Individuals with serious mental Illnesses who are being discharged from inpatient settings and remain unconnected to outpatient treatment services are at a higher risk of recidivism. After discharge, psychiatric patients are at high risk of adverse outcomes, including psychiatric rehospitalization (
1,
2 ), first-episode or recurrent homelessness (
3,
4 ), violence against others (
5 ), and suicide (
6,
7 ). Delayed or absent outpatient follow-up psychiatric treatment contributes to poor outcomes (
8,
9 ). Recent estimates suggest that only half of all discharged psychiatric patients transition successfully to outpatient care (
10 ).
The most effective type of bridging strategy involves coordination of ongoing treatment between inpatient and outpatient staff. Patient telephone contact predischarge with outpatient clinicians predicts outpatient follow-up for patients assigned to receive outpatient psychiatric care from new clinicians (
11 ). Communication about patients' discharge plans between inpatient and outpatient clinicians, patients' attendance at outpatient programs before discharge, and family involvement during the hospital stay are associated with outpatient follow-up (
12 ).
This study assessed the effectiveness of a brief critical time intervention (B-CTI) model for veterans with serious mental illness who were being discharged from inpatient psychiatric treatment facilities. CTI was originally a nine-month model designed to prevent recurrent homelessness among men with mental illness who were being discharged from homeless shelters (
13 ). The original CTI model was effective at reducing extended homelessness and negative symptoms (
15 ), and it was cost-effective in comparison to usual care (
16 ). CTI has subsequently been adapted for other populations, such as homeless persons with mental illness who are being discharged from psychiatric hospitals, homeless families, homeless veterans, and men with mental illness who are being discharged from prison (
17 ). We shortened and adapted the original CTI model, creating a brief three-month intervention that seeks to enhance continuity of psychiatric outpatient care. We hypothesized that veterans randomly assigned to receive B-CTI would have significantly better continuity of care.
Methods
Settings and design
The study site was the Department of Veterans Affairs (VA) Capitol Healthcare Network, which includes four acute inpatient units (two of which are linked in one health care system). Baseline assessments were completed between February 2003 and April 2005. Consenting veterans who met study inclusion criteria and who were being discharged from the acute inpatient unit were randomly assigned to receive B-CTI or usual care. Participants completed an in-person interview conducted by a rater who was blind to the study condition at baseline and three months later. Chart reviews provided service utilization data.
Participants
Participants were eligible for the study if they were 18 to 70 years of age, lived within 50 miles of the inpatient facility, and were diagnosed as having a schizophrenia spectrum disorder, major depression, bipolar disorder, or psychotic disorder not otherwise specified. Participants were determined to be at risk of dropping out of treatment after the index hospitalization if they were diagnosed as having a co-occurring substance use disorder in the year before the index admission, had a history of medication nonadherence in the year before the index admission according to patient self-report or chart, or had an inpatient admission during the two years before the index admission, followed by a readmission, an emergency room visit, or no outpatient visits within 30 days postdischarge. Patients who were homeless or currently receiving or eligible for services from the mental health intensive case management team by virtue of four or more psychiatric inpatient hospitalizations within the past year were excluded.
Differing institutional review board requirements across settings created two different procedures for participant screening and recruitment. Review of inpatient logs identified all patients who met age and diagnosis criteria. Two sites permitted screening the charts of persons meeting age and diagnosis criteria to determine whether they met other inclusion criteria. Persons meeting eligibility criteria were approached for consent. Two other sites required participants' verbal consent before chart screening. The same procedure was followed in these two sites after obtaining verbal permission.
A total of 211 inpatients were eligible for the study and were approached, and 155 (73%) provided written informed consent after receiving a complete study description. Persons who consented to participate did not differ on the basis of age or race from those who refused; women were less likely than men to refuse participation (p<.05). Twenty patients were withdrawn from the study immediately after they provided consent—15 became ineligible as a result of changes in discharge plan or changes in diagnosis, and five had such rapid discharge that no assessments were completed—leaving 135 enrollees (61 participants at the linked sites 1 and 2, 27 participants at site 3, and 47 participants at site 4). A total of 116 participants received three-month evaluations. Gender, race, and age did not differ significantly between those who completed the follow-up assessment and those who did not. Medical charts provided service utilization data for the six-month period postdischarge.
Intervention description
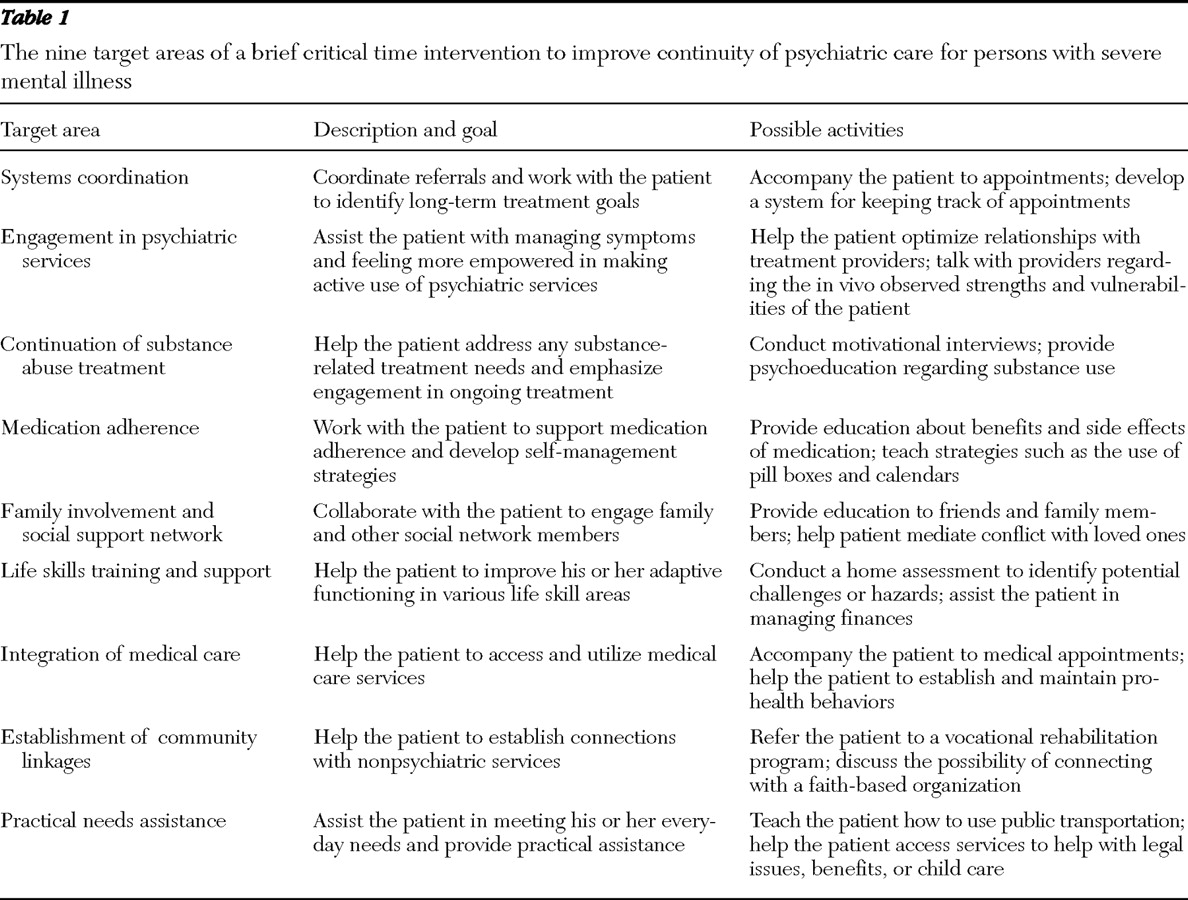
This study's adapted B-CTI model roots patients within existing systems of community-based services and social support, thereby facilitating the transition from inpatient hospitalization to outpatient services and community living. The three-month intervention begins before hospital discharge. The B-CTI clinician, who has training in nursing or social work, receives a referral and immediately meets with the patient to assess individual needs and barriers to outpatient care. The clinician builds rapport, develops individualized treatment goals, identifies barriers to treatment, and establishes a case management plan. There are nine possible target areas for clinical focus (
Table 1 ). The focus areas are determined by the initial assessment and ongoing reappraisal of the patient's needs. Clinicians are trained to emphasize systems coordination and psychiatric stabilization and to identify an additional two to three target areas. The three phases of the original CTI model were reduced to two in B-CTI; the phases are labeled bridging the transition to outpatient care and facilitating engagement in community-based services.
After discharge, the B-CTI clinician maintains a high level of patient contact, conducting home visits, accompanying the patient to initial appointments, and providing emotional and practical support for the patient and family. During the first 30 days after discharge, the B-CTI clinician had a mean±SD of 4.95±3.03 patient contacts. Contacts during the entire period of B-CTI averaged 12.67±7.93.
The comparison condition consisted of referral to outpatient treatment, partial hospitalization, and substance abuse treatment according to each unit's usual practices. There was no formal care coordination beyond the point of referral.
Fidelity
B-CTI clinicians were drawn from existing clinical staff at each site. One clinician covered sites 1 and 2. Clinicians completed a two-day training session to review B-CTI's essential elements and manual. Clinicians had biweekly telephone supervision.
Fidelity was assessed by review of all B-CTI chart notes by coinvestigators. Clinician ratings of focal priorities were extracted. Evidence of whether the B-CTI clinician addressed each priority focus area and the overall extent to which services were consistent with the model were evaluated using information from chart notes and the clinical supervisor. Study coinvestigators AL and RG, who played a key role in the manualization of the intervention and who also oversaw provider training, discussed each case and arrived at a consensus. Ratings ranging from 1, not at all, to 5, very much so, were given for each of the five key process variables (see below). A summary index variable representing overall process implementation fidelity was created by taking the average across the five ratings.
Assessments and variables
Mental disorder diagnoses made by the inpatient treating psychiatrist were obtained for descriptive purposes. All participants were assigned to the category of schizophrenia and other schizophrenia spectrum disorders or to mood disorders.
Service utilization variables were dependent measures and were obtained through medical chart abstraction spanning the six months after index hospitalization. Use of acute and subacute services, including days of inpatient hospitalization, number of emergency room visits (psychiatric and somatic), and days of partial hospital program use were recorded. We recorded use of nonacute services, including every mental health, substance use, and general medical outpatient visit, and the associated provider. B-CTI clinicians were considered members of the mental health team.
Primary outcomes were based on VA performance measures and included measures of continuity from inpatient care to outpatient care, continuity of outpatient care, and outpatient treatment intensity. We constructed five dependent variables (key process variables) assessing inpatient to outpatient care continuity and treatment intensity. The first variable was the number of days until the first mental health or substance abuse outpatient visit. The second and third were the proportion of patients who received any mental health or substance abuse outpatient treatment during the first 30 and 180 days after discharge. The fourth was the number of mental health or substance abuse outpatient visits in these intervals. Finally, the fifth variable indicated outpatient continuity of care: we assessed the number of two-month periods during the first six months after discharge in which the veteran had two or more outpatient mental health or substance abuse visits. If the veteran had two visits, he or she received a score of 1 for that period; if not, the veteran received a score of 0. Veterans could receive a score of 0 to 3 on this variable.
To examine use of high-cost acute services, we constructed three variables representing the aggregate number (over the six-month postdischarge period) of inpatient hospital days, partial hospital days, and emergency room visits.
Satisfaction and processes of care also functioned as dependent variables. Satisfaction with outpatient care in the three months after discharge was assessed in the participant interviews with a 4-point scale (scored as 0, not all satisfied; 1, not very satisfied; 2, somewhat satisfied; and 3, very satisfied). Participants were asked whether they had received any assistance with an array of different care needs. The five needs categories included coordination of services or engagement; help with substance abuse treatment; medication management; family and social networks and community linkages; and life skills training, support, and practical needs assistance.
Psychiatric symptoms were dependent variables and were assessed with the Brief Psychiatric Rating Scale (BPRS) (
18 ). We utilized the total score as well as the scores on the subscales that measured positive symptoms, negative symptoms, hostility, anxiety, and withdrawal.
The 33-item Quality of Life Interview (QOLI) (
19 ) provided ratings of dependent variables of subjective and objective quality of life in eight life domains: living situation, daily activities and functioning, family relations, social relations, finances, work and school, legal and safety issues, and health. The subjective scale is scored so that 1 (terrible) indicates the worst and 7 (delighted) indicates the best.
Data analysis
We compared the demographic and clinical characteristics of the B-CTI and comparison groups using t tests, chi square analyses, and Fisher's exact tests. We next compared the groups across all sites on the primary service utilization outcomes and on other dependent variables obtained at the three-month assessment. These comparisons were conducted with basic regression models controlling for site as a covariate. Analyses used an intent-to-treat method. Vigorous attempts were made to interview each participant regardless of his or her treatment participation. All available data were used in the data analysis.
Because of potential site differences in the implementation of the B-CTI model and to account more directly for degree of adherence to the model, we conducted post hoc exploratory analyses, repeating all of the above analyses including only individuals in the B-CTI group who received the intervention with high fidelity (participants with fidelity summary index scores >3. We conducted another set of analyses including only those with fidelity summary index scores >4). We made within-site comparisons for the combined sites 1 and 2 and site 4 using the same analysis plan outlined above. Site 3 had too few participants for site-level analyses.
Comparisons of counts of inpatient, outpatient, and emergency room visits were conducted with negative binomial regression models, the resulting effect estimates from which are expressed as event rate ratios. Poisson regression models are often used to analyze counts; however, the count distributions for this study were overdispersed, and we therefore utilized negative binomial regression.
To accommodate count distributions with a high proportion of zeros, we used zero-inflated negative binomial regression (
20 ). Such models posit two latent groups: one whose response is almost always zero (for example, those not in need of a psychiatric inpatient stay) and the other with a distribution that can include some zeros (for example, those who are in need of a psychiatric inpatient stay but who do not go). A pair of effect estimates is produced by these models: one, the relative odds of not having an event (for example, inpatient visit), and two, the event rate ratio (among those in the second latent group).
Comparison of continuous measures, scores, and Likert scales was conducted with linear regression. Comparison of dichotomous variables (percentages) was conducted with logistic regression. The one event-time variable (time until earliest service) was analyzed with a Cox proportional hazards regression model to account for right-censoring.
Results
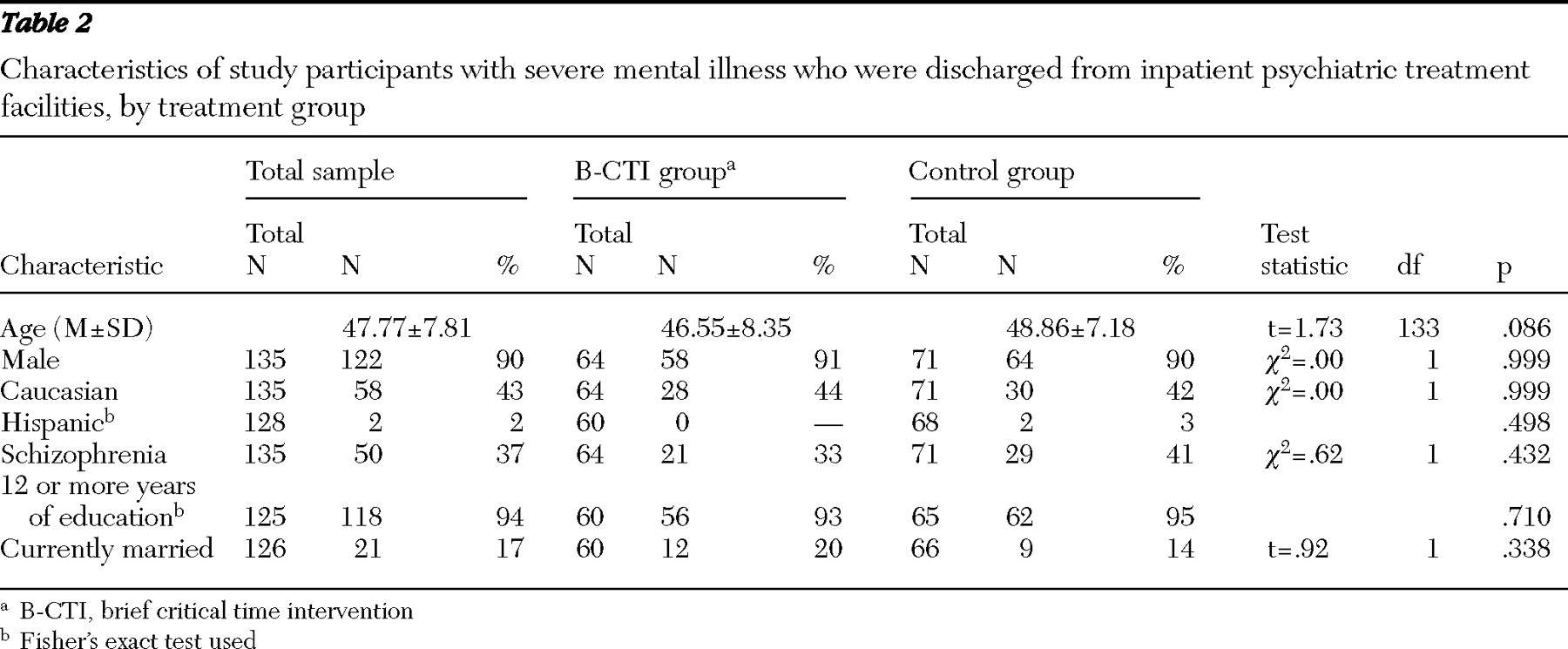
Demographic characteristics of the sample and the intervention groups are shown in
Table 2 . Most participants were male, and there was a mean age of 47.8 years. There were no significant differences between the two intervention groups with regard to demographic variables.
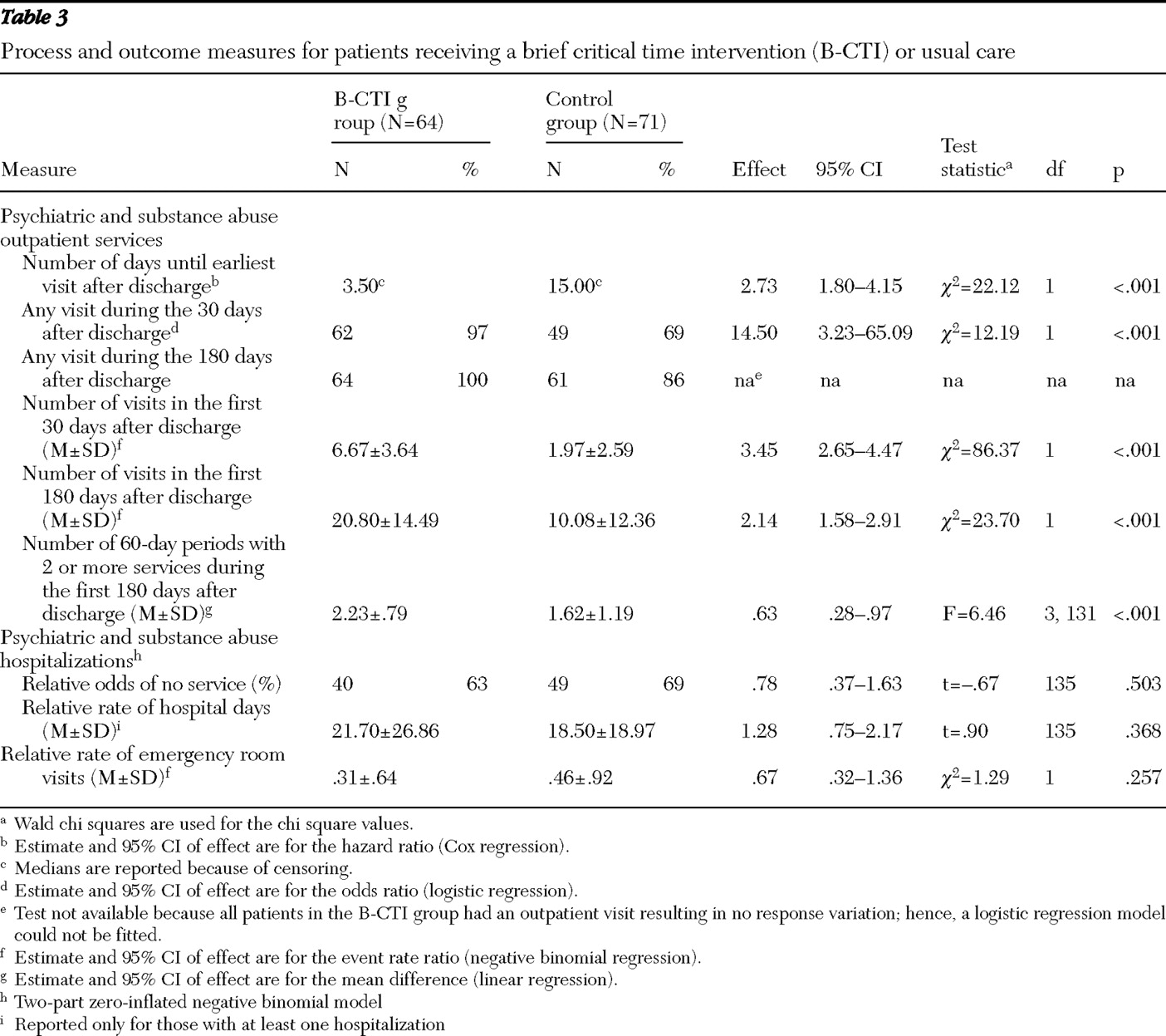
Continuity and intensity of care
Compared with the control group, the B-CTI group had significantly fewer days between hospital discharge and the first outpatient visit (
Table 3 ). A greater proportion of participants in the B-CTI group had a mental health or substance abuse visit within 30 days and 180 days of discharge. Participants in the B-CTI group had more total mental health and substance abuse visits within 30 days and 180 days of discharge. Those in the B-CTI group also had greater continuity of outpatient care, as evidenced by a greater number of two-month blocks with two or more outpatient visits over 180 days.
Acute and subacute care
There were no overall differences between the groups in days of hospitalization or emergency room visits (
Table 3 ).
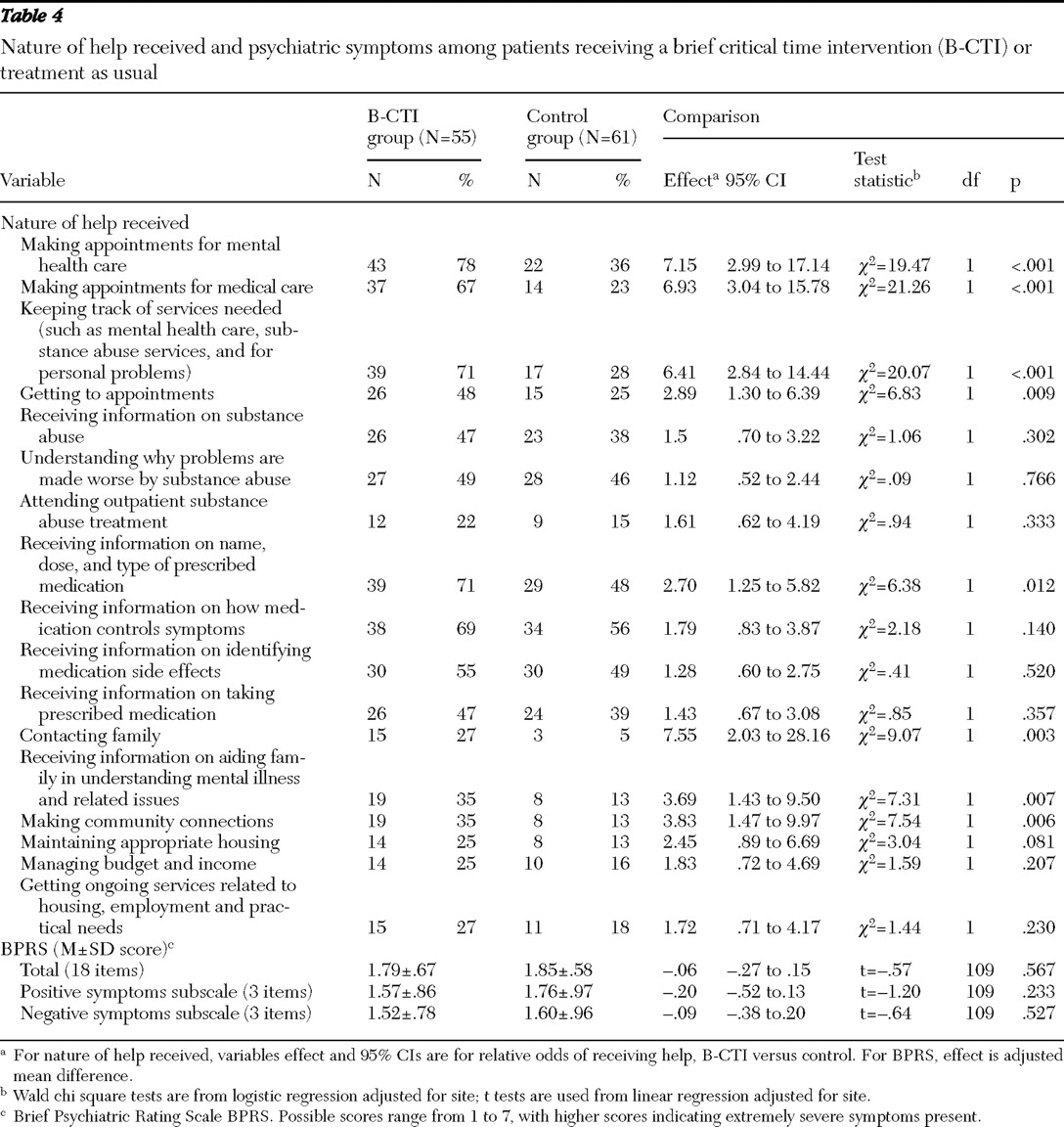
Satisfaction and needs
Overall satisfaction with mental health services did not differ between the groups. Participants in the B-CTI group reported receiving significantly more help in scheduling mental health and medical outpatient appointments and in tracking and getting to those appointments. Those in the B-CTI group reported receiving more information on name, dose, and type of medication prescribed for them and receiving more aid in contacting family members and social supports, making community connections, and helping family members to better understand mental illness and other related issues (
Table 4 ). The two groups did not differ in receiving general information on substance abuse, understanding why problems are made worse by substance abuse, attending substance abuse treatment, receiving information on how medication controls symptoms and side effects, and receiving help with practical housing and budget needs.
Quality of life and symptoms
Compared with participants in the control group, those in the B-CTI group described significantly greater levels of satisfaction with legal and safety issues (5.30±1.5 versus 4.72±1.5; p=.026) and greater frequency of social contacts (2.92 ±1.15 versus 2.40 ±1.08; p=.013). No differences were found in satisfaction with living situation, daily activities and functioning, family relations, finances, work and school, and health. Psychiatric symptoms did not differ between the groups.
Fidelity analyses
Sensitivity analysis that examined only participants in the B-CTI condition who received the intervention with high fidelity did not change any results. Eighty percent (51 of 64) received a fidelity score rating of 3, and 63% (40 of 64) received a fidelity rating score of 4.
Site analyses
The B-CTI group at sites 1 and 2 had significantly fewer psychiatric emergency room visits, compared with the control group (.2±.5 versus .6±1.0) ( χ 2 =4.14, df=1, p=.042).
Discussion
This study provides evidence that B-CTI targeted at the point of inpatient discharge can be helpful in promoting postdischarge continuity of care. This is consistent with previous studies of CTI, which have shown its effectiveness in reducing homelessness among persons with serious mental illness who are living in shelters and in reducing homelessness and institutionalization for homeless veterans who are being discharged from inpatient settings (
13,
21 ). Of note, our program was not intended for individuals with a level of care targeting needs consistent with referral to assertive community treatment or the VA's Mental Health Intensive Case Management. It was purposely designed for and implemented within a group of patients who were thought to benefit from this low-intensity supplemental service. In general, the more targeted and focused the psychosocial interventions are, the more they are found to be effective for their targeted outcomes.
Although B-CTI did not produce overall reductions in use of high-cost acute services, combined sites 1 and 2 had an overall reduction in use of emergency room services. Although caution is important in interpreting this secondary analysis, these sites may have had different patterns of use of emergency room services that were more amenable to modification by B-CTI. A recent study of Medicaid beneficiaries investigated the likelihood of outpatient follow-up within seven days of discharge from inpatient services. Study hospitals had widely different rates of follow-up, suggesting that provider and facility characteristics may play a key role in outpatient follow-up (
22 ).
The B-CTI participants received services in the target areas identified during their ongoing assessment. This suggests that B-CTI clinicians were in fact focusing on connecting patients to outpatient services and solidifying community supports. The B-CTI clinicians clearly did not focus on substantive aspects of treatment, such as medication and substance abuse, which may be more appropriate for longer-term services.
B-CTI produced only a modest impact on overall outcome, with no differences in symptoms, compared with the control intervention. Quality of life improved in one subjective domain (satisfaction with legal and safety issues) and one objective domain (overall social contacts). This could be interpreted as a discouraging comment on the absence of association between processes of care and outcomes and limited cost-effectiveness. However, psychiatric symptom levels were low overall, and it is possible that both a ceiling effect and the maximum degree of medication adherence at the time of discharge hindered the expression of symptom differences at the three-month assessment. The quality-of-life differences between the groups may again reflect the B-CTI focus on social networks, which may also enhance a feeling of safety. Notably, the follow-up period of three months was short; future work should focus on whether B-CTI's short-term improvement in care processes improves outcomes over a more extended period.
Our study was limited by its small size and geographic scope and limited power to explore the impact of fidelity and site-level implementation differences. These limitations are balanced by the randomized experimental design, careful implementation of a manualized intervention by trained but regular clinical staff, and raters blind to study condition.