalaureate-prepared nurses (
6 ) have been associated with lower surgical patient mortality rates and better quality of hospital care. However, no studies have investigated the effects of nurse staffing and education on outcomes of surgical patients with comorbid serious mental illness.
The purpose of this study was to identify surgical patients with comorbid serious mental illness, compare their outcomes with those of patients without serious mental illness, and determine the effects of nurse staffing and education levels on patient outcomes.
Methods
This cross-sectional study included data from a nurse survey, patient discharge records, the American Hospital Association (AHA) Annual Survey, and the Pennsylvania Department of Health Hospital Questionnaire. The study received expedited approval from the institutional review board of the University of Pennsylvania.
A total of 157 hospitals were included in the analysis. To be included a hospital had to have more than 100 surgical discharges during the window of observation (April 1, 1998, to November 30, 1999). Data on hospital characteristics had to be available from the AHA surveys and the Department of Health questionnaire. In addition, survey responses were required from more than ten staff nurses at the hospital in order to create reliable staffing and education estimates (
5 ), and more than ten patients had to have a diagnosis of serious mental illness either upon surgical admission or during a hospitalization within 90 days before the surgical admission.
Nurse survey data were collected through a survey mailed in 1999 to half of all licensed registered nurses in Pennsylvania. The response rate for the survey was 52% (a total of 42,329 nurses). The final sample included 9,989 staff nurses who worked in direct patient care. Patients aged 20 to 85 years with a diagnosis-related group for general, orthopedic, or vascular surgery between April 1, 1998, and November 30, 1999, were included in the analysis. The first admission for any of the specified diagnosis-related groups for each patient was analyzed. There were 228,433 patients in the final sample.
The nurse staffing measure (
5 ) was created for each hospital by calculating the mean number of patients that nurses reported caring for on their last hospital shift. The nurse education measure was calculated for each hospital as the proportion of nurses who reported that their nursing degree was a baccalaureate or higher. Thirty-day mortality was defined as death within 30 days of admission. Failure to rescue was defined as death after the patient developed a complication after surgery (even if the patient had been discharged); this measure has well-established statistical properties for assessing the effect of organizational characteristics on surgical outcomes (
7,
8 ). Length of stay was extracted from a variable indicating the number of days from the admission date to the discharge date for each patient.
Several hospital and patient characteristics were used for risk adjustment (
5,
7,
9,
10 ). Hospital characteristics included teaching status, technology status, number of beds, and board certification of surgeons. Patient characteristics included age, sex, race, admission source, insurance status, surgery type, and medical comorbidities (
7,
9,
10 ). For this study, patients with serious mental illness (psychotic conditions, major affective disorders, and bipolar disorders) were identified through a classification system that cross-referenced
ICD-9 and
DSM-IV diagnoses (
11 ). [A list of the
ICD-9 and
DSM-IV diagnoses is available as an online supplement to this article at
ps.psychiatryonline.org .]
Patients with serious mental illness were identified, and separate descriptive statistics were calculated. The effect of nurse staffing and educational levels on outcomes was examined with generalized estimating equations. The models were adjusted for hospital and patient characteristics, as well as significant interactions. The statistical significance level was set at .05. SAS version 9.1 was used for data analyses. [A more detailed description of the methods and a list of additional references are available in an online supplement to this article at
ps.psychiatryonline.org .]
Results
Of the 228,433 surgical patients in the sample, 4.7% (N=10,666) had a diagnosis of serious mental illness upon admission or during an admission within the previous 90 days. Eighty percent (N=8,563) of these patients had a major depressive disorder. The mean±SD age for patients in the group with serious mental illness was 60.0±16.1, and for the group without serious mental illness it was 59.2±17.0. Among those with serious mental illness 80.6% (N=8,601) were white, 5.9% (N=627) were black, and 13.5% (N=1,438) were in the category "other." Among those without serious mental illness 78.6% (N=171,228) were white, 6.9% (N=15,055) were black, and 14.5% (N=31,484) were other.
Thirty percent (N=3,191) of patients with serious mental illness were male, compared with 44.5% (N=96,800) of the group without serious mental illness. A higher percentage of patients with serious mental illness were admitted as an emergency (31.8%, [N=3,390] compared with 27.0% [N=58,772] of patients without serious mental illness; p<.01)
A higher percentage of patients with serious mental illness had public insurance (54.4% [N=5,799] compared with 44.2% [N=96,236] of those without serious mental illness; p<.01). Larger proportions of patients with serious mental illness had diagnoses of medical comorbidities, including hypertension, chronic lung disease, diabetes, and substance abuse. [A table with data on medical comorbidities is available as an online supplement to this article at
ps.psychiatryonline.org .]
The mean number of patients cared for by a nurse on the most recently worked shift in the average hospital was 5.9±1.0. Average nurse workloads across hospitals ranged from 3.7 to 9.2 patients. In the average hospital, about 30% of nurses held at least a bachelor's degree, with a range of none to 74%.
Among patients with serious mental illness, 1.8% (N=188) died within 30 days of admission. The percentage was similar—2.0% (N=4,265)—among those without serious mental illness. Patients with serious mental illness experienced more postsurgical complications (30.6% [N=3,259] compared with 26.4% [N=57,528] of those without serious mental illness; p<.001). Among these patients, the proportion of failure-to-rescue cases was significantly lower for patients with serious mental illness (5.8% [N=188] compared with 7.4% [N=4,265] of those without serious mental illness; p<.001), Patients with serious mental illness had an average length of stay almost one full day longer than patients without serious mental illness (6.1±6.3 days compared with 5.3±6.1 days; p<.001).
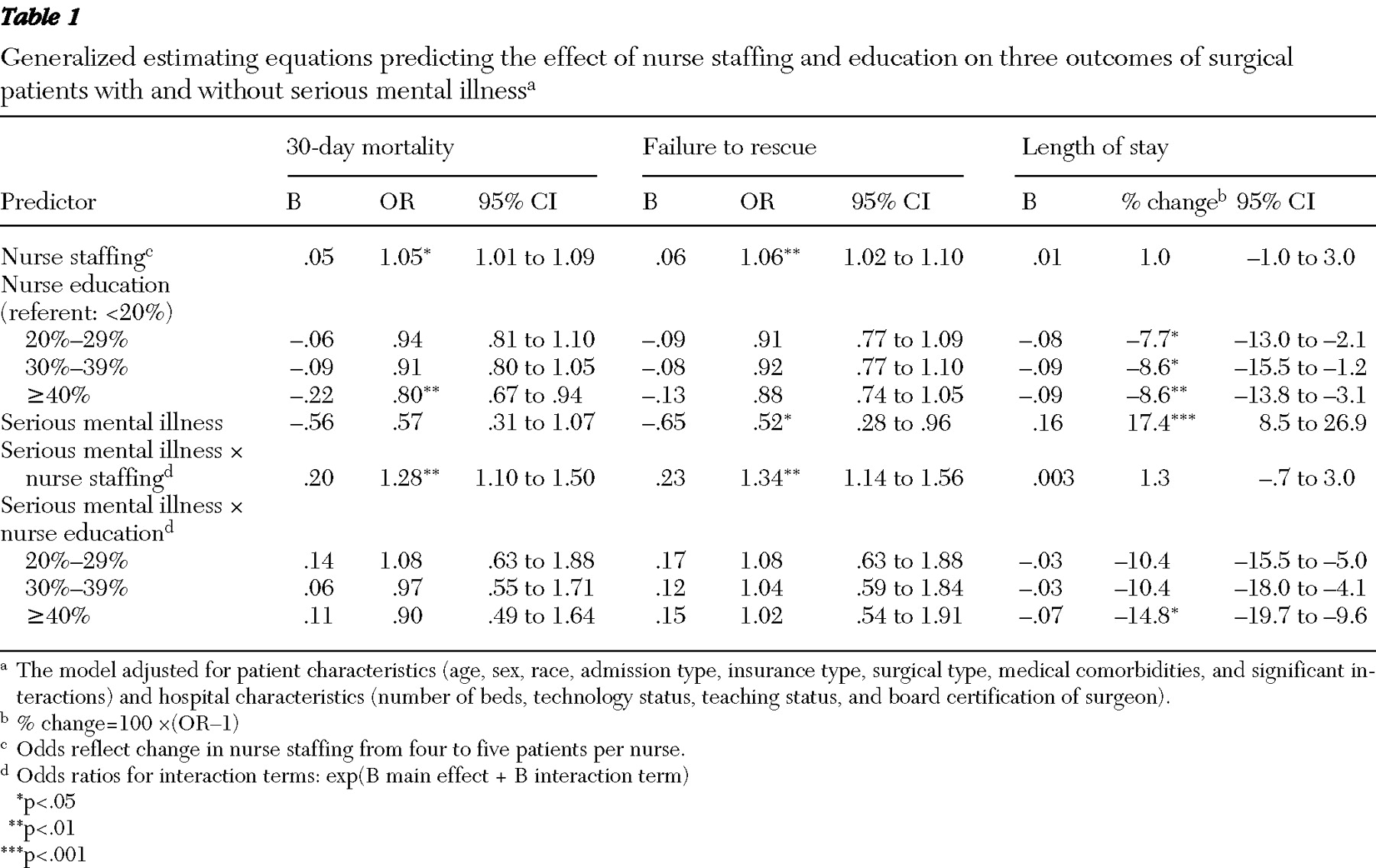
Estimates from the generalized estimating equation models are shown in
Table 1 . The odds of mortality within 30 days of admission and of failure to rescue for patients with serious mental illness were significantly lower than those for patients without serious mental illness; however, nurse staffing had a notably stronger effect on the prevention of death among patients with serious mental illness. The odds of dying within 30 days and of failure to rescue were compared in hospitals with five patients per nurse and those with four patients per nurse. When nurses had more patients, the odds of dying within 30 days were 28% higher for patients with serious mental illness than for those without serious mental illness, and the odds of failure to rescue were 34% higher. Although estimates for nurse education were in the hypothesized direction, the analysis did not show a statistically significant effect of education on mortality outcomes.
When the analysis controlled for patient and hospital characteristics, length of stay for patients with serious mental illness was 17.4% longer than that for patients without serious mental illness. Length of stay was compared in hospitals where 40% or more of nurses had a baccalaureate degree and hospitals where less than 20% did so. For patients with serious mental illness, length of stay was 14.8% shorter in the hospitals where nurses had more education. This difference nearly compensates for the almost 17% longer hospital stays associated with having a serious mental illness. Nurse staffing did not have a statistically significant association with length of stay.
Discussion
This study demonstrated that better nurse staffing had an even greater protective effect on the outcomes of vulnerable hospitalized patients than has been previously reported for general surgical patients. The odds of dying within 30 days of admission and of failure to rescue increased significantly for all surgical patients as the patient-to-nurse ratio increased; however, the odds were significantly higher for patients with comorbid serious mental illness. Nurse education demonstrated hypothesized effects on 30-day mortality and failure to rescue in the models, but the effects did not reach statistical significance. The detrimental effect of having a serious mental illness on length of stay was mitigated almost completely in hospitals with high proportions of baccalaureate-prepared nurses.
Some limitations in the study design and data should be noted. The analyses were restricted to data collected in 1999 for a somewhat different, but related, purpose. There is no reason to expect that the basic phenomena under study have changed over time; indeed nurse shortages and continuing cost containment pressures on the hospital workforce have probably resulted in greater vulnerabilities for hospitalized patients. The unique nature of the linked nurse, patient, and organizational data provided an unusual opportunity to examine the research questions. Despite the large scale of the parent study, the analyses for this study were limited in terms of statistical power by the size of the patient sample with serious mental illness and their lower death rate compared with patients without serious mental illness. Sensitivity analyses demonstrated that estimates became stable with more than ten surgical patients with serious mental illness per hospital. Examination across multiple years and data sources would increase the likelihood of accurately identifying psychiatric illness. The proportion of patients with serious mental illness in this study, however, is comparable to current national prevalence rate estimates (
12,
13 ). Given the high rates of undiagnosed psychiatric illness and the possibility of undercoding of chronic conditions on patient discharge abstracts, outcome estimates for patients with serious mental illness in this study represent the worst cases. In the sample of patients with serious mental illness, 80.3% (N=8,563) had a diagnosis of major depression, which is slightly higher than the proportion reported in the population of persons with serious mental illness (
12 ). Differences in patient characteristics between the group with serious mental illness and the group without it were accounted for in the risk adjustment modeling.
Overall, patients with serious mental illness had lower odds of dying within 30 days of admission and after experiencing a complication resulting from surgery. Because patients with serious mental illness have shorter life expectancies (
14 ), this finding seems counterintuitive and could be attributed to selection bias. Patients with serious mental illness may receive procedures only when they are less severely ill than their peers; however, our data did not allow us to investigate this possibility. Such a bias might obscure an overall effect of increased mortality among patients with serious mental illness, but it would not obscure an interaction with nursing characteristics. The sample of patients with serious mental illness in this study may have been fairly healthy compared with the overall population of persons with serious mental illness.
Conclusions
Levels of nurse staffing in hospitals have been found to be the most consistent and prominent nursing organization characteristic to be predictive of patient outcomes (
15 ). Findings of this study add to this body of evidence and suggest that nurse staffing may be one of the most important components of the surveillance system that protects patients from adverse outcomes. Patients with serious mental illness are vulnerable to poor outcomes because of their impaired cognition and because their poor communication skills require nurses to spend more time understanding them. Although this study focused on patients with serious mental illness, many patients in acute general hospitals have similar vulnerabilities related to poor communication skills, including those with dementia and non-English speakers.
The strong effect of nurse staffing on outcomes of patients with serious mental illness has implications for hospital administrators and policy makers. The results of this study suggest that patients with diagnoses of serious mental illness may especially suffer from hospital financial cutbacks, which often target nurses. The fatal consequences associated with high patient-to-nurse ratios have been demonstrated in this study and in many others. Results of this study suggest that nurses' education may be an important element in the length of stay of surgical patients with serious mental illness. Growing numbers of patients with psychiatric illness, along with continued evidence of poor outcomes in hospitals with inadequate staffing and lower percentages of educated nurses, suggest a need to consider payment policy changes that would more appropriately compensate hospitals for the nursing care required to produce good outcomes for patients with serious mental illness.
Acknowledgments and disclosures
This study was supported by grants R01-NR04513 and T32-NR0714 from the National Institute of Nursing Research, National Institutes of Health. The authors thank Nancy Hanrahan, Ph.D., R.N., Eileen Lake, Ph.D., R.N., Jeffrey H. Silber, Ph.D., M.D., Douglas Sloane, Ph.D., and Timothy Cheney for their thoughtful assistance.
The authors report no competing interests.