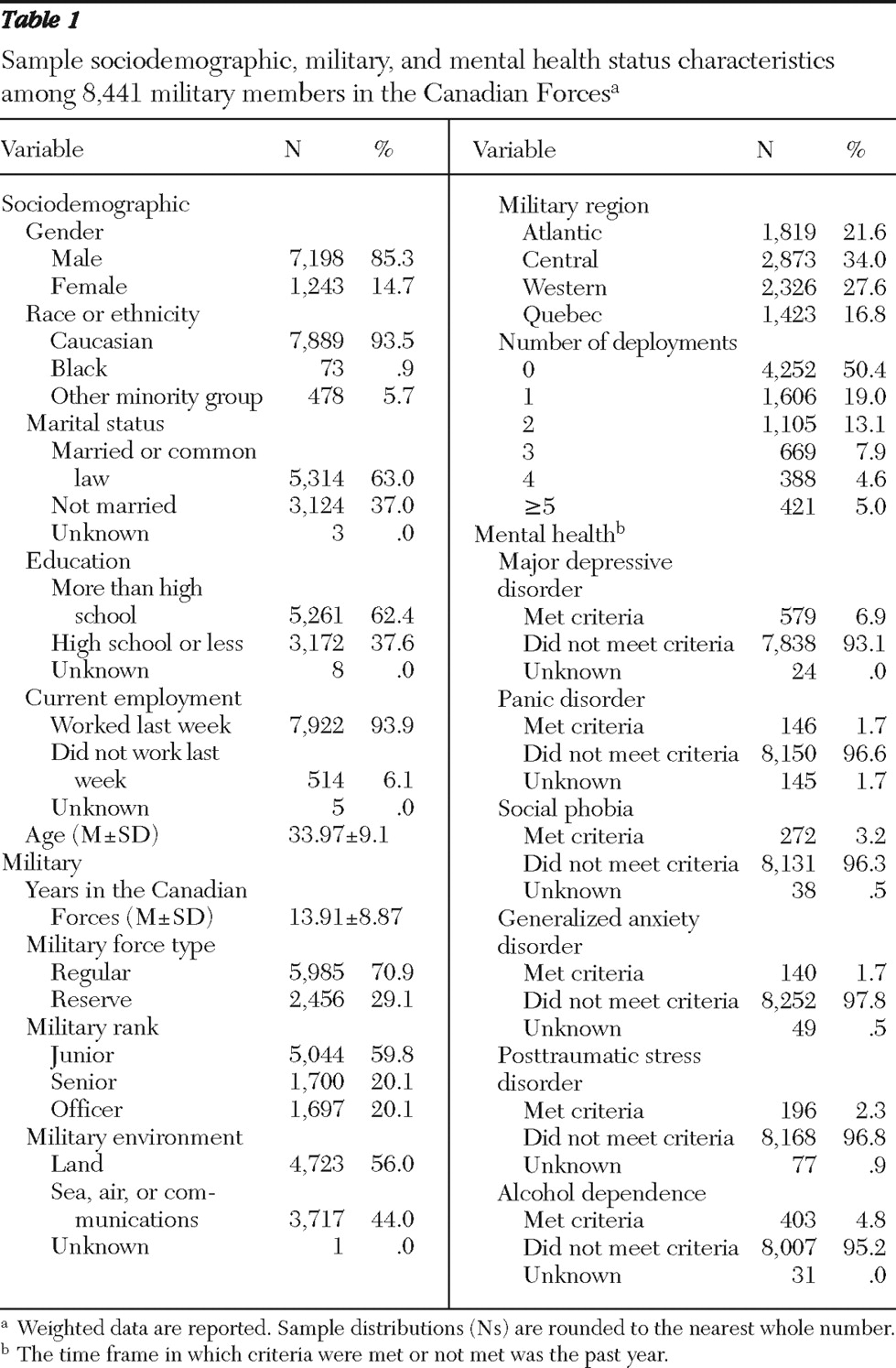
Descriptive analyses of past-year service use
Past-year service use was summarized here first for the whole sample (N=8,441); it was then summarized separately for those who met (N=1,220) or did not meet (N=7,221) criteria for at least one mental disorder in the past year. Of the whole sample, only 943 (11.2%) saw either a mental health professional or a medical professional in the past year. More military members consulted a mental health provider (N=767, 9.1%) than a medical provider (N=539, 6.4%). Of the whole sample, 395 (4.7%) had one to five visits, whereas 372 (4.4%) had six or more visits with a mental health provider. Of the whole sample, 361 (4.3%) had one to five visits, whereas 178 (2.1%) had six or more visits with a medical provider.
Of those who met criteria for at least one mental disorder in the past year, 472 (38.7%) saw either a mental health provider or a medical provider. More military members consulted a mental health provider (N=396, 32.5%) than a medical provider (N=324, 26.6%).
Of those who did not meet criteria for any disorder in the past year, 471 (6.5%) saw either a mental health provider or a medical provider. More military members consulted a mental health provider (N=371, 5.1%) than a medical provider (N=215, 3.0%).
Prediction of past-year service use
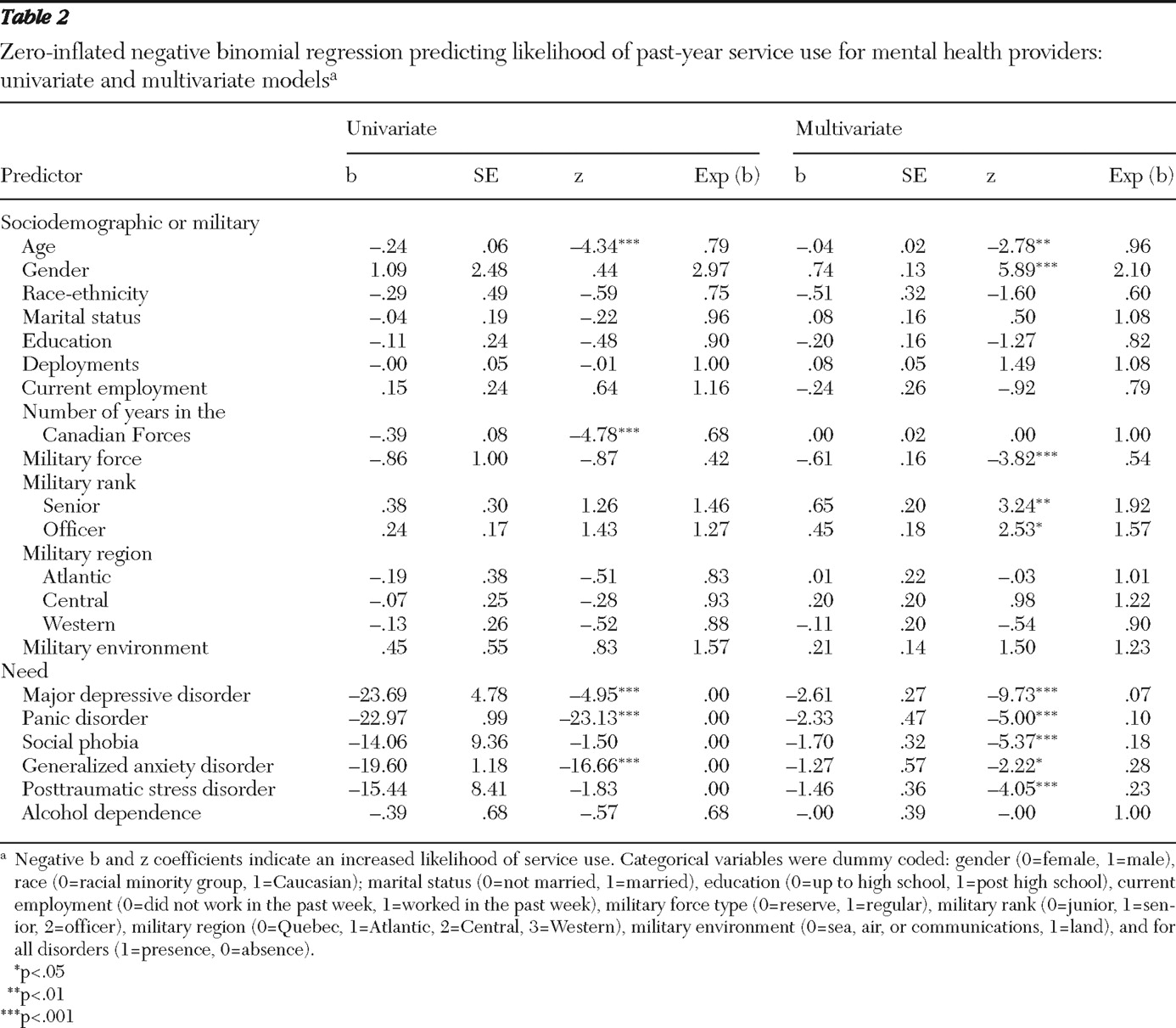
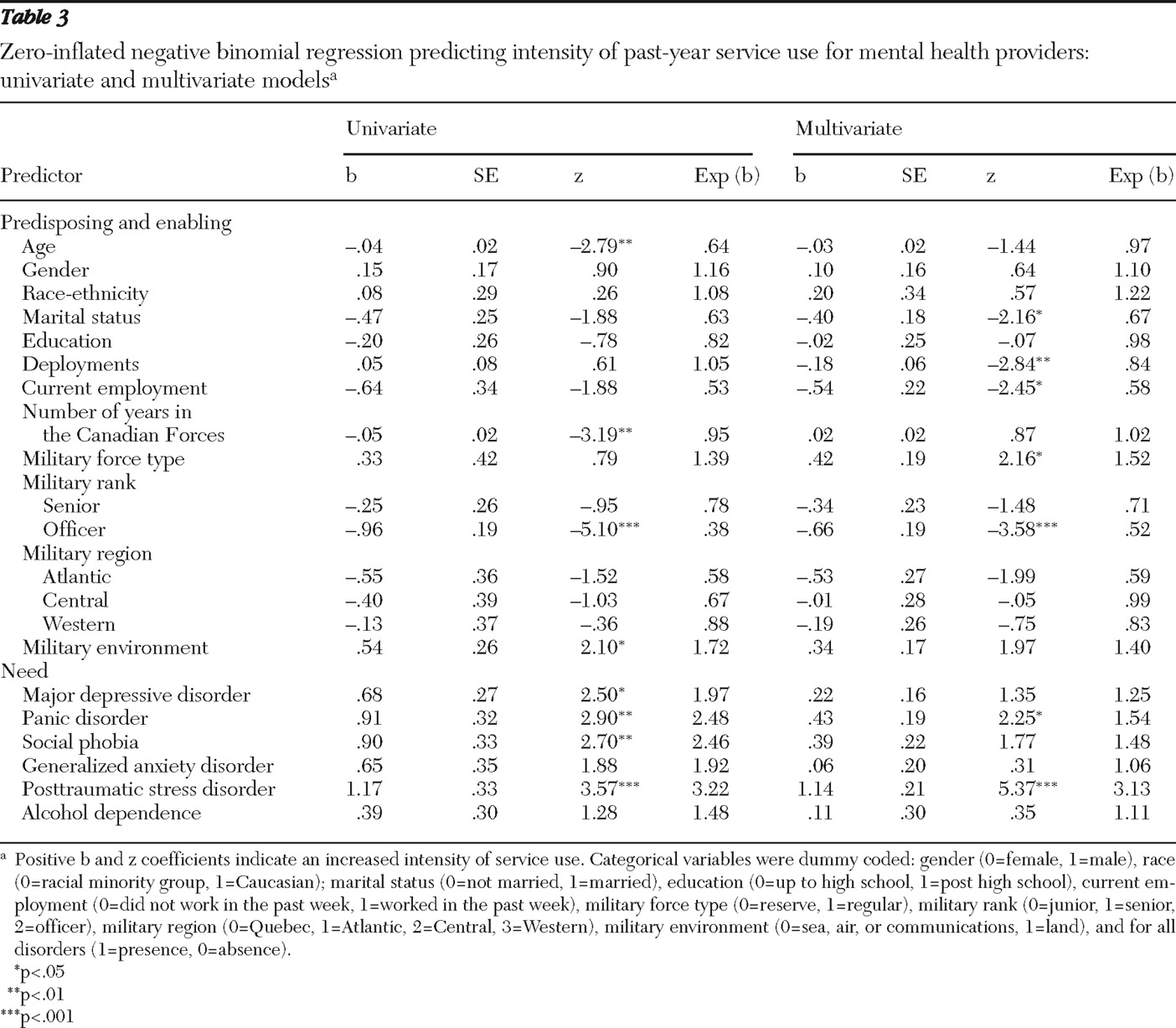
Univariate analyses: mental health providers. In univariate analyses to predict past-year service use versus nonuse (that is, service use likelihood) with mental health providers, the predisposing variables of older age and longer military service duration and the need variables of past-year major depressive disorder, generalized anxiety disorder, and panic disorder were associated with an increased likelihood of service use. In univariate analyses to predict service use visit counts (that is, service use intensity) with mental health providers, the predisposing variables of older age, longer military service duration, and lower military rank were associated with fewer visits, whereas the predisposing variable of being in the land troops and the need variables of past-year major depressive disorder, panic disorder, posttraumatic stress disorder, and social phobia were associated with more visits (
Tables 2 and
3 ).
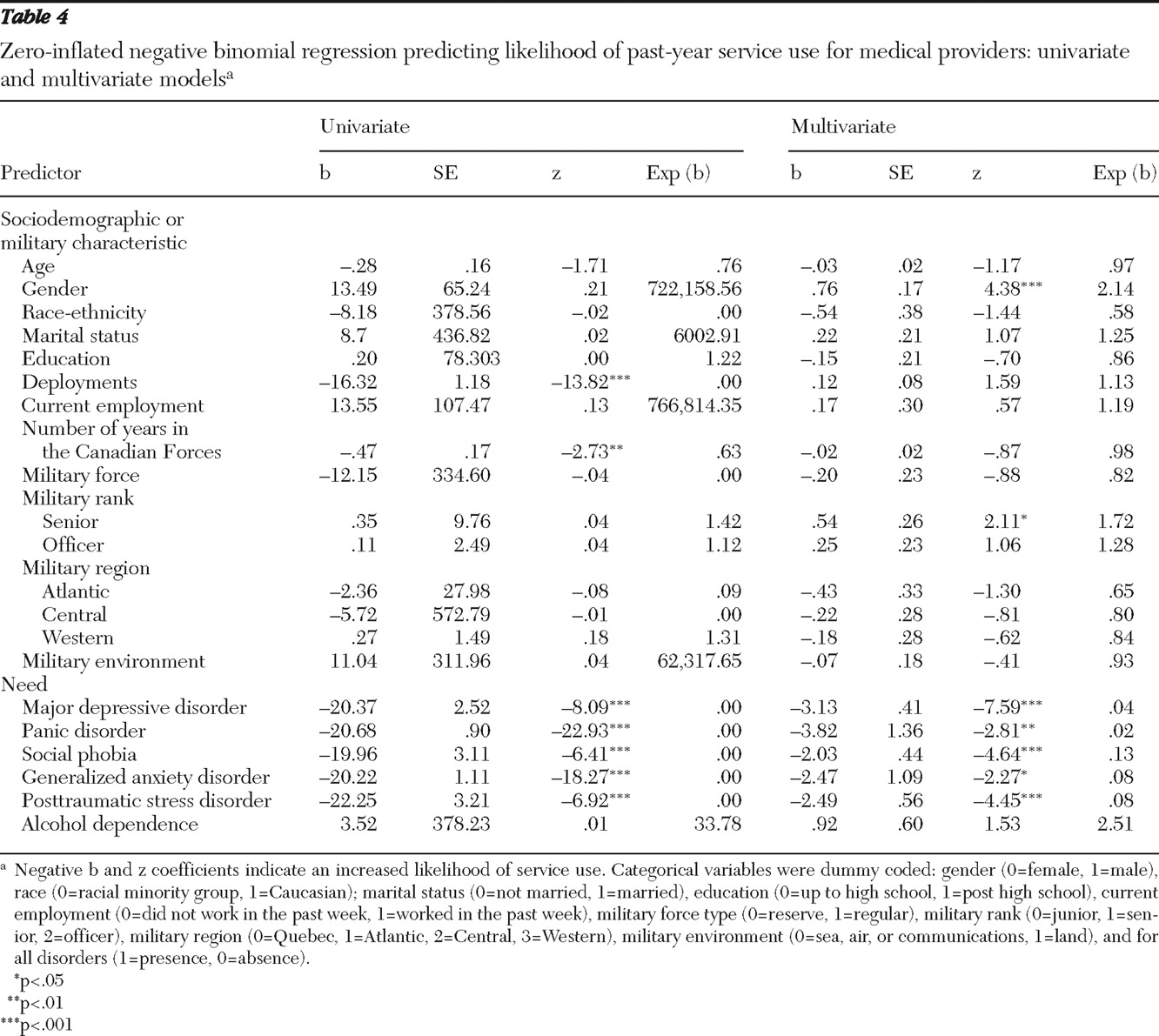
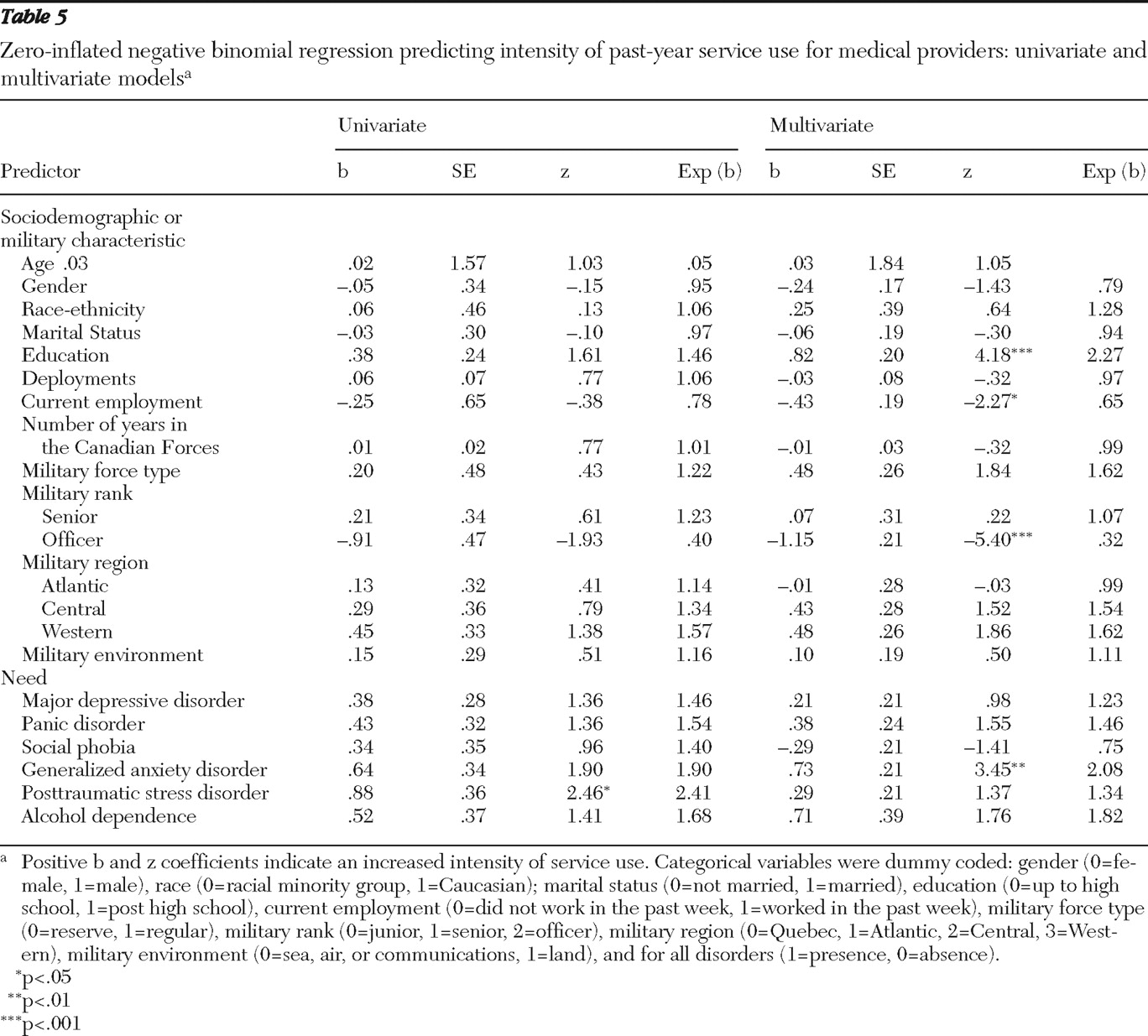
Univariate analyses: general medical providers. When using univariate analyses to predict service use likelihood with medical providers, we found that the predisposing variables of greater number of military deployments and longer military service duration and the need variables of past-year major depressive disorder, panic disorder, social phobia, generalized anxiety disorder, and posttraumatic stress disorder were associated with increased likelihood of service use. In univariate analyses for medical providers, only the need variable of past-year posttraumatic stress disorder was associated with more visits (
Tables 4 and
5 ).
Multivariate analyses: mental health providers. In multivariate analyses to predict past-year service use with mental health providers, the predisposing and enabling factors in step 1's overall ZINB regression model were significant ([N=8,092] likelihood ratio [LR]
χ 2 =267.16, df=31, p<.001), contributing 4.6% variance. Variables significantly associated with greater service use likelihood included being in the regular forces and lower military rank. Variables significantly associated with greater service use intensity included being unemployed, being in the regular forces and the land troops, and having a lower rank. Step 2 added a significant amount of variance (14.2%) ([N=8,092] LR
χ 2 diff =879.75, df=12, p<.001). Thus, the final model accounted for 18.9% of the variance in service use with mental health providers ([N=8,092] LR
χ 2 =1,146.91, df=43, p<.001). In the final model, older age, being in the regular forces, female gender, lower rank, past-year major depressive disorder, panic disorder, social phobia, generalized anxiety disorder, and posttraumatic stress disorder were all associated with greater likelihood of service use. Being in the regular forces, nonmarried status, fewer deployments, unemployment, lower rank, and past-year panic disorder and posttraumatic stress disorder were all associated with more visits (
Tables 2 and
3 ).
Multivariate analyses: general medical providers. In multivariate analyses to predict past-year service use with medical providers, step 1's overall ZINB regression model was significant ([N=8,092] LR
χ 2 =211.85, df=31, p<.001), contributing 4.7% variance. Significant predictors of greater service use likelihood included the predisposing variables of being in the regular forces and unemployment. Variables significantly associated with greater service use intensity included higher education and lower rank. Step 2 added a significant amount of variance (16.7%) ([N=8,092] LR
χ 2 diff =803.85, df=12, p<.001). Thus the final model accounted for 21.4% of the variance in likelihood of service use with medical providers [N=8,092]LR
χ 2 =1,015.69, df=43, p<.001). In the final model, female gender, lower rank, past-year major depressive disorder, panic disorder, generalized anxiety disorder, social phobia, and posttraumatic stress disorder were associated with greater likelihood of service use. Higher education, lower rank, unemployment, and past-year generalized anxiety disorder were associated with more visits (
Tables 4 and
5 ).