Study site and overview of programs
Supported independent living programs in Philadelphia began in 1987 when the city participated in the Robert Wood Johnson (RWJ) Foundation Program on Chronic Mental Illness. The initial allotment included 125 Section 8 housing vouchers to subsidize rents for persons with serious mental illness. From 1987 to 2002 the capacity of the supported independent living programs rose to 632 units through funding from federal, state, and local sources. In 2002 a total of 27 residential support teams provided services to residents to maintain independent living through skills development and by linking residents to community-based mental health services. Admissions were processed through a single-point-of-entry referral and placement unit, which conducted assessments and placements for all applicants to community residential programs (
22 ).
A variety of housing units were available for residents, including single-room-occupancy units, one- to three-bedroom apartments, and single-family homes. A majority (60%) of supported independent living residents in 2002 lived in rental units that were either owned by or leased through a quasi-government housing development agency established at the time of the RWJ program. The role of the housing agency was that of a regular property owner for persons with psychiatric and other disabilities; the agency was not involved in providing support services for its tenants. An equal proportion of residents lived in rental units that were owned privately and leased through residential support teams (20%) and in buildings that were owned by mental health agencies that also operated residential support teams (20%) (
22 ).
Although supported independent living programs provided long-term subsidized housing with support for independent living, access to and maintenance of housing was contingent upon sobriety, making these programs resemble the "treatment first" approach (
24 ). A majority (85%) of residential support teams instituted drug and alcohol testing for residents. Program rules and regulations were used to exert behavioral control over residents and facilitate treatment compliance. For example, more than one-third of the 27 teams required resident participation in house and community meetings, and one in five implemented a mandatory escrow policy for residents to put aside savings for future use. Despite these program requirements, residential support staff discouraged noncompliant and problematic behaviors, such as treatment noncompliance and potentially self-destructive behavior, but staff did not regard these behaviors as warranting immediate discharge from housing. A protracted process for working with "noncompliant" residents was generally put in place to avoid undesirable housing discharges.
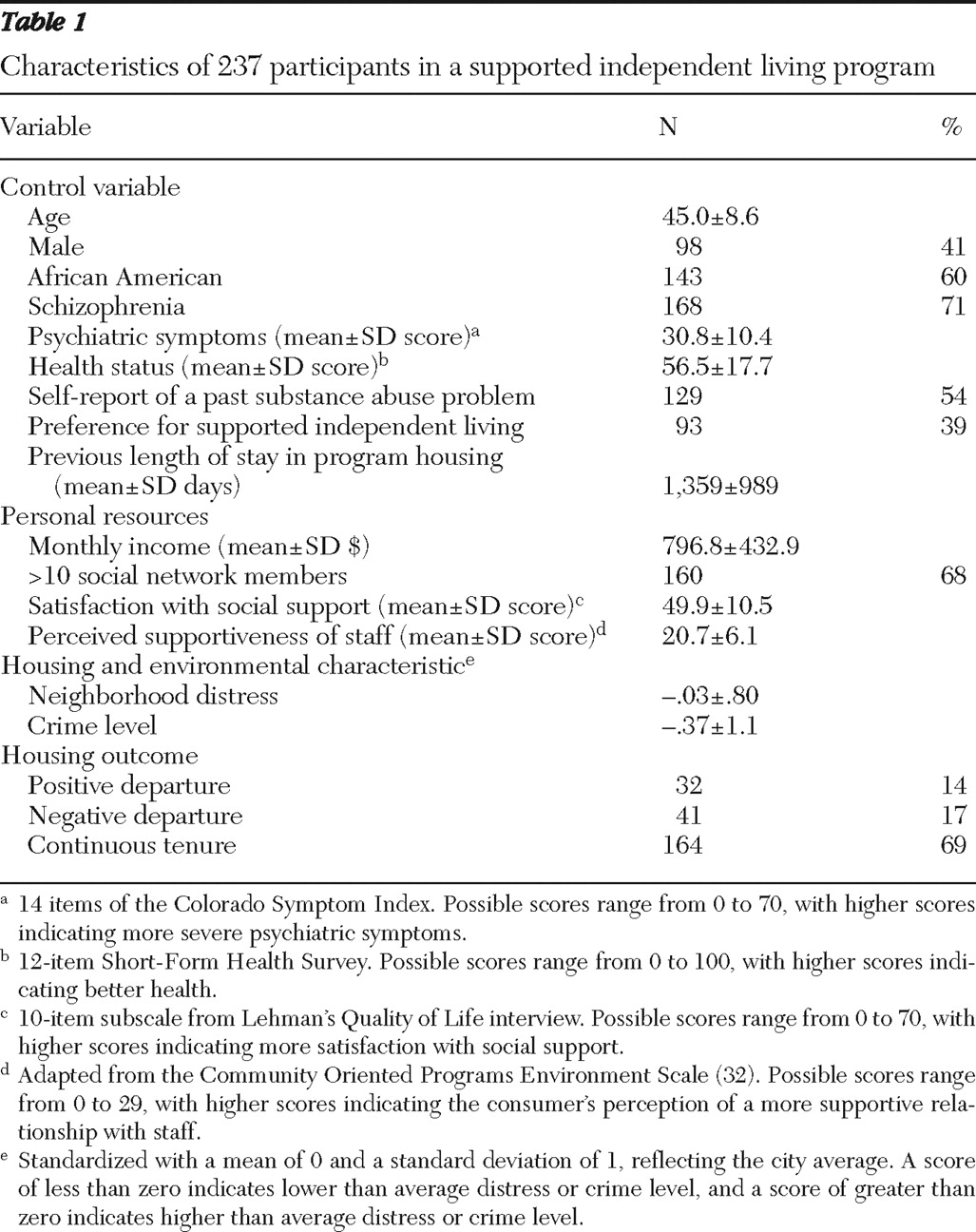
Measures
Demographic and clinical characteristics and control variables. Age was determined at the time of the interview. Gender, race (African American or other), psychiatric diagnosis (schizophrenia or other), and housing preference (yes or no) were all binary coded. Previous length of stay in housing provided by the supported independent living program was measured by number of days between the admission date and the interview date. Substance abuse history was measured by a one-item yes-or-no question in the original interview: "In your lifetime, have you considered your use of any substances on the list a major problem?" Substances on the list included alcohol, heroin, methadone, other opiates and analgesics, barbiturates, sedative-hypnotics and tranquilizers, cocaine and crack cocaine, amphetamines, cannabis and marijuana, hallucinogens, inhalants, and other substances. Severity of psychiatric symptoms was measured by 14 items of the Colorado Symptom Index (CSI), a self-report measure that has been found to be reliable and valid (
26,
27 ). Possible scores range from 0 to 70, with higher scores indicating more severe psychiatric symptoms. Self-reported health status was measured by the 12-item Short-Form Health Survey (SF-12), which is known to be a reliable and valid instrument for measuring functional health status (
28,
29 ). Possible scores range from 0 to 100, with higher scores indicating better health. These instruments were administered as part of the interview protocol in the parent study.
Personal resources. Income was measured as the total amount of money received from all sources during the past month. We included two aspects of social support—number of social network members as an objective dimension and satisfaction with social relations as a subjective dimension. Categories of relationship in the social network included spouse, partner, or significant other; family member; housemate or living companion; work, volunteer, or school associate; friend or acquaintance; group or organization member; service professional; and peer consumer. The number of social network members was dichotomized, with 1 indicating ten or more members and 0 fewer than ten members. Satisfaction with social relations was measured by a ten-item subscale from Lehman's Quality of Life interview, which has satisfactory reliability and validity (
30,
31 ). Possible scores range from 0 to 70, with higher scores indicating more satisfaction with social relations (Cronbach's
α =.89).
Supportiveness of the program's residential staff as perceived by participants was measured by an adapted version (29-item) of the Community Oriented Programs Environment Scale developed by Moos (
32 ) to indicate the extent to which the consumer-staff relationship is considered to be respectful, spontaneous, consumer-oriented, and proactive on the part of the staff. Possible scores range from 0 to 29, with higher scores indicating a more supportive relationship with staff as perceived by the consumer (
α =.88).
Housing environmental characteristics. To construct the measures of neighborhood distress and crime level, we extracted data from the 2000 Census data file on demographic, housing, and socioeconomic characteristics of 1,816 block groups in Philadelphia. A neighborhood distress score was derived by principal-components analysis reflecting the percentages in the block group with female-headed households with children under age six, households below 75% of the poverty line, vacant housing units, the unemployment rate for the block group, and households with public assistance income. From the same principal-components analysis, a crime factor score was derived, reflecting crimes against persons per 1,000 population and crimes against properties per 1,000 population.
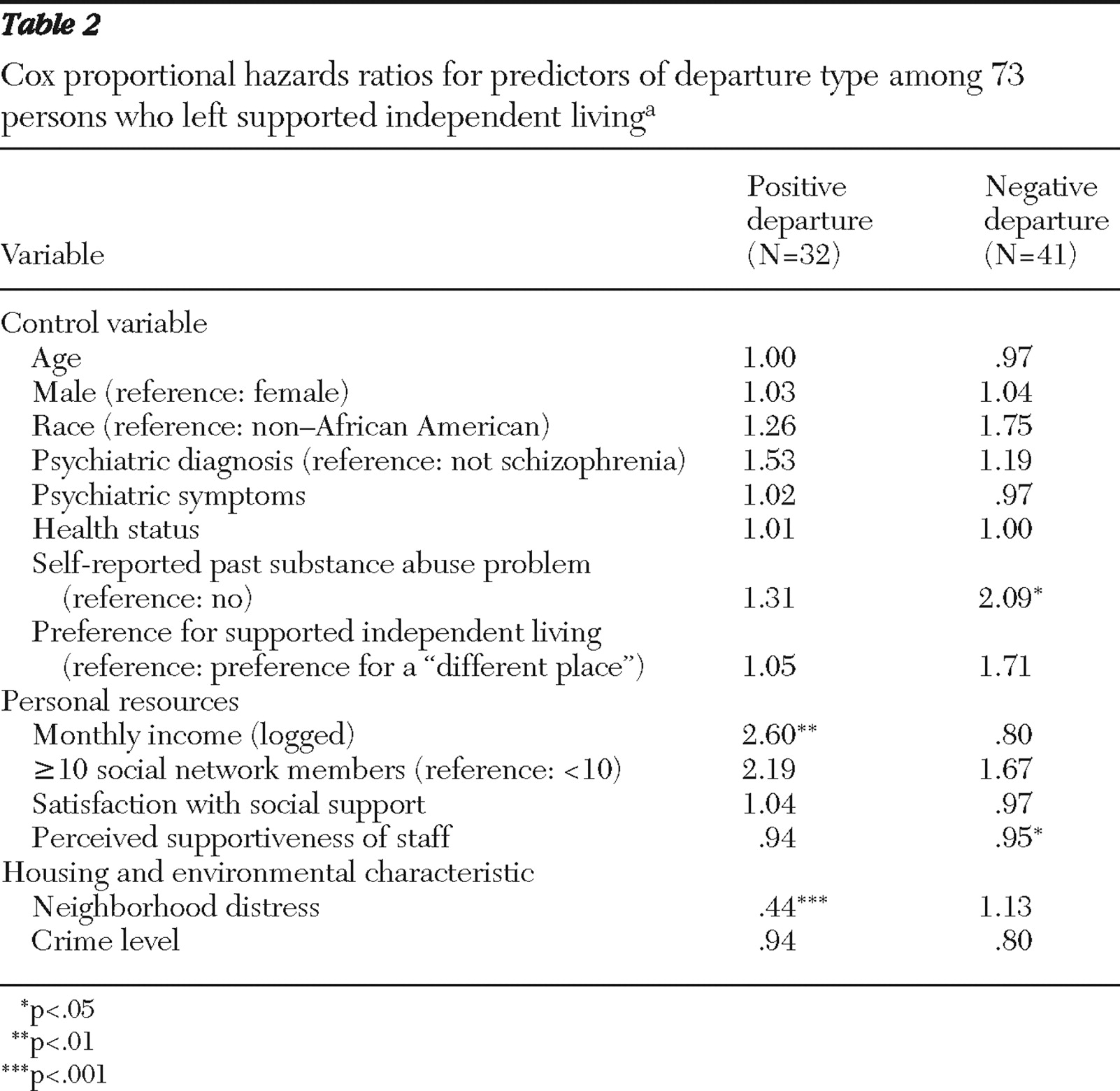
Housing outcomes. On the basis of the discharge codes reported in the administrative data, two types of housing departure were distinguished. Positive departure referred to moving to a higher level of independence, including living alone or living with a spouse in other subsidized housing, living in unsubsidized market-rate rental housing, and living in privately owned housing. Negative departure referred to leaving supported independent living for less independent settings, including those requiring higher intensity of care and institutionalized settings, or for unstable living arrangements, including nursing homes, psychiatric hospitals, congregate mental health residential programs, drug or alcohol treatment facilities, jails, or return to the streets or homeless shelters. To qualify as having departed, study participants had to have left supported independent living for 90 days or longer. This definition precluded temporary moves to other housing settings that were followed by a return to supported independent living.
Creating the housing outcome variable required quantifying the length of time each participant stayed in supported independent living. For persons who departed, length of stay was computed as the difference between date of admission to supported independent living and date of discharge. For those who remained in supported independent living through the end of the study, length of stay was computed as the difference between date of admission and date at the end of the study, or 30 months after the interview date. To capture the three housing outcomes—two types of departure and remaining in the program—an indicator variable was constructed for each participant, coded 1 for a positive departure, 2 for a negative departure, and 0 if the participant remained in supported independent living throughout the study period.