The changing role of public psychiatric hospitalization in the past 50 years has received much attention. As state and county facilities downsized (
1 ), the private-sector and general hospitals have been increasingly responsible for persons formerly served in public institutions, including persons with serious mental illness (
2 ). Less attention has been directed at characterizing the populations currently served by state hospitals. Focus in the United States has largely been on mental health among minority groups, as demonstrated by the Surgeon General's recent report (
3 ), and not on immigrant populations.
Considerable research in Europe, however, has indicated that compared with native-born persons, immigrants are more frequently hospitalized in psychiatric facilities (
4,
5,
6 ). Historically, high rates of mental hospital admission of foreign-born persons have been reported after waves of immigration to America, including the Irish in Massachusetts (
7,
8 ) during the mid-19th century and southern and eastern Europeans in New York in the early 20th century (
9 ). Foreign-born white adults formed about 20% of the general population in 1900 but more than a third of the resident inmates (
10 ).
More than 10% of the total U.S. population in 2000 consisted of immigrants (
11 ). In the past decade, states with large urban centers, such as New York, Los Angeles, Miami, and Chicago, have received large influxes of immigrants (
12 ). Illinois is one of a handful of states with more than one million foreign-born residents (
12 ). A substantial number of immigrants live below the poverty line and have either no benefits or very limited access to federal entitlements, including medical coverage (
12 ). Therefore, demand on state and local resources is frequently neither planned for nor budgeted. The heavy use of public services by low-income immigrants and refugees in California was estimated to cost about $1,200 per native household in 1996 (
13 ). Some jurisdictions have instituted measures to limit access to local public health and social services by undocumented persons (
14 ).
This study was designed to examine the impact of immigrants on admissions to Illinois state facilities over a ten-year period (1993–2003). We wanted to determine whether foreign-born persons, especially of Asian and Hispanic origin, were disproportionately hospitalized relative to their percentage of the general population and whether these rates changed over the ten years. We also compared possible demographic, social, and clinical differences between immigrants and native-born admissions. Because Mexican-origin immigrants constitute the largest foreign-born group in the state, we also compared this population with immigrants of a non-Hispanic background.
Methods
Data selection
The study involved an analysis of admission trends by immigrants to all Illinois state hospitals. Sufficient and reliable computerized data for birthplace have been available in the state hospital Central Information System only since 1992. Comparisons were made for three time points: 1993, 1998, and 2003. Because the research used only epidemiological data and no personal identifiers, the study was exempt and received expedited review by the institutional review board of the Division of Biological Sciences at the University of Chicago.
The data files contained auto-numbered listings of all first admissions and readmissions of adult persons with mental illness to each state-operated mental health facility in Illinois for 1993, 1998, and 2003. Each record included an individual's age, sex, race, marital status, education, final diagnosis (axis I and axis II), length of stay, birthplace, citizenship, primary language, English speaking (none, very limited, and limited), and Social Security number (yes or no). The initial admission was identified as the index episode, and readmissions across the study period were omitted so that each person in the final study sample was counted only once. Individuals who were under 18, had a developmental disability, or were admitted for forensic reasons were excluded.
Birthplace was missing from approximately 10% of the records for each time point, so all admissions for these individuals during the ten-year study period were scanned to determine whether birthplace was entered on another episode. If an answer was not supplied, the records were manually reviewed by two investigators because the records contained information regarding primary language, the level of English proficiency, country of citizenship, presence or absence of a Social Security number, and race. If the reviewers agreed that the patient neither spoke English nor was a U.S. citizen, the record was coded for a foreign-born patient without a designated country of birth. For example, many patients spoke only Spanish and were Hispanic, but a country of birth was not specified. Otherwise, patients with no listed birthplace were considered U.S. born.
Because 95% of the foreign-born admissions were from the six-county metropolitan Chicago area (Cook, Kane, DuPage, Will, McHenry, and Lake counties), we report our findings from just those counties (representing metropolitan Chicago). Similar findings emerged when the analysis included the entire state.
Data analysis
Multiple logistic regression analysis (
16 ) was used to examine trends in the proportion of psychiatric admissions of foreign-born patients. The unadjusted trend across time was examined with the Cochran-Mantel-Haenszel chi square test for trend (
17 ) and with the bivariate logistic regression model; the latter used a binary indicator for foreign born as the dependent variable and year as the independent variable. In addition the adjusted trend with foreign born as the dependent variable was examined by multiple logistic regression analysis.
Variables considered as additional independent variables for the adjusted time trend in a multiple logistic regression model included age at admission, gender, racial and ethnic background (black, white, Hispanic, Asian, or other), marital status (married or not married), education, first admission versus repeat admission, and primary diagnosis (coded into eight categories). Presumptively documented versus undocumented (no Social Security number), English language proficiency (no versus yes), and primary language were added to the analysis for determining differences between Mexican and non-Mexican foreign-born admissions.
Results
The foreign-born population in metropolitan Chicago (
18 ) grew about 45% (12.1% to 17.5%) between 1990 and 2000, whereas the proportion of foreign-born individuals admitted to state facilities, although increasing 80% (7.3% to 13.1%) between 1993 and 2003, remained below their percentage of the population. Immigrants of Mexican origin increased 94% (3.7% to 7.2%) between 1990 and 2000, and the proportion admitted more than doubled (2.0% to 4.4%) between 1993 and 2003 but remained below their percentage of the population. Likewise, during the same periods, immigrants of Asian origin increased 40% (2.8% to 3.9%) and the proportion admitted increased 64% (1.4% to 2.3%) but was still less than the percentage of Asian immigrants in the population.
The proportion of admissions who were foreign born was 7.3% in 1993 (505 of 6,907), 10.9% in 1998 (461 of 4,220), and 13.1% in 2003 (606 of 4,626). The adjusted trend across time was highly significant ( χ 2 =105.6, df=1, p<.001, Cochran-Mantel-Haenszel test of trend). The odds of being foreign born increased an average of 7.0% per year (odds ratio [OR]=1.07, 95% confidence interval [CI]=1.05– 1.08).
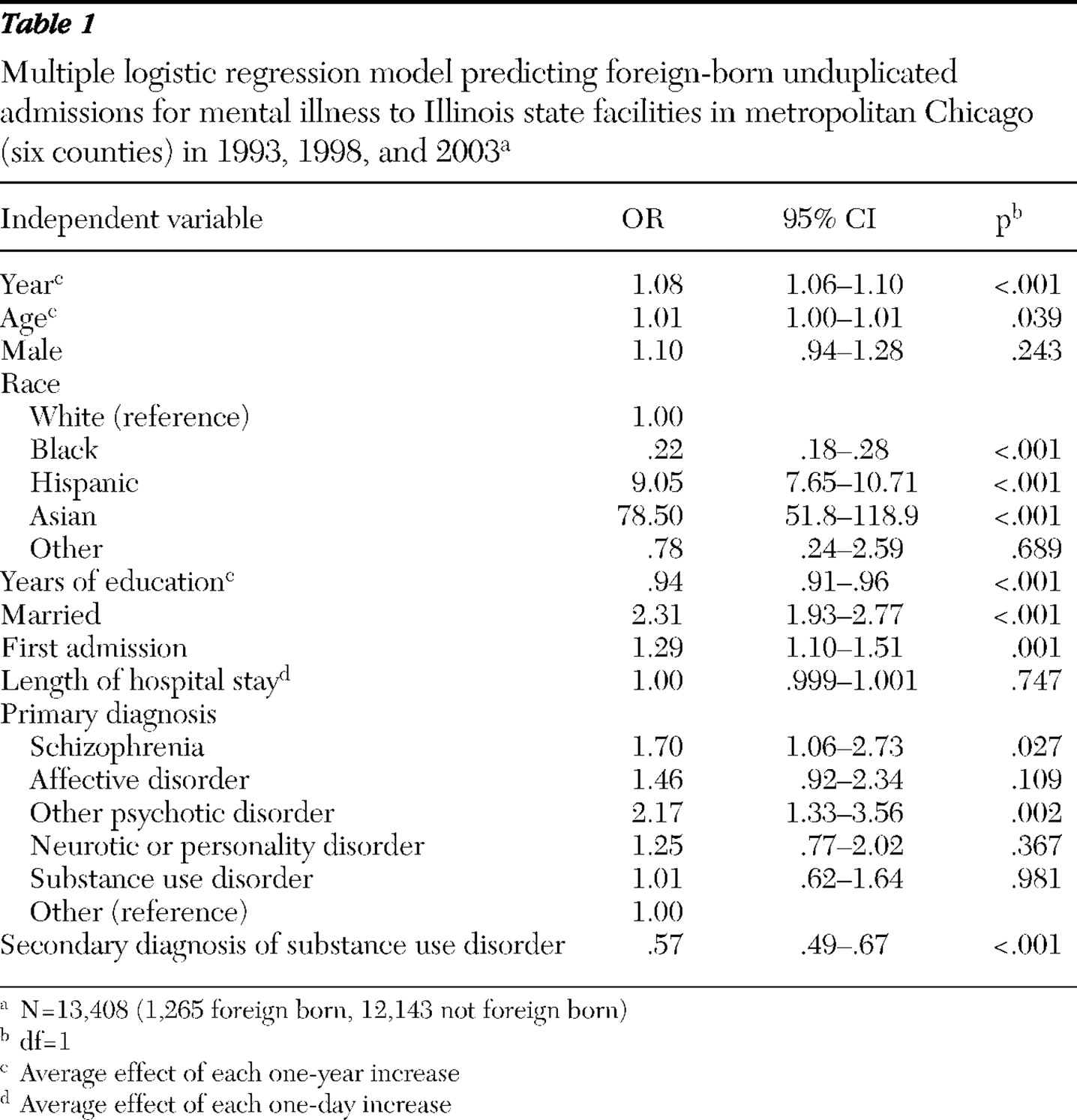
The adjusted trend across time remained significant, with an average increase of 8.0% per year in the odds of being foreign born (OR=1.08, CI= 1.06–1.10) (
Table 1 ). The odds of being foreign born increased with age and for married persons, first admissions, and persons with a primary diagnosis of schizophrenia or another psychotic disorder. Immigrants were considerably less likely than native-born patients to have a co-occurring substance use and mental disorders. They also were likely to be less educated. Compared with white patients, black patients were 80% less likely to be foreign born, whereas the odds of being an immigrant were nine times greater for Hispanics and 78 times greater for Asians.
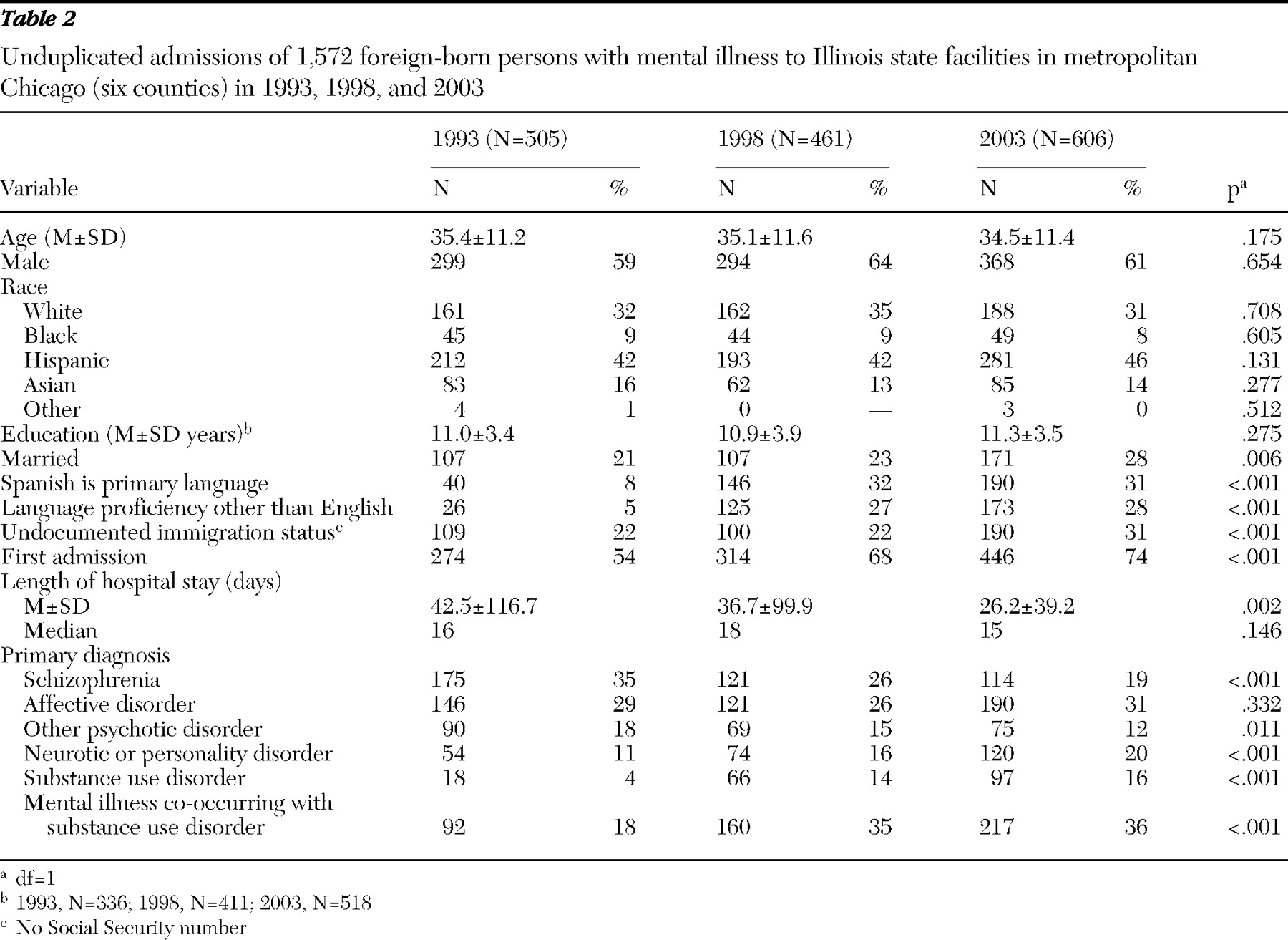
Analysis of change in the characteristics of immigrants revealed that the proportion of married persons among foreign-born admissions significantly rose during the study period, as did the frequency of individuals not proficient in English and whose primary language was Spanish (see
Table 2 ). The percentage of first admissions (54%– 74%) as well as the frequency of presumptively undocumented persons (22%–31%) also significantly increased. Consistent with overall state trends, schizophrenia and other psychotic diagnoses decreased while the frequency of nonpsychotic disorders rose. The percentage of co-occurring mental and substance use disorders also rose (18%–36%) among foreign-born admissions but remained lower than the rate for native-born admissions (30%–58%, data not shown). Length of hospital stay also considerably decreased over the study period.
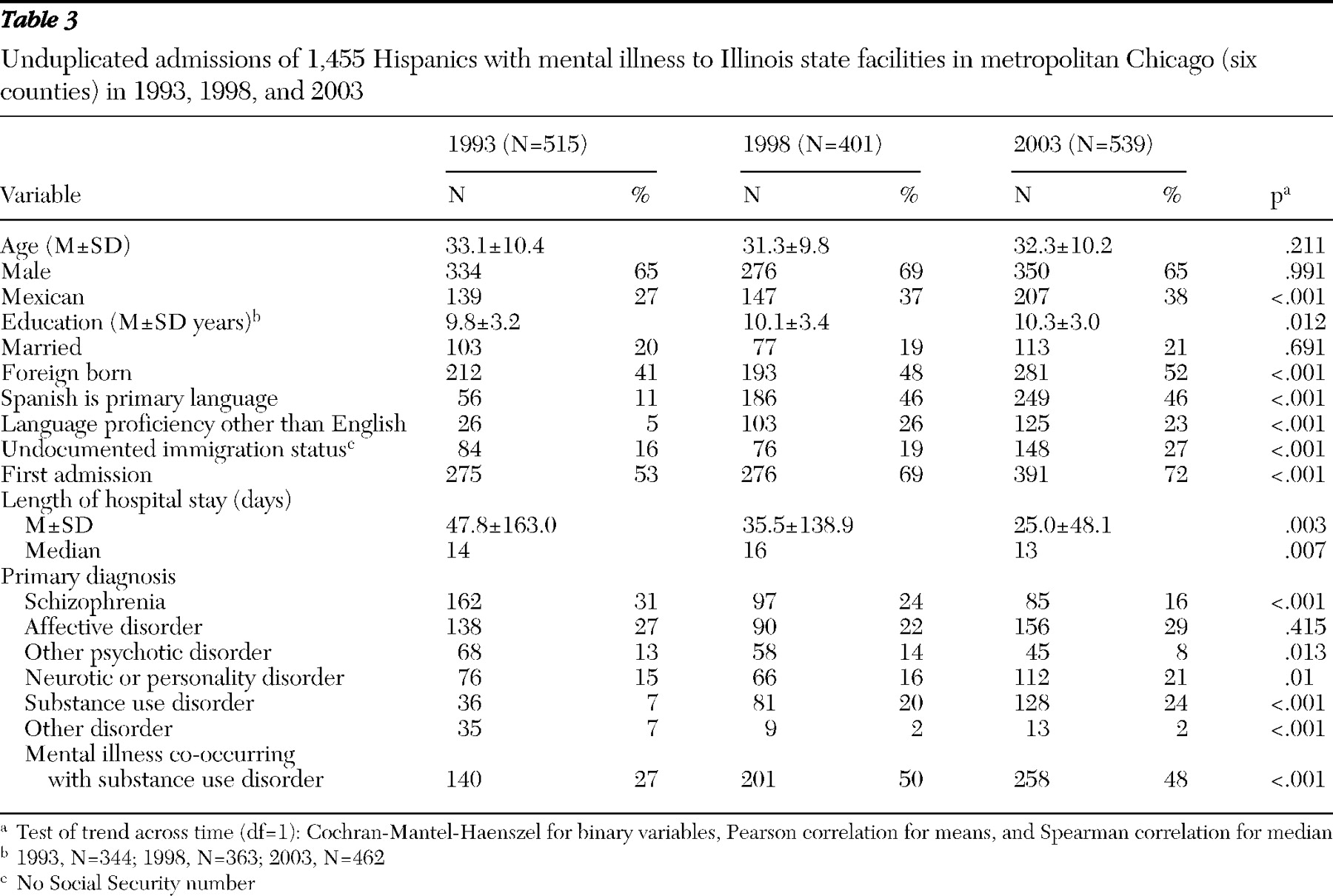
A similar analysis of change over time showed an increase in the number of Hispanic patients who were foreign born and an increase in foreign-born Hispanic patients who were first admissions (see
Table 3 ). The percentage who were of Mexican origin increased from 27% to 38%; the frequency of presumptively undocumented individuals rose nearly 70%. Both Spanish as the primary language and lack of English proficiency rose between 1993 and 2003 but were stable between 1998 and 2003.
Consistent with overall trends in metropolitan Chicago, the average length of hospitalization for Hispanic admissions decreased almost 50% during the study period. The significant decline in a primary diagnosis of schizophrenia and marked rise in substance use disorder during the ten-year period also paralleled diagnostic patterns for all patients (data not shown).
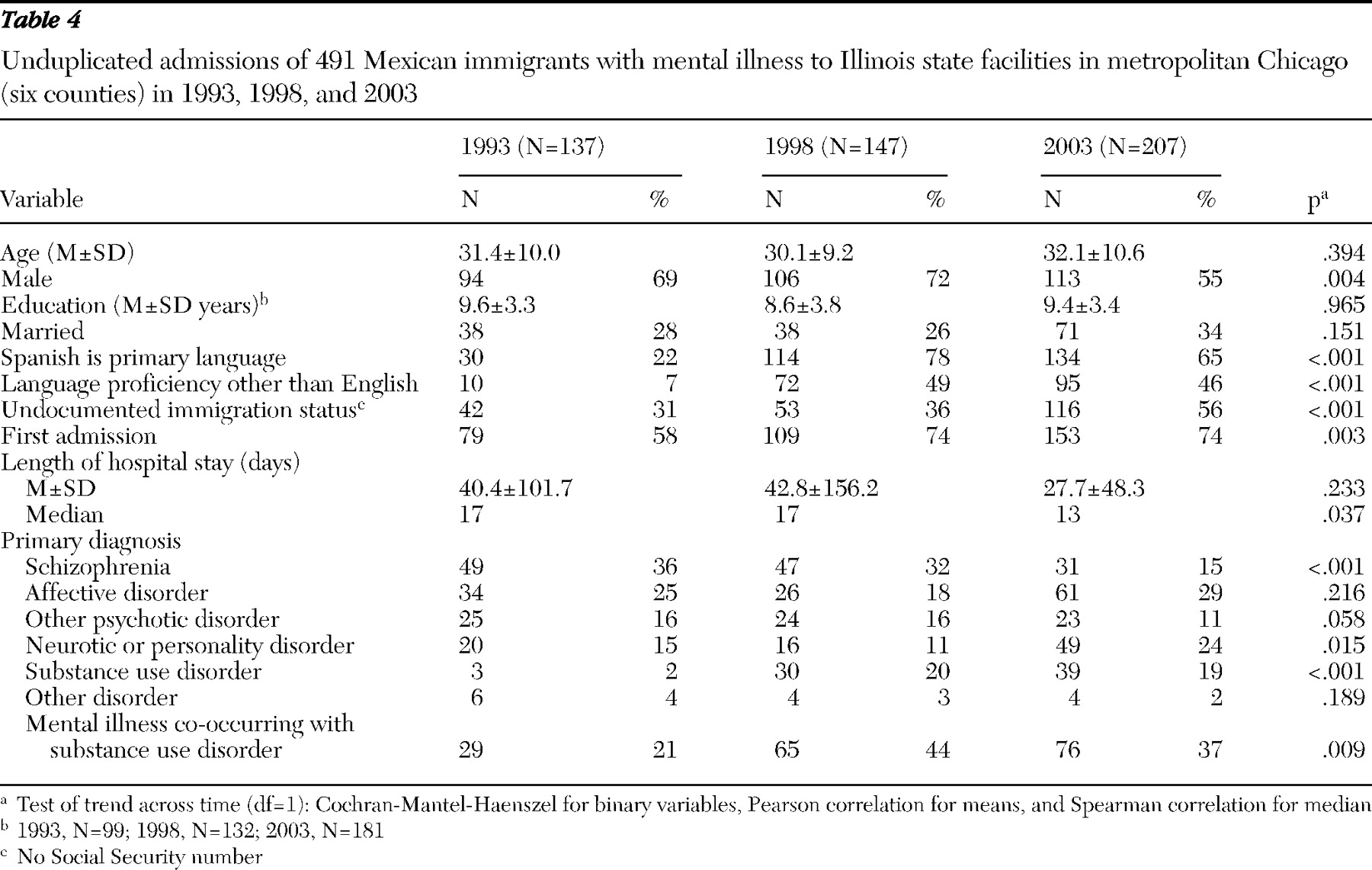
Because Mexican immigrants constituted the largest group of foreign-born admissions during the study period, we also examined the significance of trends across time for this population (
Table 4 ). The percentage that was male decreased, and the proportion admitted for the first time increased from 58% to 74%. They were more likely to have Spanish as their primary language and to be nonproficient in English. The rate of presumptively undocumented individuals rose 81% during the ten-year period and more than 55% between 1998 and 2003. Fifty-six percent of immigrants of Mexican origin admitted in 2003 did not have a Social Security number.
Paralleling overall trends in metropolitan Chicago over the ten-year period, our results showed that Mexican immigrants had briefer lengths of stay and were more likely to be diagnosed as having a neurotic or personality disorder or a substance use disorder than as having schizophrenia.
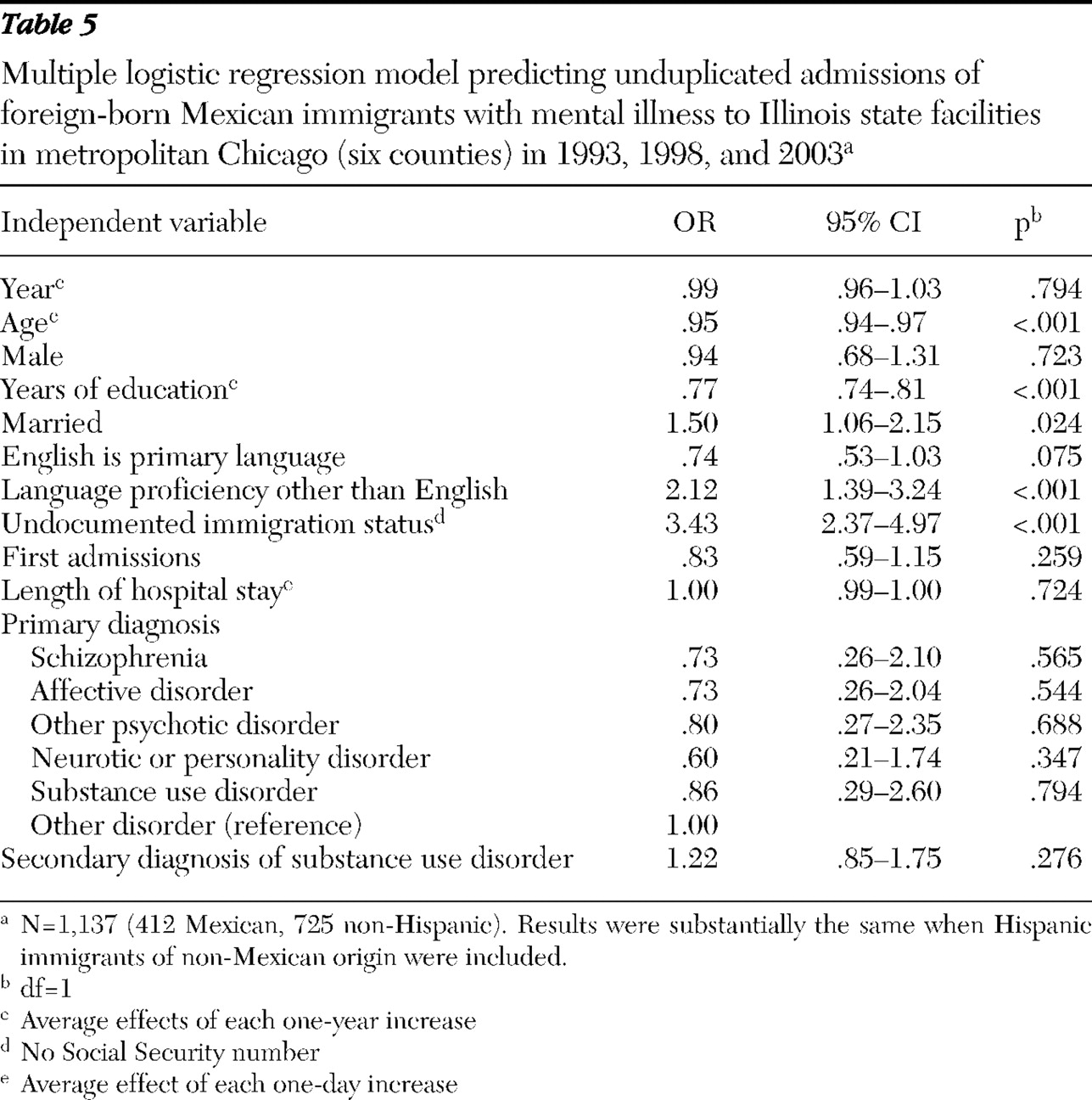
Although similar to non-Hispanic immigrants on most psychiatric variables, Mexican-origin immigrants significantly differed in other respects (
Table 5 ). They were younger and were more likely to be married and to have less education than other immigrants. Mexican immigrants also were more likely to be nonproficient in English and presumptively undocumented.
Discussion
Our findings indicate that compared with nonimmigrants, the proportion of immigrants admitted to Illinois state facilities has been steadily rising but is still below their representation in the overall population. These results are not in keeping with previous historical trends, when immigrants were disproportionately hospitalized for mental illness after a wave of immigration to the United States. The results are also in sharp contrast to numerous studies in Europe that report higher rates of schizophrenia (
6,
19,
20,
21 ), hospitalization (
4,
5,
6 ), and suicide (
22,
23,
24 ) among immigrants compared with nonimmigrants.
The obvious question is why the incidence of psychiatric hospitalization is not higher among immigrants in the United States with the recent immigration wave. The height of deinstitutionalization occurred between 1980 and 2000 (
1 ), so one possibility is that limited bed availability has reduced access for the foreign born to psychiatric hospitalization. But this seems less probable because the data indicate that foreign-born individuals are increasingly replacing native-born persons as the new entries into the public mental health system. More plausible is that differential rates of psychiatric hospitalization exist among immigrant groups. Studies in Britain (
5,
25 ) have shown that black persons from Africa and the Caribbean are more frequently hospitalized than native whites. However, admission rates, particularly for South Asians (India, Pakistan, and Bangladesh) and persons from Hong Kong as well as for Germans and Italians, are lower than rates for English-born persons (
25 ).
Certainly the transition to a new environment also is facilitated by the vast social and technological changes that have occurred since the previous immigration wave. Mass communication and globalization, for example, have reduced the size of the world as well as the strangeness and unfamiliarity of different societies, readily making known the unknown. Travel to America is considerably less of a hardship and strain today than it was 150 years ago. America is also changed and, compared with many European countries, is a multiethnic and multiracial society presumably more receptive to differences (
7 ).
The current U.S. immigration wave markedly differs from previous migrations in that it is predominantly from Latin America (largely Mexico) and Asia. European findings clearly support less stress and lower hospitalization rates for Asian immigrants (
25 ), and a recent epidemiological study has concluded that Asian immigrants are at lower risk of psychiatric disorders than U.S.-born Asians (
26 ), although there may be some gender differences (
27 ). Furthermore, risk of psychiatric disorder was found to be lower for Mexican immigrants than for persons of Mexican origin born in the United States (
28 ).
It was thus not unexpected that hospitalization rates for Hispanics and Asians in this study were less than their population representation. The reasons for underutilization may include less need, perceived barriers to access (
3 ), or preferred use of alternative services. Asians typically have higher incomes than most groups of new immigrants, so they may more often choose private medical treatment.
One implication of these findings is that immigrants from Mexico and Asia might be more adaptive and less vulnerable to stress than persons involved in earlier immigration waves. Some support for this selective-migration view is that the prevalence of psychiatric disorders among more recent Mexican immigrants in California was found to be lower than the prevalence among Mexico City residents (
29 ). One theory proposes that maintaining traditional values and close family ties among Mexicans insulates them against external stress (
30 ); other theories suggest that exposure to potential acculturation stress (achievement, for example) is actually minimized by lower expectations among recent immigrants (
28 ). In keeping with these ideas it has been shown that the risk of psychiatric disorder among immigrants, including Hispanics, increases with longer duration of U.S. residence (
31 ). With Mexican-origin immigrants increased tenure of residence also has been associated with increased risk of psychiatric disorders (
29 ), with urbanization and English-speaking proficiency especially increasing risk of illicit drug use (
32 ).
Foreign-born persons are contributing to changing populations of state hospital admissions in Illinois. They rose (80%) at a faster rate than their population growth in metropolitan Chicago during the study period and were about 30% more likely than natives to be first admissions. Consistent with census data (
12 ), our study showed that immigrants were more likely to be younger, married, and less educated. They more often received a psychotic diagnosis, a result similar to epidemiological studies in England (
33 ) but not in the United States (
28 ). Also striking is that foreign-born admissions were nearly half as likely to have co-occurring substance abuse as nonimmigrants, based on axis II substance abuse diagnoses.
Hispanics, predominantly of Mexican origin, are by far the largest ethnic-racial group of immigrants in Illinois as well as in the country. Almost 600,000 Mexican immigrants lived in the Chicago area in 2000, slightly more than 40% of the immigrant population (
18 ). Their proportion of the unduplicated foreign-born admissions gradually increased during the study period (27%–34.2%) and is steadily approaching their representation in the overall immigrant population.
Although there are similarities, there are important differences between Mexican and other foreign-born psychiatric patients, most notably the proportion of individuals whose immigration status is undocumented and who do not have proficiency with English (
34 ). Being undocumented has not been given much consideration in the literature and may be a contributing factor for low utilization of mental health services by Mexican immigrants (
3 ) but also may unduly contribute to stressful life circumstances (
35 ).
Why admissions of Mexican-origin immigrants proportionately increased over the study period is less understood. The average age of the hospitalized Mexican-origin immigrants did not increase over time, therefore eliminating the possibility that increased tenure of residence in this country (acculturation) increased the risk of psychiatric disorder and, inferentially, hospitalization. But other changes occurred. This population was more likely to be presumptively undocumented, more likely to have a substance use disorder, and more likely to be female, and individuals showed a complicated pattern of language proficiency.
Because undocumented immigrants usually do not have access to either private or public insurance benefits, they may have no other option but hospitalization in the public mental health system. Such an increase has been noted in Texas (
36 ). Second, the increase in substance use disorders, especially among men (data not shown), may reflect the corrosive effects of American culture (
33 ). Substance use problems are new in Mexican culture, and even brief exposure to alcohol and drugs in the United States has been shown to heighten the risk of substance use disorders (
37 ). Third, women accounted for a substantial proportion of the increase in Mexican-origin admissions and in 2003 approximated their proportion in the total population of foreign-born Mexicans. Finally, the rates of both Spanish as a primary language and nonproficiency with English rose dramatically between 1993 and 1998, but by 2003 the former decreased and the latter reached a plateau. This may suggest that a more rapid process of acculturation has started to occur.
An alternative hypothesis for the rise in admissions of Mexican-origin immigrants (compared with their proportion of the population) is that even if there are no changes in the degree of acculturation there may have been changes in the institutions that facilitate the individual immigrant's hospitalization (social service organizations, police, and so on). Whether such institutional changes have occurred is conjectural. Furthermore, the extent to which factors such as length of residence, being undocumented, exposure to alcohol and drugs, gender, and language have influenced these changing rates of public psychiatric hospitalization is an issue for further study.