In the Netherlands, the general practitioner acts both as a mental health care provider and as a gatekeeper. As a gatekeeper, the general practitioner can refer patients for mental health care that is more specialized. Over the past 20 years there has been an increase in general practitioner referrals to mental health services. In response the Dutch government has strengthened the general practitioner's gatekeeper function to manage and limit the ever-increasing number of people using mental health care services (
1 ). The government did this by specifying in the insurance guidelines that a specialist in nonacute care can start treatment only after receiving a formal written referral by a general practitioner. Yet general practitioners, already struggling with increasing workloads, needs of patients, and long working hours (
2 ), have tended increasingly to refer patients with mental health problems to mental health services (
3 ). This has resulted in long waiting times, poor continuity of care, and increasing dissatisfaction among patients, general practitioners, and mental health professionals (
4 ). To decrease both the workload of the general practitioner and referrals to specialized mental health services, various forms of collaborative mental health care have been introduced (
2 ).
Three collaborative care models have been described: the shifted outpatient clinic, the consultation liaison model, and the attached-mental health professional model (liaison attachment scheme) (
5,
6 ). In the third model, mental health professionals are attached to a primary care practice and operate as part of the extended primary care team, leading to co-located services. This model results in improved geographical convenience for patients, decreased stigma, increased ease of referral, increased communication, and better continuity and integrated care (
5,
6 ).
The literature concerning the feasibility and effectiveness of the various collaborative care models mainly addresses specific psychiatric conditions. Collaborative care interventions have proved to be effective in reducing psychopathology among persons with depression (
7,
8 ), including elderly persons (
9 ). Studies involving patients with psychosis, patients who abuse substances, and patients who use a high volume of mental health care have yielded mixed results. Studies of patients with anxiety disorders, personality disorders, eating disorders, attention-deficit disorder, and dementia are underrepresented (
10 ). Collaborative care studies of heterogeneous patient groups with common mental disorders are scarce. Only two randomized controlled trials, both carried out in the United Kingdom, have been conducted (
11,
12 ). The studies found a significant improvement in mean patient symptom scores, social functioning, and quality of life, with no significant differences between the usual and collaborative care conditions.
This study compared the effect of introducing collaborative care based on the attached-mental health professional model in a primary care setting in the Netherlands. We hypothesized that collaborative care would be at least equal to usual care regarding the effect on the psychopathology of patients, quality of life of patients, and satisfaction of patients and general practitioners, but it would be superior with regard to referral delay, duration of treatment, number of appointments, and related treatment costs.
Methods
Approval for the study was obtained from an Independent National Review Board for Mental Health (METIGG) in Utrecht.
Randomization
We invited all general practitioner practices in the Hague metropolitan area (126 practices with 240 general practitioners) that were not already participating in an ongoing collaborative care program to participate in this study. Of the 42 eligible practices, 15 declined to participate, and the remaining 27 practices (with 46 general practitioners) were randomly assigned to groups—14 practices were assigned to the collaborative care condition and 13 were assigned to care as usual. [A diagram showing the participating practices and number of patients referred to the trial is available as an online supplement at
ps.psychiatryonline.org .] In this cluster randomized controlled trial, practices were the unit of randomization (
13,
14 ). The practices (not individual patients) were randomly assigned to one of two conditions: either the practice continued its usual way of referring patients to specialized mental health services if indicated (usual care), or the practice referred patients to an on-site mental health professional who could see the patient for a maximum of five sessions (collaborative care). Between January 2003 and March 2005 all participating practices reported to the researchers all patients whom they intended to refer to a mental health organization.
Study population
Inclusion criteria for patients were age 18 or older, the presence of a mental disorder, and an indication for treatment that is more specialized. Exclusion criteria were dementia, delirium, acute severe psychotic symptoms, or a crisis condition demanding immediate care. The enrolled patients (N=165) reflect an urban population, and all were insured under the near-universal Dutch health insurance system. Of the 165 patients, 133 (81%) were native Dutch, ten (6%) were from Surinam, four (2%) were Turkish, three (2%) were Moroccan, and 15 (9%) were born in various other countries. According to the Mini International Neuropsychiatric Interview (MINI) (
15,
16 ), the study group consisted of a heterogeneous group with common mental disorders, mainly mood and anxiety disorders (
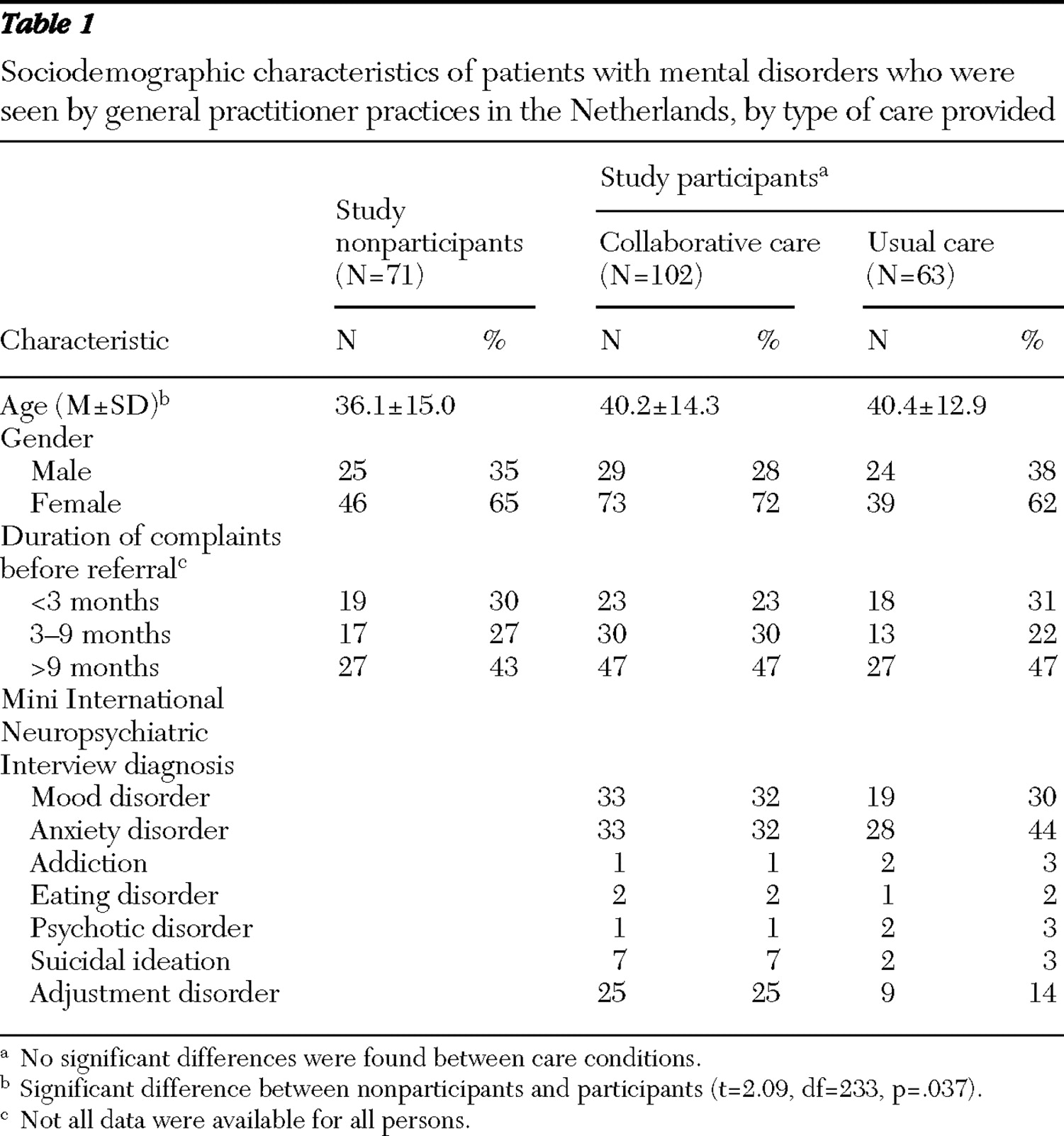
Table 1 ).
After oral and written information was presented to the patient, written informed consent was obtained. Neither patients nor general practitioners received financial or other incentives to participate.
Assessments
In this study the official Dutch version of the MINI 5.0.0. was used (
17 ). Patients were interviewed by an independent, well-trained research nurse. The Symptom Checklist (SCL-90) (
18 ) is a validated self-report inventory with 90 items measuring psychopathology during the previous week. The overall psychoneuroticism score was used (
19 ). The World Health Organization Quality of Life Questionnaire (WHOQOL-BREF) (
20 ) is a validated scale and produces scores in four domains related to quality of life and one domain referred to as the general evaluative facet, which describes overall quality of life and general health. The Dutch Mental Healthcare's "Thermometer of Satisfaction" is a widely used 20-item questionnaire that assesses patient satisfaction with mental health care received (
21 ). The general practitioner completed a Likert scale survey with four items indicating satisfaction with regard to time saving, workload relief, change in patients' complaints, and change in patients' quality of life.
At baseline, the MINI, SCL-90, and WHOQOL-BREF were administered. At three, six, and 12 months the SCL-90, WHOQOL-BREF, and patient and general practitioner satisfaction surveys were given. Waiting time between referral and the first face-to-face contact with a mental health professional (referral delay), duration of the treatment, and the number of mental health care appointments and their costs in Euros were assessed by telephone interviews with patients, by the electronic patient record system of the mental health services in the Hague, and by the rates provided by the Dutch Health Care Authority.
Interventions
In the collaborative care program, trained mental health professionals (community psychiatric nurses and psychologists) from mental health services had regular face-to-face contact with the general practitioner, consulted patients, and helped to refer patients in need of acute care. In the general practitioner's office, patients who were referred to the attached mental health professional received a short focused intervention consisting of a clinical assessment. This was followed by a maximum of four sessions based on cognitive-behavioral therapy and supporting principles (
22 ). A team of psychiatrists met face to face with the mental health professionals once a month and conducted regular meetings with the general practitioners. If indicated, patients could be referred to a specialized mental health care program after the initial clinical assessment with the mental health professional or at a later date.
Usual care involved the traditional referral of patients by the general practitioner, if indicated, to mental health services for treatment.
Analysis
Outcome measures included patients' psychopathology, patients' quality of life, patients' and general practitioners' satisfaction with care, system-related waiting time before treatment (referral delay), duration of the treatment, and the number of mental health care appointments and their costs in the 12-month follow-up after referral. For a study where the patients were randomly assigned to treatment, the Power and Precision software (Biostat) determined that 82 patients per condition should be needed to detect a clinically relevant difference in mean±SD scores between the two conditions of 22±50 points on the SCL-90 (power 80%,
α =.05). Taking into account an intracluster correlation coefficient (ICC) of .01 for the cluster randomization (
23 ), the needed sample size per condition was 85 to 89 patients.
Preliminary analyses included checking for selection bias and the computation of descriptive statistics, chi square analyses, and t tests to assess the comparability of study groups at baseline. Five patients (two in collaborative care, three in usual care) had no contact with any mental health service during the 12 months after referral by their general practitioner. These patients were included in the analyses (intention-to-treat principle).
A consequence of cluster randomization at the level of general practitioner practices (instead of at the level of individual patients) was a lack of independence for the outcomes of patients from the same practice. This means that outcomes for patients from the same practice were correlated—that is, nonindependent (
13 ). Ignoring clustering and dependence of outcome could create serious technical problems—for example, underestimation of standard errors and regression coefficients (
24 ). Therefore hierarchical linear modeling was chosen as the statistical method to resolve these issues (
24 ). Analyses were carried out with MlwiN 2.0 (
25 ). A hierarchical structure with three levels was identified in the data: each patient had several repeated measurements of outcomes, and several patients were referred by the same general practitioner. The repeated measurements per patient were assigned to level 1, the patients to level 2, and the general practitioners to level 3. Units at one level were grouped, or nested, within units at the next highest level.
In the analyses four dependent variables were used: the SCL-90 sum score as an indicator of overall psychopathology, WHOQOL-BREF general evaluative facet regarding quality of life, patients' overall satisfaction rating, and the mean score on the four items indicating general practitioners' satisfaction. These variables were analyzed separately; the satisfaction of general practitioners and patients was assessed at three time points, whereas psychopathology and quality of life were assessed at four time points. To examine the effects of the variables, a conceptual model for a general time effect was constructed. The relative effects of condition and its time effect were examined by entering them in the basic model. Variables resulting in a significant improvement of the conceptual model were retained. See Raudenbush and Bryk (
24 ) for a formal description of the analysis, or contact the authors of this article for more information.
Results
The 27 participating general practitioner practices used standard forms to identify for the researchers 236 patients who were eligible for inclusion in the study. Of these patients 165 consented to participate: 102 of the patients were being seen at practices in the collaborative care group, and 63 were from practices in the usual care group.
The imbalance between the two conditions with regard to the number of patients referred to mental health services is noteworthy. A difference in the number of referrals between the general practitioners practices was already apparent two years before the start of the study and persisted two years after the start of the trial. This consistency indicates that the difference is a reflection of a historical referral pattern and is not related to this study.
The 165 participating patients did not differ from the 71 patients who declined to participate in the study except in regard to age: participants were significantly older (40.3±13.7 versus 36.1±15.0 years). There were no differences between the usual care group and the collaborative care group on any of the other baseline variables (
Tables 1 and
2 ).
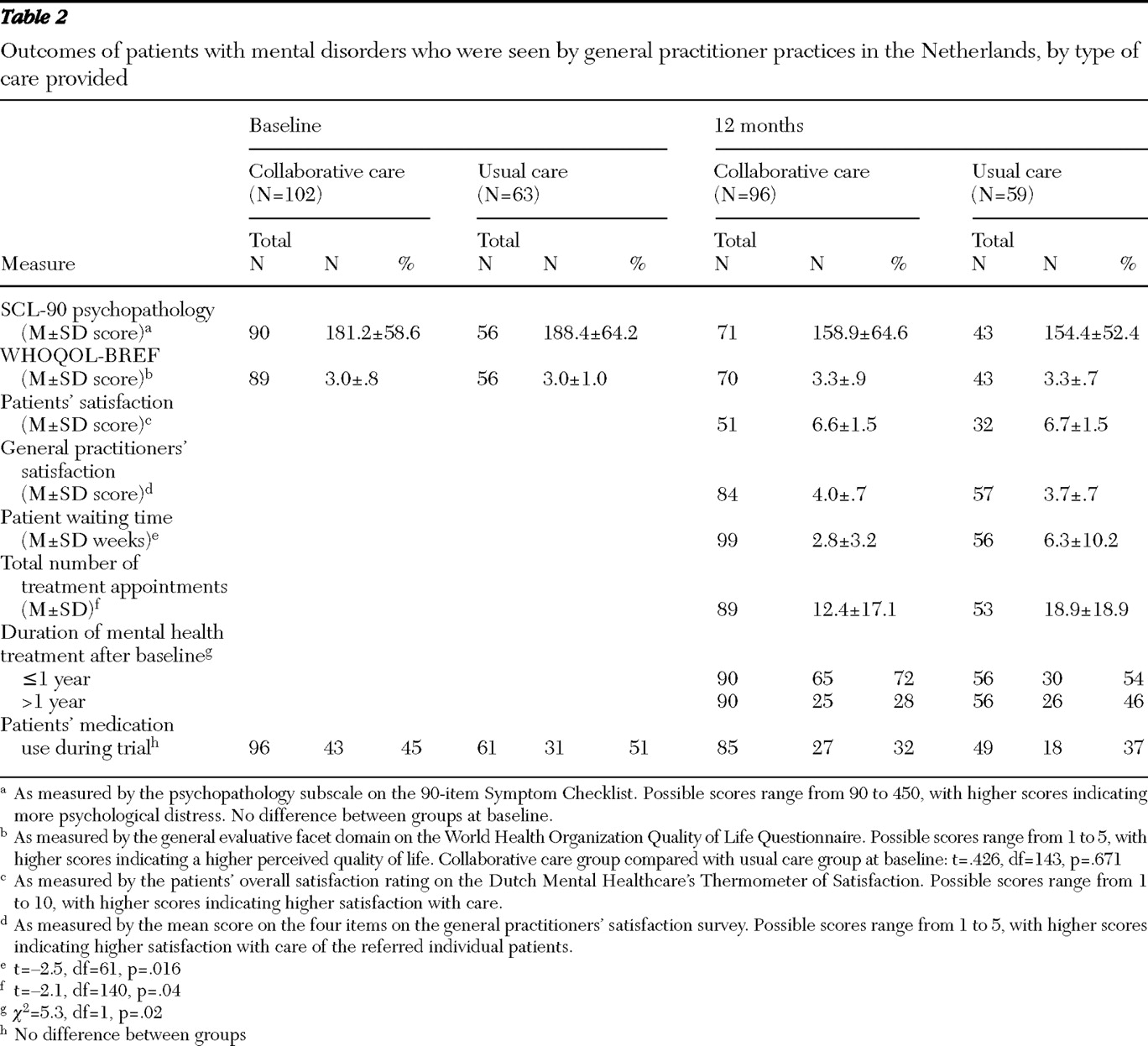
As shown in
Table 2, the number of patients using medication (antidepressants, benzodiazepines, analgesics, or antipsychotics) did not differ between conditions (collaborative care or care as usual) at baseline or at the end of the trial. The mean±SD waiting time for the first face-to-face contact with a mental health professional was significantly lower for collaborative care (2.8±3.2 weeks) than for usual care (6.3±10.2 weeks), according to a t test for independent samples. In the collaborative care condition, 33 patients (32%) were subsequently referred to specialized mental health care after one or more appointments with the mental health professional. For the patients who were subsequently referred, the mean number of appointments with the attached-mental health professional in the collaborative care group was 3.5±4.2. The patients who were subsequently referred to specialized mental health care by the collaborative care professional had an additional mean number of 21.7±24.3 appointments.
According to a t test for independent samples, the total mean number of appointments in the 12-month period was significantly lower in the collaborative care condition (12.4±17.1) than in the usual care condition (18.9±18.9). The mean cost for a patient in the collaborative care condition was €1,199±1,621, and it was €1,762±1,683 in the usual care condition. At the end of the 12-month period, significantly more participants from the collaborative care condition (N=65, or 72%) were no longer participating in treatment, compared with participants from the usual care condition (N=30, or 54%), according to a chi square test (
Table 2 ).
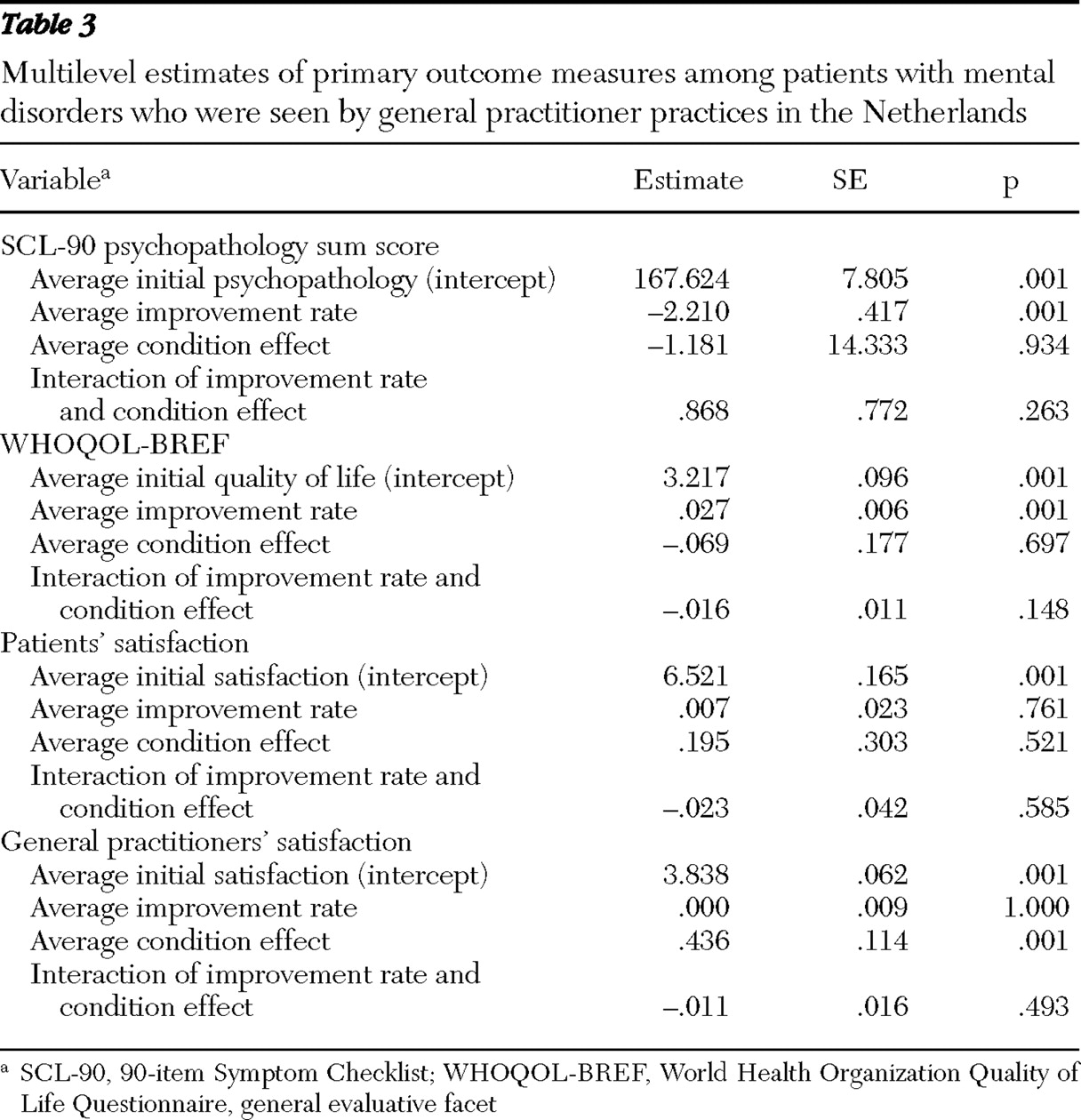
As shown in
Table 3, a significant improvement over time was found for both the SCL-90 psychopathology score (p=.001) and the WHOQOL-BREF general evaluative facet (p=.001). However, there was no significant difference between the two conditions, and there was no interaction effect between improvement and condition. Patient satisfaction showed no significant improvement over time, no condition effect, and no interaction effect between improvement and condition. General practitioners' satisfaction did not improve significantly over time, and there was no interaction effect between improvement and condition. However, a significant difference was found between the conditions. General practitioners from the collaborative care condition had a satisfaction score that was significantly higher than that of general practitioners from the usual care condition (p=.001) (
Table 3 ).
Discussion
We expected collaborative care to be equally or more effective than usual care in reducing psychopathology and increasing quality of life, patients' satisfaction, and general practitioners' satisfaction. We found that both collaborative care and usual care significantly reduced existing psychopathology, increased quality of life, and resulted in comparable satisfaction of patients. Collaborative care led to significantly higher levels of general practitioners' satisfaction and a significant reduction in referral delay and duration of treatment. A significant reduction of contacts with mental health organizations was achieved in the 12-month period, leading to a significant reduction in costs.
Our results are in accordance with the two randomized controlled trials comparing generic community mental health nursing care and problem-solving treatment with usual primary care (
11,
12 ). Problem-solving treatment is a brief (six session) structured psychological treatment that has been developed. In another pilot study, enhanced liaison between secondary mental health care and primary care teams did not lead to a significant difference in the reduction of symptoms, compared with standard care (
26 ). Although our study was slightly underpowered, the comparable effectiveness of both service models in decreasing patients' symptoms and increasing their quality of life may be a reflection of the high standard of primary care in the Netherlands. Consequently, it might be hard for an intervention to achieve significantly higher effectiveness than usual care (
1 ). Additionally, the fact that the care in the collaborative care condition was provided by mental health professionals trained and supervised within the context of a mental health organization might account for the comparability of outcome in both conditions. Of course it might also be a reflection of the natural course of the disorders, in which symptoms may improve over time.
There are limitations to this study. When the study started in 2003, about 65% of the general practitioners in the Hague area were already participating in the collaborative care program. The remaining general practitioners who wanted to participate first had to enroll in this study. This may have resulted in a bias, because being assigned to the usual care condition might have created dissatisfaction for the general practitioner involved. Also, the number of referrals per general practitioner practice in the usual care condition was substantially less than that for the collaborative care condition. However, when this number was compared with the referral pattern two years before starting and two years after the trial, there was no change in the number of patients referred. In hindsight, stratification by number of earlier referrals at the start of the study could have prevented the risk of a possible preexisting referral bias. The fact that patients from both conditions were comparable on all baseline variables indicates that the randomization at the level of the general practitioner practice resulted in a successful randomization at the individual patient level. Finally, this study cannot answer whether other collaborative care programs might be more or less cost-effective than this particular collaborative intervention.
A strength of this study is that randomization occurred at the general practitioner level. This design permits comparison of general practitioner practice referrals, rather than the individual course of treatment per patient. The high follow-up rate and low drop-out rate are indications of the quality of the trial management. Because patients in the study had various common mental disorders—the types of disorders that are regularly seen by general practitioners—the findings of our study are generalizable to other general practitioners.
This study is the first randomized controlled trial comparing collaborative care and usual care among patients in an urban environment. Results might be generalized to other urban settings and countries with similar health care systems, such as the United Kingdom, Spain (
27 ), and Canada (
28 ).
Conclusions
This trial provides evidence that collaborative care for patients with common mental disorders at the primary care level is feasible and as effective as standard mental health care. However, collaborative care results in significantly lower utilization of resources, as indicated by fewer appointments with a mental health professional, shorter treatment duration, and higher satisfaction among general practitioners.
Acknowledgments and disclosures
This study was funded by Delta Lloyd and OHRA Ziekenfonds, a health insurance company. The authors thank the patients and general practitioners, interviewer L. Dijkhuizen, M.Sc., the staff and management of the collaborative care program, and the Parnassia Bavo Group.
The authors report no competing interests.