Mental health problems and substance abuse are common among persons living with HIV and are associated with lower quality of life, inconsistent use of antiretroviral therapy, and worse medical outcomes (
1,
2,
3,
4,
5,
6,
7 ). Substance abuse also contributes to HIV transmission through needle sharing and an association with high-risk sex (
8,
9 ). Despite the availability of effective therapies, many persons with HIV do not receive needed mental health and substance abuse care (
10,
11,
12,
13,
14 ).
Medical care, mental health care, and substance abuse care often occur in separate treatment sectors with distinct care sites, organization, and financing (
15,
16 ). This fragmentation discourages comprehensive care for patients with coexisting conditions. The Institute of Medicine's 2006 report on
Improving the Quality of Health Care for Mental and Substance-Use Conditions emphasizes the need to integrate and coordinate care for patients with coexisting medical, mental health, and substance use conditions and reviews a number of general strategies to accomplish this (
15 ). First, integrated care models attempt to strengthen organizational linkages between existing medical care, mental health care, and substance abuse treatment services. These affiliations may facilitate referral and improve care coordination by decreasing administrative and financial barriers. Second, case managers can assist in identifying care needs and linking patients to appropriate treatment. Third, having case managers, medical clinicians, mental health professionals, and substance abuse clinicians in a common location can improve access to care by reducing transportation barriers and making it easier for patients to see the most relevant clinicians. Finally, case managers, medical clinicians, mental health professionals, and substance abuse clinicians can form multidisciplinary teams that routinely meet to discuss patient needs and promote care coordination. Several studies have evaluated integration of medical care in the mental health and substance abuse treatment settings (
17,
18,
19,
20,
21 ). In contrast, less is known about the effect of interventions to integrate mental health and substance abuse treatment with medical clinics caring for persons with HIV (
22 ).
In this study we examined the impact of clinic organizational characteristics on mental health care and substance abuse care in the HIV Cost and Services Utilization Study (HCSUS), a nationally representative sample of persons in care for HIV (
23 ). Prior analyses of data from the HCSUS identified patient characteristics associated with mental health and substance abuse care, including income, education, insurance status, and HIV symptom burden (
10,
13 ). Little is known, however, about the impact of medical clinic organizational characteristics on access to behavioral health services for this population. We hypothesized that access to mental health care and substance abuse care would be better for patients in clinics with institutionally affiliated mental health care and substance abuse care and also when affiliated mental health care and substance abuse treatment are located in the medical clinic. In addition, we expected that access to mental health care and substance abuse care would be better for persons receiving care in clinics with on-site case managers, clinics with more frequent multidisciplinary team conferences, and in HIV specialty clinics.
Methods
Patient sample
The HCSUS was a multistage probability sample of all noninstitutionalized persons who received outpatient care for HIV in the United States between 1996 and 1998. Prior publications describe the HCSUS sampling scheme in detail (
23,
24 ). The baseline survey interviewed 2,864 participants between January 1996 and April 1997. At the first follow-up, between December 1996 and July 1997, a total of 2,466 participants were interviewed; at the second follow-up, between August 1997 and January 1998, a total of 2,267 participants were interviewed. After providing a complete description of the study to the participants, written informed consent was obtained. This study received approval from the institutional review board of the University of Missouri-Columbia.
Clinic sample
In the first follow-up interview, respondents reported where they received HIV care. The HCSUS study team telephoned these clinics and identified 282 treatment sites. Clinic medical directors completed questionnaires for 200 of the 282 sites (71%). These sites cared for 2,031 of the 2,466 (82%) participants at first follow-up, and this group formed our study sample. There were no significant clinical or demographic differences between the full sample and the subsample with associated clinic data (
25 ). We used responses from the first follow-up for two reasons. First, these data were collected closest in time to the survey that gathered clinic data. Second, use of combination antiretroviral therapy had become common by this time, and these responses better reflect care in the current era of HIV medicine (
26 ).
Dependent variables
Our two primary dependent variables were whether at the first follow-up interview patients reported using outpatient mental health specialist care or outpatient substance abuse care since the baseline interview (mean± SD interval 240±80 days). Utilization before the baseline survey was not included. Respondents reported any care and number of visits. Mental health specialists included psychiatrists, psychologists, psychiatric nurses, and psychiatric social workers. A third dependent variable was whether participants reported use of specific illicit drugs (heroin, sedatives, amphetamines, analgesics, cocaine, inhalants, and LSD or other hallucinogens) in the 30 days before the second follow-up survey.
In addition, we asked participants if they had discussed emotional problems with medical providers during clinic visits since baseline, received mental health care during hospitalizations, or attended residential substance abuse treatment. As previously reported, inpatient mental health care and residential substance use treatment were infrequent (1.8% reported inpatient mental health care, and 2.7% reported residential substance abuse treatment since baseline) and were usually associated with outpatient mental health and substance use care, respectively (
10 ). Because of the rarity of inpatient care and significant overlap with reported outpatient care, we restricted our analyses to outpatient mental health care and substance abuse treatment as representative measures of specialist care in the outpatient setting.
Independent variables
Clinic characteristics. Clinic directors reported whether specialized substance abuse treatment or mental health care was available to patients in the same institution as the HIV care site, which we refer to as affiliated care; whether case managers, mental health specialists, or substance abuse treatment professionals were regularly available within the clinic during business hours; whether the clinic was an HIV specialty clinic; the number of multidisciplinary team conferences held per year to discuss care of HIV-positive patients in the clinic; the number of persons with HIV who visited the clinic in the past year; and the percentage of clinic revenue obtained from the Ryan White CARE act, a federal funding program that supports HIV care. "Case manager" was defined as a specified person other than the patient's primary physician, nurse practitioner, or physician's assistant, who served as a manager, advocate, or care coordinator and who helped to arrange and coordinate medical, mental health, and social services. Responses regarding institutional affiliation and on-site location of mental health care and substance abuse specialty care were combined to form separate three-level care affiliation variables: no affiliated care, affiliated off-site care, and affiliated on-site care.
Patient characteristics. In models for predicting use of health services, we adjusted for patient need and predisposing and enabling characteristics that can affect use of mental health care and substance abuse treatment. This adjustment was based on the behavioral model of health care utilization (
27,
28 ) (
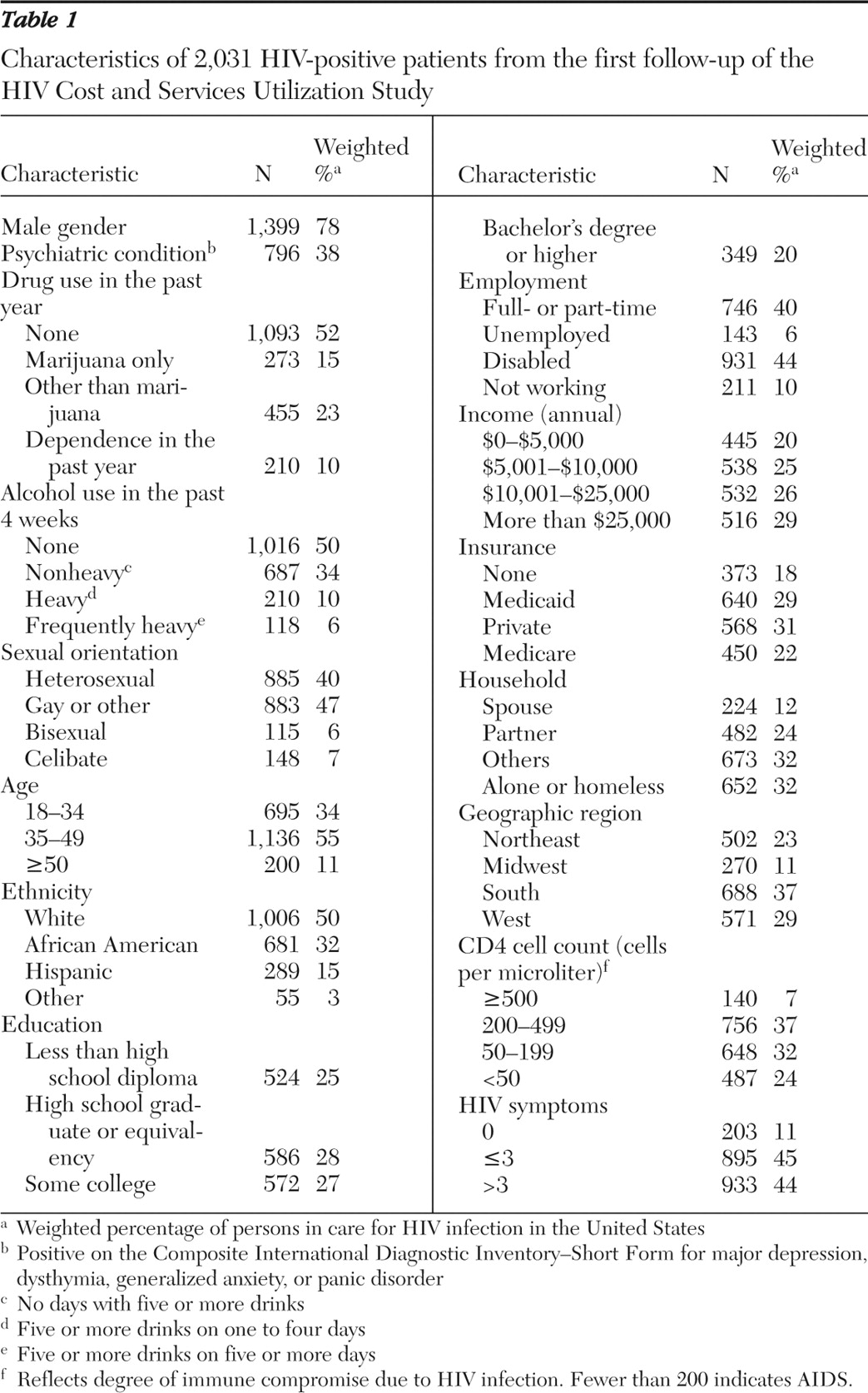
Table 1 ). These variables were identified as important predictors in previous HCSUS analyses (
10,
29 ).
Need variables included measures of psychiatric symptom severity, drug use, and alcohol use. During the first follow-up interview, respondents completed the Composite International Diagnostic Inventory-Short Form (CIDI-SF). To assess psychiatric symptom severity we used a scale ranging from 0 to 16 and derived from the CIDI-SF (
29 ). Variables representing need for substance abuse care were derived from questions regarding drug use in the past year and alcohol use in the past four weeks (
30 ). Drug use was classified as no drugs, marijuana use only without dependence, use of other illicit drugs without dependence, or drug dependence. Alcohol use was classified as no drinking, nonheavy drinking (no days with five or more drinks), heavy drinking (five or more drinks on one to four days), and frequent heavy drinking (five or more drinks on five or more days).
Variables that may predispose patients to or facilitate mental health care and substance abuse care included age, gender, race-ethnicity, sexual orientation, number of HIV-related symptoms, CD4 cell count, insurance status, employment, income, household composition, and geographic region.
Statistical analyses
Data weights accounted for the complex HCSUS design and nonresponse in both the patient surveys and the site surveys, and the weights made the sample representative of all persons in care for HIV in the United States (
25 ). We used SUDAAN software, version 9.1, to account for the complex sampling design and clustering of patients in clinics.
To determine the cross-sectional associations between clinic characteristics and care use, we estimated separate logistic regression models for use of outpatient mental health and substance use specialist care. We adjusted for all described patient variables because these were expected a priori to be associated with both clinic characteristics and use of care. We analyzed the entire sample and adjusted for psychiatric symptom severity as a continuous variable and for level of drug use. Prior studies indicated that patients with less severe psychiatric symptoms that do not meet the cutoff point for disorders, or so-called "subthreshold disorders," may experience increased morbidity, use more behavioral health services, and benefit from efforts to improve behavioral health care (
31,
32,
33 ). Approximately one-third of HCSUS respondents reporting mental health specialist care did not meet criteria for a mental health disorder on the CIDI-SF, and most of these respondents had significant symptoms. Moreover, inspection of the data revealed that the relative impact of clinic characteristics on care use did not differ significantly by presence of a psychiatric disorder on the CIDI-SF or by substance use. In addition, we tested for interactions between need variables and clinic variables in multivariate models for predicting care use.
The models also adjusted for the number of days between baseline and the first follow-up survey, although this did not change estimates for clinic variables. Reported models included all clinic variables hypothesized to predict care, even if results were not significant. Data on clinic team conferences were missing for 11 respondents, and reported logistic regression models used observations for the 2,020 participants with complete data. We subsequently tested whether number of patients with HIV or funding source confounded clinic effects by including in the model the number of HIV-positive patients seen in the clinic and the percentage of funding obtained through the Ryan White CARE act.
Analysis of substance abuse outcomes
In an effort to investigate the relationship between clinic characteristics and substance abuse outcomes, we defined a subpopulation of participants who reported substance abuse in the previous year at the first follow-up interview (N=666) and who were included in the second follow-up survey approximately six months later (N=606). These respondents attended 161 of the 200 original clinics. Because of the high frequency of medical marijuana use among persons with HIV, this sample excluded persons reporting only marijuana use without dependence (
34 ). Within this subpopulation we estimated a logistic regression model for 30-day abstinence from substance use at the second follow-up. In addition to clinic variables, this model included a series of dummy variables indicating which substances the respondent reported using at first follow-up, substance dependence, and the other patient variables described above.
Results
A majority of patients in care for HIV were male (78%), and 38% had a psychiatric condition according to the CIDI-SF (
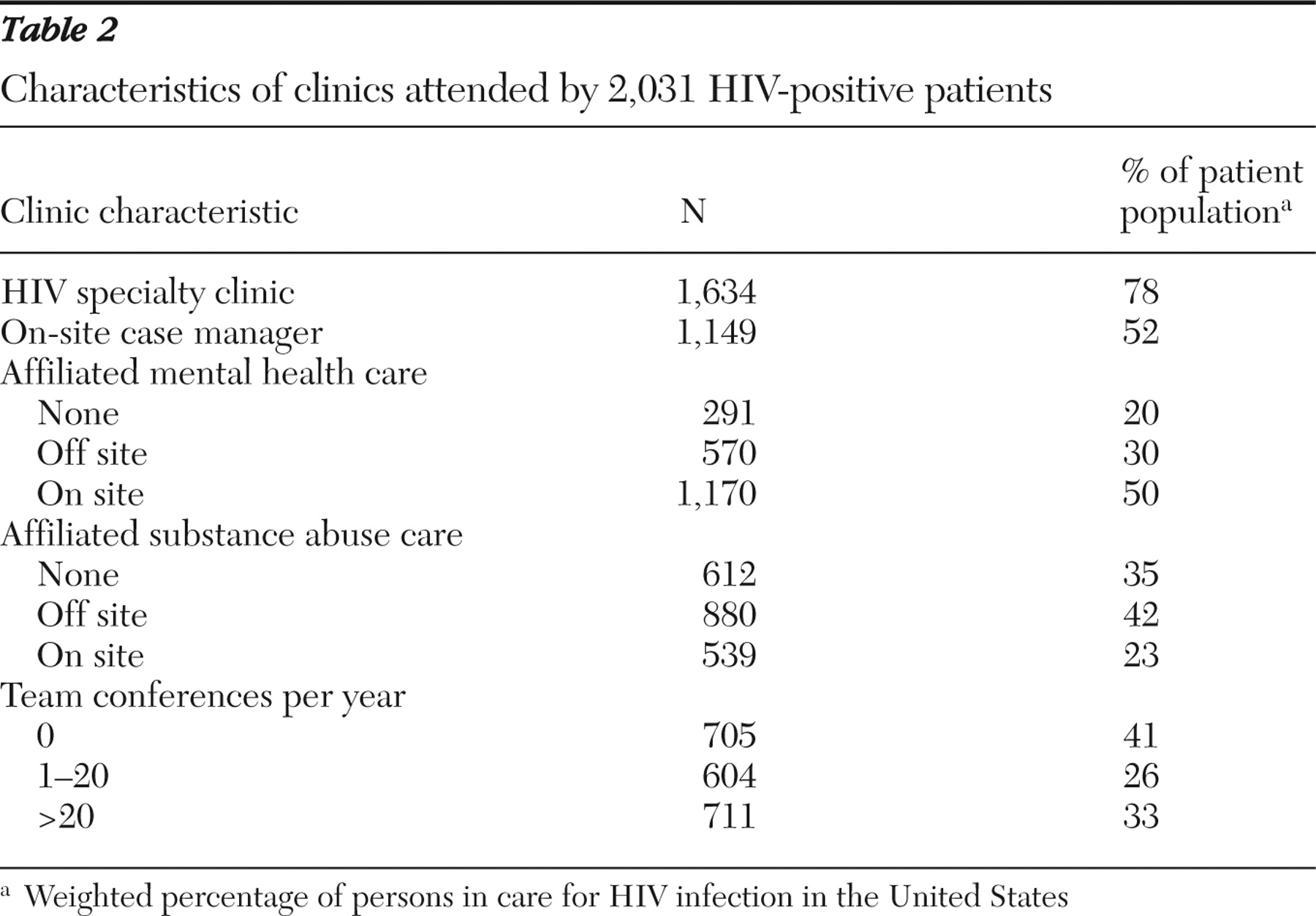
Table 1 ). A higher percentage of persons attended clinics with affiliated mental health care compared with affiliated substance abuse care (80% versus 65%, p=.04), and a majority of patients attended HIV specialty clinics (
Table 2 ). Prior HCSUS analysis found that clinics that specialize in HIV care were more likely to have on-site case managers, mental health specialists, and substance abuse treatment clinicians (
25 ).
Mental health care
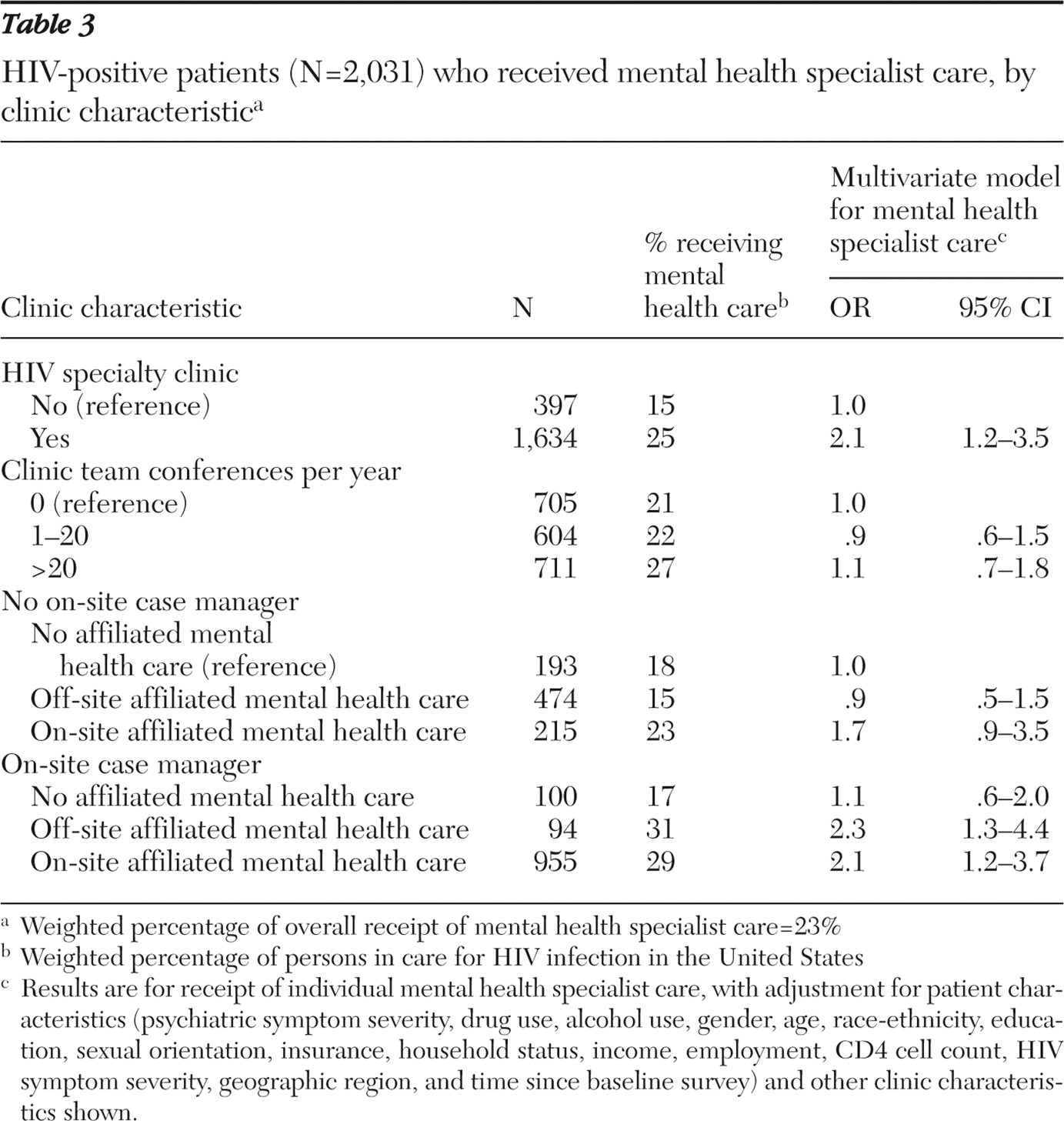
Data inspection suggested an interaction between on-site case management and the degree of clinic affiliation with mental health specialty care (
Table 3 ). On-site case management was associated with a higher percentage of patients seeing a mental health specialist in clinics with affiliated mental health care (31% off site and 29% on site) but not in clinics without affiliated mental health care (17%). For clinics with case managers, a similar percentage of patients received mental health specialist care in clinics with off-site affiliated care (31%) and clinics with on-site care (29%). In contrast, for clinics without case managers there was a tendency for more use of mental health specialist care with on-site care (23%) but not with off-site affiliated care (15%).
The interaction between on-site case management and the degree of affiliation with mental health specialist care was significant in a logistic regression model that adjusted for patient and other clinic characteristics (p=.01 for likelihood ratio test, df=2).
Table 3 reports odds ratios (ORs) and 95% confidence intervals (CIs) for mental health specialist care in clinics with specific combinations of case management and mental health care affiliation compared with clinics without case management or affiliated mental health care. In clinics with on-site case management, the effects of off-site affiliated care (OR=2.3) and on-site care (OR=2.1) were not statistically different.
Patients in HIV specialty clinics were more likely than patients not in HIV specialty clinics to see a mental health specialist, and this association persisted after we adjusted for patient and other clinic characteristics (
Table 3 ). In multivariate analysis, there was not a significant association between the number of clinic team conferences and care use. Discussion of emotional problems with medical providers was common (39%), but no clinic characteristics were significantly associated with such discussions (data not shown).
Substance abuse care
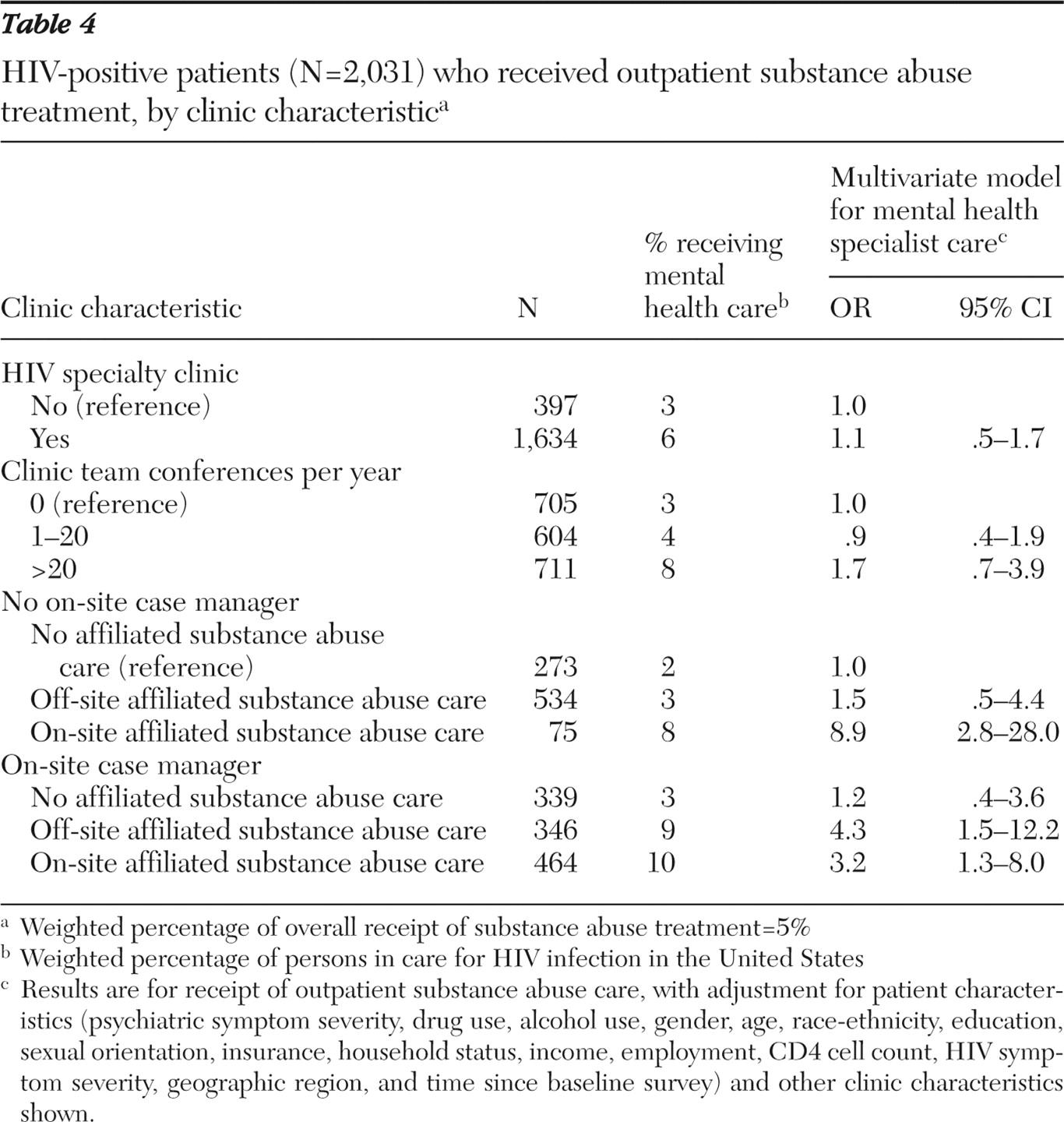
We observed similar results for use of outpatient substance abuse care (
Table 4 ). On-site case management was associated with a higher percentage of patients receiving substance abuse care in clinics with affiliated substance abuse care (9% in clinics with off-site affiliated care, and 10% in clinics with on-site care) but not in clinics lacking any affiliated care (3%). For clinics with case managers, the effect was similar for affiliated off-site substance abuse care and on-site substance abuse care. In the absence of on-site case management, only on-site substance abuse care was associated with a higher percentage of treatment use (8%).
The interaction between case management and affiliated substance abuse care remained significant in the multivariate model (p<.01 for the likelihood ratio test, df=2). Most clinics with on-site substance abuse care also offered on-site case management. Of the 539 participants attending clinics with on-site substance abuse care, only 75 were in clinics without case management, and 67 of these were in one clinic. The CIs for this group were consequently large (OR=8.9), and the estimated effect of this care arrangement on treatment use was not statistically different from the effect for clinics with both on-site care and case management (OR=3.2) (
Table 4 ). HIV specialization and number of team conferences were not associated with substance abuse care after the model adjusted for patient and other clinic variables.
There were no significant interactions between need variables and any significant clinic predictors of mental health or substance abuse care. Neither funding from the Ryan White CARE act nor clinic volume of HIV patients were significant predictors of care, and inclusion of these variables did not significantly change the effects of other clinic variables. Poisson regression models of the number of mental health or substance abuse care visits yielded results similar to the logistic regression models.
Substance abuse outcomes
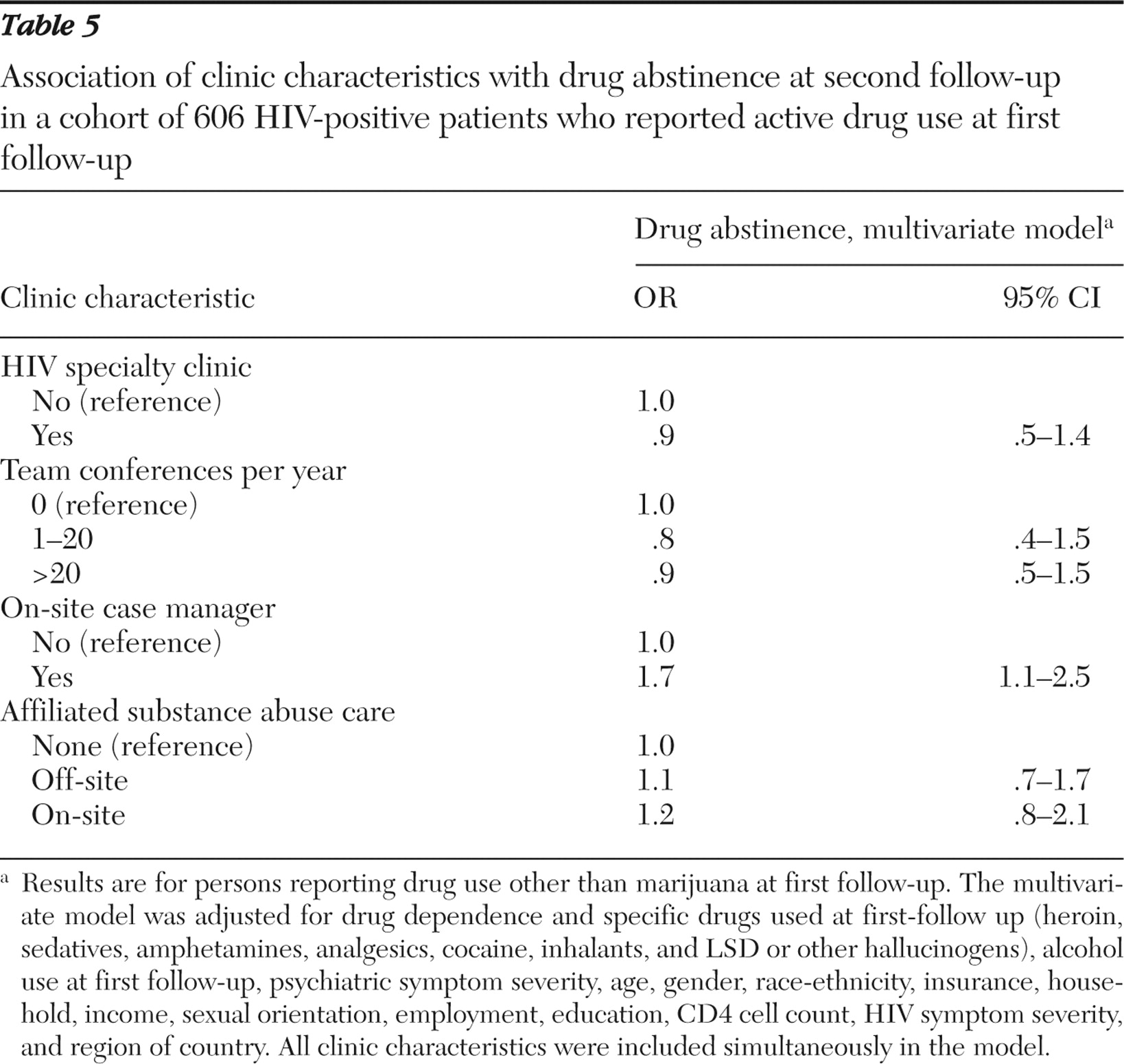
We next examined the association of clinic characteristics with substance abuse outcomes in the subset of 606 persons reporting substance abuse in the year before the first follow-up interview (
Table 5 ). In a logistic regression model that adjusted for other clinic and patient characteristics, including use of specific drugs and drug dependence at first follow-up, we observed an association between care in clinics with on-site case management and 30-day abstinence from substances at follow-up six months later (OR=1.7). In this smaller subpopulation, the effect of affiliated substance abuse care was not significant in the multivariate model, and the interaction between case management and care affiliation was not significant.
Discussion
In this nationally representative study of persons in care for HIV, organizational characteristics of the medical clinic had an important effect on use of mental health care and substance abuse specialist care. Effective antiretroviral therapy has transformed HIV infection from a terminal illness into a chronic illness. These results add to the existing literature on the impact of medical clinic organizational characteristics on access to behavioral health services for patients with chronic medical conditions (
15,
35 ).
Case managers may facilitate linkage to mental health care and substance abuse care by making referrals, scheduling appointments, and arranging transportation (
36 ). This may explain the observation that affiliation with off-site behavioral health services was associated with increased behavioral health care for patients in clinics with case managers but not in clinics without case managers. Furthermore, on-site case management was associated with more behavioral health care only if treatment services were affiliated with the clinic. This suggests that case management alone may not overcome the administrative barriers separating the medical and behavioral health care sectors. Both case management and some form of organizational affiliation with behavioral health services may be necessary to facilitate referral. In this study we did not know the exact nature of affiliations between medical clinics and behavioral health services, only whether mental health or substance abuse care was available at the same institution. Clinics may establish referral processes and care contracts with behavioral services outside of the institution or, conversely, may have little administrative or financial linkage to services within the same institution. Future studies should characterize the impact of specific financial and procedural relationships between medical clinics and behavioral health services.
Prior studies in substance abuse treatment settings found that on-site medical care leads to greater use of medical care than does referral to off-site medical providers, but these studies did not account for location of case management (
20,
37 ). In clinics with case managers, we observed similar use of behavioral health services for clinics with off-site affiliated care and clinics with on-site care, suggesting that easily accessible case managers may help patients navigate referral and transportation barriers. Clinics that are unable to arrange on-site behavioral health care may find that providing on-site case management and affiliating with off-site behavioral health services is a more attainable goal.
Few participants in this study attended clinics with on-site substance abuse care but no case management. Most of these patients attended one clinic, and the observed impact of this particular care configuration on substance abuse treatment may not generalize. This study did, however, include a large number of participants in clinics with both on-site substance abuse care and case management, and it seems unlikely that removing case managers from clinics with on-site substance abuse care would improve access to treatment.
Our findings suggest that persons receiving HIV care in clinics with on-site case managers may also have better substance abuse treatment outcomes. In addition to helping patients obtain substance abuse treatment and mental health care, case managers help arrange other services, such as housing, transportation, and child care (
12 ). These services stabilize the disorganized living situations of persons abusing substances and may independently improve outcomes (
38 ). The effect of on-site case management within medical clinics is probably mediated by higher use of case managers. We cannot exclude the alternative possibility that on-site case management is a marker for high-functioning clinics and that other, unmeasured characteristics of these clinics may lead to more use of behavioral health services and improved substance use outcomes.
HIV specialization and mental health care
Clinics that specialize in HIV provide higher-quality HIV care, but little is known about the impact of HIV specialization on care for other conditions (
25,
39 ). In this study, persons receiving care in HIV specialty clinics were more likely to see a mental health specialist, even after we adjusted for other clinic characteristics. Many persons with HIV infection have multiple comorbid conditions, including a high prevalence of mental health conditions. Thus providers and clinics that specialize in HIV care may be more likely to develop knowledge and systems that facilitate mental health care. There was no association between HIV specialization and substance abuse care, however, after adjustment for other clinic characteristics. This may be due to greater difficulties in detecting patients with substance abuse.
Clinic team conferences and access to specialist care
Although there was a trend toward more substance abuse care for patients in clinics with more team conferences, there was no statistically significant association between the number of team conferences and mental health or substance abuse care, after we adjusted for other clinic characteristics. Simply counting the number of team conferences may be too general a measure to capture the impact of multidisciplinary care teams on access to behavioral health services. Demonstration of an effect for care teams may require better measures of team structure and function that may correlate with team effectiveness, such as expertise of specific team members and disciplinary diversity, the degree of specification of team member roles, and methods of communication (
15,
40 ).
Limitations
The study data are from 1997 and 1998, and the medical management of HIV has evolved since then. However, this study identified associations between medical clinic characteristics and access to specialist behavioral health services, and there is reason to believe that the findings remain relevant. Mental health problems and substance abuse are still common among persons with HIV, and access to behavioral health specialists is still poor for this population (
41,
42 ). Provision of mental health care and substance abuse care by medical providers has likely become more common in the past decade (
43 ). Recent studies indicate that mental health specialists may provide more intensive care than medical providers for mental health conditions (
43 ). Despite the likely increasing delivery of mental health and substance abuse care by medical providers caring for persons with HIV, access to mental health professionals and substance abuse treatment specialists will remain an important issue for a subset of this population with severe or refractory mental illness or substance use conditions.
The HCSUS also relied on self-report for measure of care use and substance use, was unable to adjust for impact of incarceration on abstinence, and lacked other drug outcomes, such as decreased use. HCSUS did not assess perceived need for care, and measures of objective need for mental health care and substance abuse care were based on survey responses, not clinical diagnoses.
Clinic data were unavailable for 82 of the 282 care sites, and nonresponse at the clinic level may have biased the results. It is possible that nonresponding clinics were more strained in their care mission and had fewer resources. The organizational characteristics under study may be less effective in these settings.
Conclusions
Although we observed significant associations between clinic characteristics and use of mental health care and substance abuse treatment, there likely were still patients with unmet needs for care, even in the best-performing clinics. Greater increases in use of mental health care and substance abuse treatment for this population may require more intensive quality improvement programs for mental health care and substance abuse treatment within HIV clinics (
44 ). These programs may include screening measures to detect patients with care needs, stepped collaborative care models with increasing interventions for patients with more severe or refractory conditions, use of treatment guidelines for specific conditions, and continuous monitoring of measures of care quality specific to mental health and substance use conditions (
44,
45,
46 ).
Acknowledgments and disclosures
This work was supported by grants from the Robert Wood Johnson Foundation and by grants R01-HS-1040802 and HS-102227 from the Agency for Healthcare Research and Quality.
The authors report no competing interests.