Latinos, the largest and fastest-growing ethnic minority group in the United States, are less likely than whites to receive depression treatment (
1,
2 ). Low rates of care can be attributed in part to practical barriers, such as low rates of health insurance and regular source of care (
3 ). However, findings that insured Latino primary care patients had lower rates of depression care than insured white primary care patients (
4 ) and that low-income patients and those with less treatment knowledge were more likely to decline care for depression (
5 ) suggest that depression-related attitudes and preferences that have not been well understood or addressed may contribute to disparities in care. The Institute of Medicine suggests that addressing patient treatment preferences is essential in improving quality of care (
6 ).
Previous studies suggest that for the treatment of depression many Latinos prefer counseling or combined counseling and medication over medication alone (
5,
7,
8,
9,
10 ). One collaborative care intervention was shown to improve the likelihood that insured primary care patients received preferred depression treatment, but it was more challenging to accommodate a preference for counseling than for medication (
11 ). It is unknown whether collaborative care could similarly improve access to preferred treatment in safety-net primary care settings serving low-income, uninsured Latinos, who may be more likely to prefer counseling.
Among 339 low-income Latino primary care patients in three public-sector primary care centers in Los Angeles, we assessed depression treatment preferences using conjoint analysis, a market research survey method adapted for measuring health care preferences (
7,
12,
13,
14 ). Next, we conducted a randomized controlled trial of a collaborative care depression intervention that provided patient education and allowed patients to choose between medication, counseling, or combined treatment. We examined whether patients randomly assigned to the intervention group were more likely than those randomly assigned to the enhanced usual care group to report that they received preferred treatment. We also examined which patient characteristics were associated with receiving preferred treatment.
Methods
Study procedures
This study was approved by the Human Subjects Committees of the University of Southern California, the University of Washington, and the University of California, Los Angeles. From November 2005 to July 2007, patients were recruited for the study at three primary care clinics in Los Angeles that serve predominantly low-income Latino populations. Patients seated in clinic waiting rooms were approached using a systematic sampling scheme and asked to participate; additional patients were referred to the study by providers. If patients were aged 18 years or older, spoke English or Spanish, and provided oral informed consent to participate, they were given an English or Spanish screening interview to complete.
The screening interview assessed eligibility to participate in the study. Patients in the clinics were eligible if they had probable major depressive disorder or dysthymia, which was determined by using the PRIME-MD Patient Health Questionnaire-9 (PHQ-9) (
15,
16,
17 ) and two questions from the Primary Care Evaluation of Mental Disorders (PRIME-MD) (
15 ). Patients were excluded if they had probable bipolar disorder (assessed with the Mood Disorder Questionnaire [
18 ]), cognitive impairment (assessed with a six-item screener derived from the Mini-Mental State Examination [
19 ]), lifetime psychotic symptoms or disorder (assessed with three stem items from the Composite International Diagnostic Interview Version 2.1 psychotic disorders module [
20 ] and one question from the Improving Mood: Promoting Access to Collaborative Treatment (IMPACT) study regarding a lifetime history of schizophrenia or schizoaffective disorder [
21 ]), or suicidal ideation.
Eligible patients who agreed to participate in the study provided written informed consent and completed baseline surveys (96% in person and 4% by telephone) in English or Spanish and were then randomly assigned to receive the 16-week collaborative care intervention or 16 weeks of enhanced usual care followed by the intervention. Randomization was stratified by clinic site, referral source, and gender. In the collaborative care intervention (
22 ), a bilingual master's-level social worker functioned as a depression care specialist and educated patients about depression and its treatment, elicited treatment preferences, and provided active outreach and systematic assessment.
Depending on patients' treatment preferences, the depression care specialist provided short-term manualized cognitive-behavioral therapy, supported antidepressant medication treatment, or both. Supported antidepressant medication treatment involved encouraging adherence, assessing side effects and treatment response, and sharing this information with primary care providers. Cognitive-behavioral therapy was provided at no cost, and prescriptions were filled at low or no cost (according to patients' usual payment arrangements at each clinic). In enhanced usual care, patients received a letter that they could bring to their primary care provider stating that they had screened positive for depression, an educational pamphlet, and a list of local mental health resources. Patients completed English or Spanish follow-up surveys 16 weeks after baseline assessment (86% in person, 11% by telephone, and 3% both in person and by telephone).
Measures
Conjoint analysis survey. Conjoint analysis assumes that consumers make choices among products on the basis of product characteristics (attributes) (
23 ). For example, consumers shopping for an automobile might simultaneously consider size, color, price, engine power, and fuel efficiency and trade off among these attributes to make a choice. In a conjoint analysis survey, participants choose among hypothetical products with varying combinations of attributes.
To design this conjoint analysis survey, attributes of depression interventions and strategies to reduce treatment barriers were identified from the literature (
24,
25 ), clinical guidelines (
26 ), focus groups, and a pilot study (
7 ). Then for each attribute, "levels" (or options) were determined. For depression treatment interventions, levels were determined for attributes as follows: treatment type (counseling, antidepressants, or both), treatment format (individual or group), treatment location (primary care or mental health clinic), and cost (no cost, $10 per month, or $20 per month). For barrier reduction strategies, levels were assigned for reducing transportation barriers (bus passes, treatment sessions by telephone, or no assistance), family involvement (yes or no), educational interventions (individual education session, group education session, or a combination of pamphlets and videos), and cost (no cost, $10 per month, or $20 per month).
Attribute levels were combined to create hypothetical treatments or barrier reduction strategies (for example, individual counseling at the primary care clinic for $20 per month or a medication group at a mental health clinic at no cost). The survey was administered at baseline in English or Spanish with visual depictions of combinations. [Examples of conjoint analysis survey cards used in the survey are available as an online supplement at
ps.psychiatryonline.org .] Each survey included six pairwise comparisons for each of the treatment scenarios and barrier reduction scenarios. Pairwise comparisons were determined by using a fractional factorial design. For each pair of scenarios, patients selected the one they preferred. Brief standardized descriptions of all treatment and barrier reduction attributes were read to patients before the survey was administered (script available upon request). For example, counseling was described as weekly meetings with a trained therapist (alone or in a group) to learn new ways to understand one's problems and develop techniques to work through them; new coping skills must be practiced between sessions, and improvement may occur over weeks to months. Medication was described as a treatment provided by a primary care provider or psychiatrist via prescription after appointments that would occur approximately monthly. Patients are also told that medication is not addictive, should be taken daily, may have side effects that can be managed, and may result in improvement after approximately one month.
Treatment received. Sixteen weeks after baseline assessment, English and Spanish self-report items validated in Partners in Care (PIC) (
27 ) were used to assess antidepressant medication use and receipt of counseling. "Any medication treatment" was defined as the use of any prescribed medication for personal, mental, or emotional problems, such as depression, anxiety, or nerves, regularly for one month or more in the previous four months. "Any counseling" was defined as one or more visits to a psychiatrist, psychologist, social worker, or counselor over the previous four months. As a validity check, we compared self-reported treatment among persons in the intervention group to treatment recorded by depression care specialists in treatment logs and found them to be significantly correlated. (Data available upon request).
Other measures. The baseline interview assessed age, gender, race, education, employment status, insurance status, language preference and country of origin, and possible presence of comorbid anxiety disorder symptoms (based on the PRIME-MD [
16 ]). Items from PIC (
24 ) assessed past treatment experience, knowledge about depression and its treatment, number of comorbid medical illnesses, stigma regarding depression care, and perceived barriers to care. Clinic site, referral source, and recruitment day and time were recorded.
Analysis
Analysis was limited to Latino participants, because our primary aim was to describe treatment preferences of Latinos and because the small sample of non-Latino patients limited our ability to draw conclusions about their preferences. We used univariate and bivariate analyses to describe the sample. A random utility model was used to create binary logit estimates of treatment and barrier reduction preference parameters (
23 ). For each regression model, the dependent variable was a binary indicator of patient's willingness to accept or not accept treatment, and independent variables were the attribute levels. The estimated
β coefficients indicate the relative utility of each attribute level, with positive values indicating stronger preference. The exp(
β ) represents the odds that a particular attribute level will increase overall treatment acceptance.
To examine patient characteristics associated with treatment preferences, the following baseline covariates that were chosen on the basis of previous literature were included in the logistic regression models (
1,
5,
28,
29 ): referral source, gender, employment status, age, years of education, insurance status, language spoken, stigma, baseline depressive symptom severity, probable anxiety disorder, number of comorbid medical illnesses, past treatment, and knowledge about medication and counseling. Interactions between covariates (such as depressive symptom severity) and attributes (such as treatment type) that would indicate the direction of the association between covariates and attributes were not found to be significant and were dropped from the final model. Mode of survey delivery (telephone versus in person) did not significantly predict treatment preferences and was not included in the final model. Conjoint data were analyzed by using SPSS, version 11.5, multinomial logit regression procedure.
Using conjoint analysis survey results, we defined a preferred treatment type (medication, counseling, or combination) for each participant. Participants whose conjoint survey results did not reflect a clear treatment preference were described as having no preference. Next, we derived a variable denoting match between stated preference (medication, counseling, both, or none) and self-reported treatment received. To examine the intervention effects on the likelihood of a match between stated preference and treatment received, we conducted logistic regression analysis that included intervention status as the primary predictor and included clinic, depressive disorder status, perceived barriers to care, and all of the covariates used in the regression listed above. To account for nonresponse to the 16-week follow-up survey, we used separate logistic regression models for the intervention and usual care groups to identify patient characteristics associated with nonresponse and used results to construct nonresponse weights. We conducted both weighted and unweighted intent-to-treat analyses using survey command in SAS, version 9.1. Weighted and unweighted analyses yielded very similar results. Unweighted results are reported.
Results
Of the 3,317 patients approached in the waiting room who were eligible for screening, 1,951 (59%) refused to participate. Of the 306 patients referred by providers, 24 (8%) refused screening. The most common reason for refusal was "not interested or do not have time" (N=1,642, 83%). Among the 1,637 patients who completed the screening, 626 (38%) screened positive for depressive disorder and 522 met study inclusion criteria. This article focuses on the 339 Latinos who screened positive for depressive disorder, were enrolled in the study, and had complete survey data at baseline. A total of 166 Latinos were randomly assigned to usual care, and 173 Latinos were randomly assigned to the intervention. Among Latinos, 148 (86%) participants in the intervention group and 139 (84%) participants in the usual care group completed the 16-week follow-up interview. [A CONSORT figure showing the number of patients screened, enrolled, and followed up is available as an online supplement at
ps.psychiatryonline.org .]
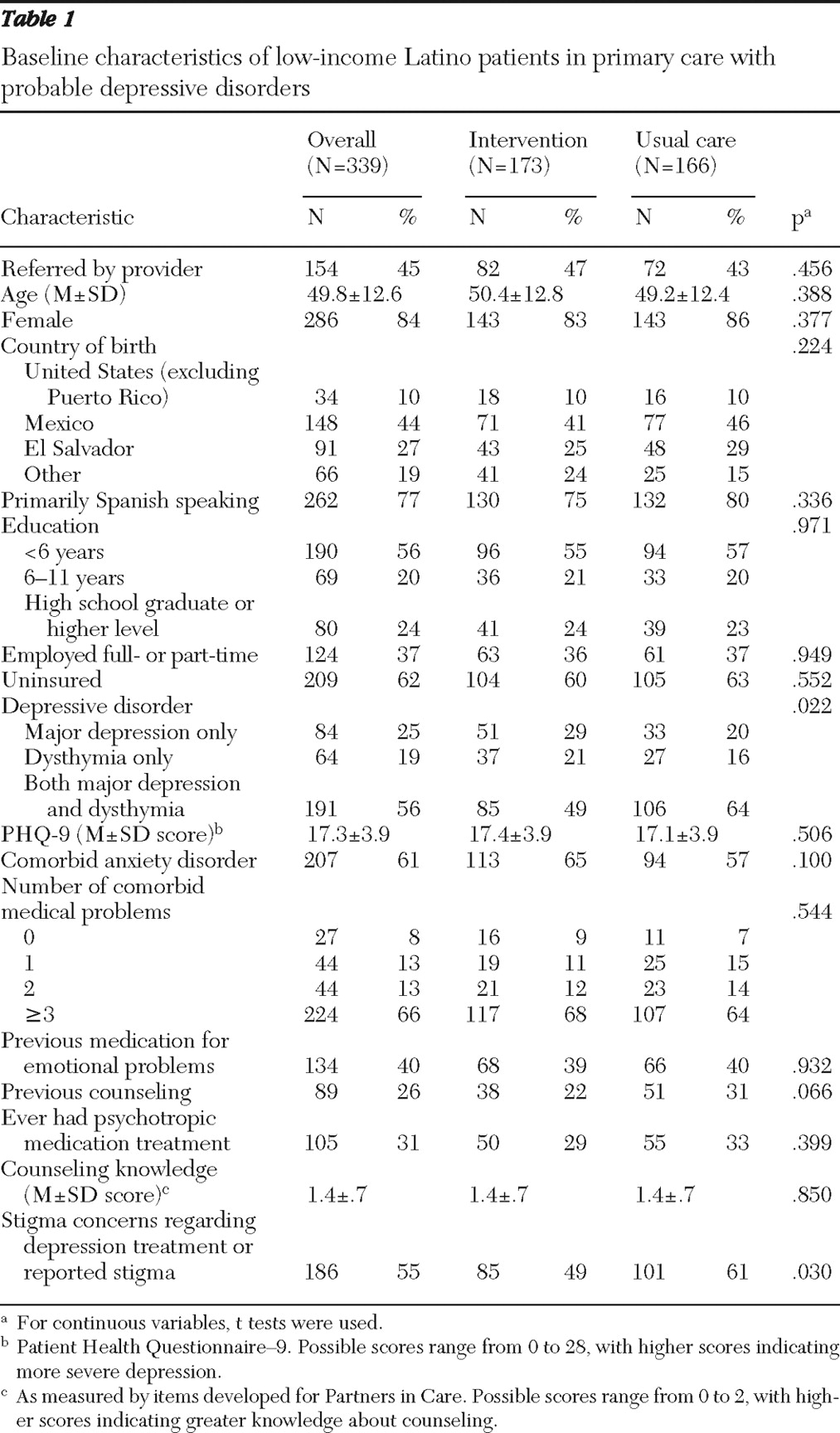
The baseline characteristics of the Latino sample are presented in
Table 1 . The overall mean±SD baseline PHQ-9 score was 17.3±3.9, indicating moderately severe depression (
30 ). The baseline PHQ-9 score was similar across both groups, although usual care participants were significantly more likely to have major depression and dysthymia (versus either alone) and were significantly more likely to report stigma regarding depression.
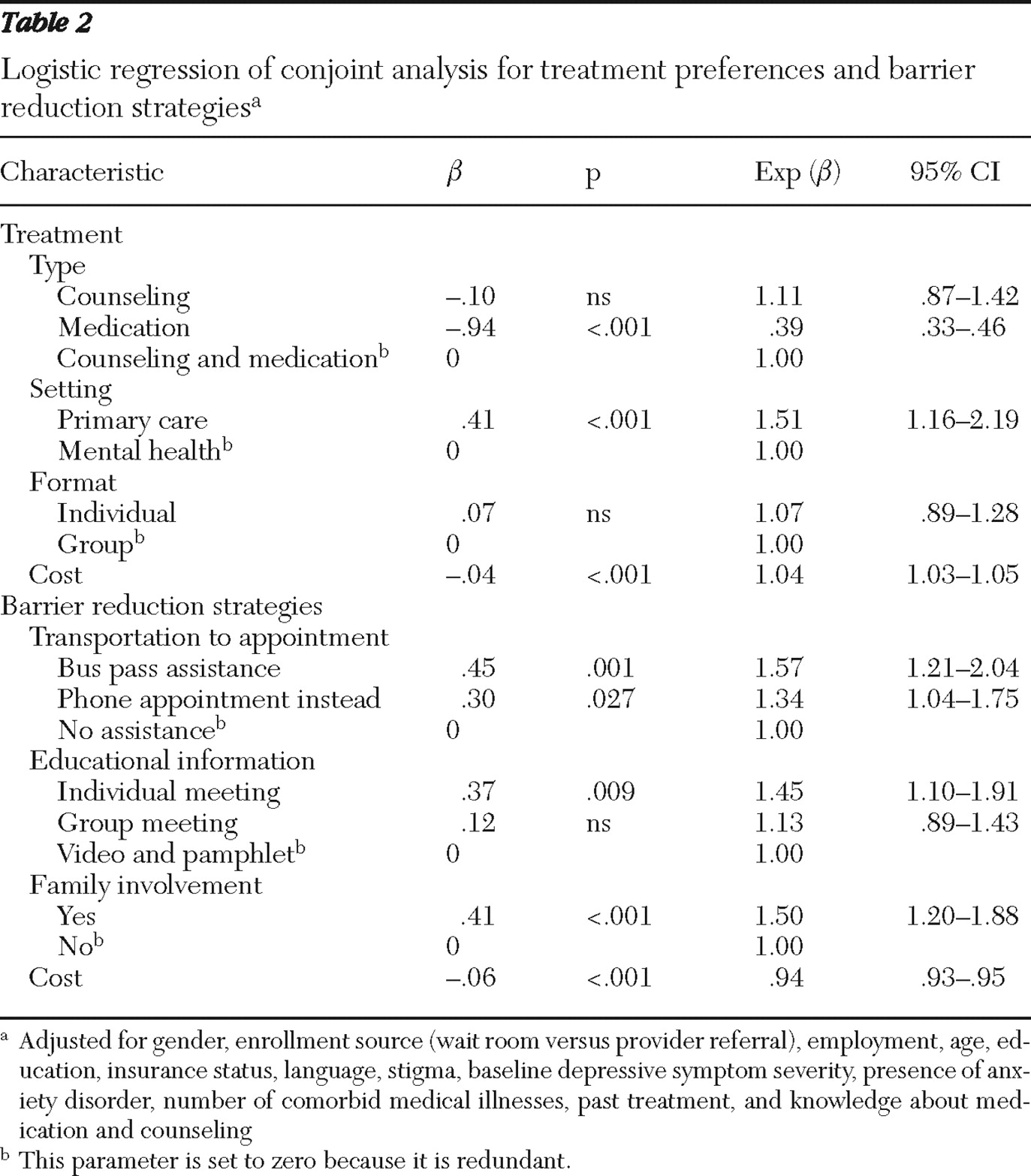
Table 2 presents the results of the conjoint analysis survey. Participants indicated that they preferred counseling or counseling plus medication over antidepressant medication alone or that they preferred treatment in primary care over specialty mental health care, but they showed no significant preference for individual versus group treatment. Depressive symptom severity and knowledge about counseling were the only patient characteristics significantly associated with treatment choice.
Regarding barrier reduction strategies, patients preferred individual educational sessions over group sessions or video or written materials. The odds of treatment acceptance were increased 1.3 times by availability of telephone sessions, 1.6 times by the availability of bus passes, and 1.5 times if family were involved in care versus not involved. Previous counseling was the only patient characteristic that predicted preference of barrier reduction strategies. The greater the cost of a treatment or barrier reduction strategy, the less likely patients were to prefer that option.
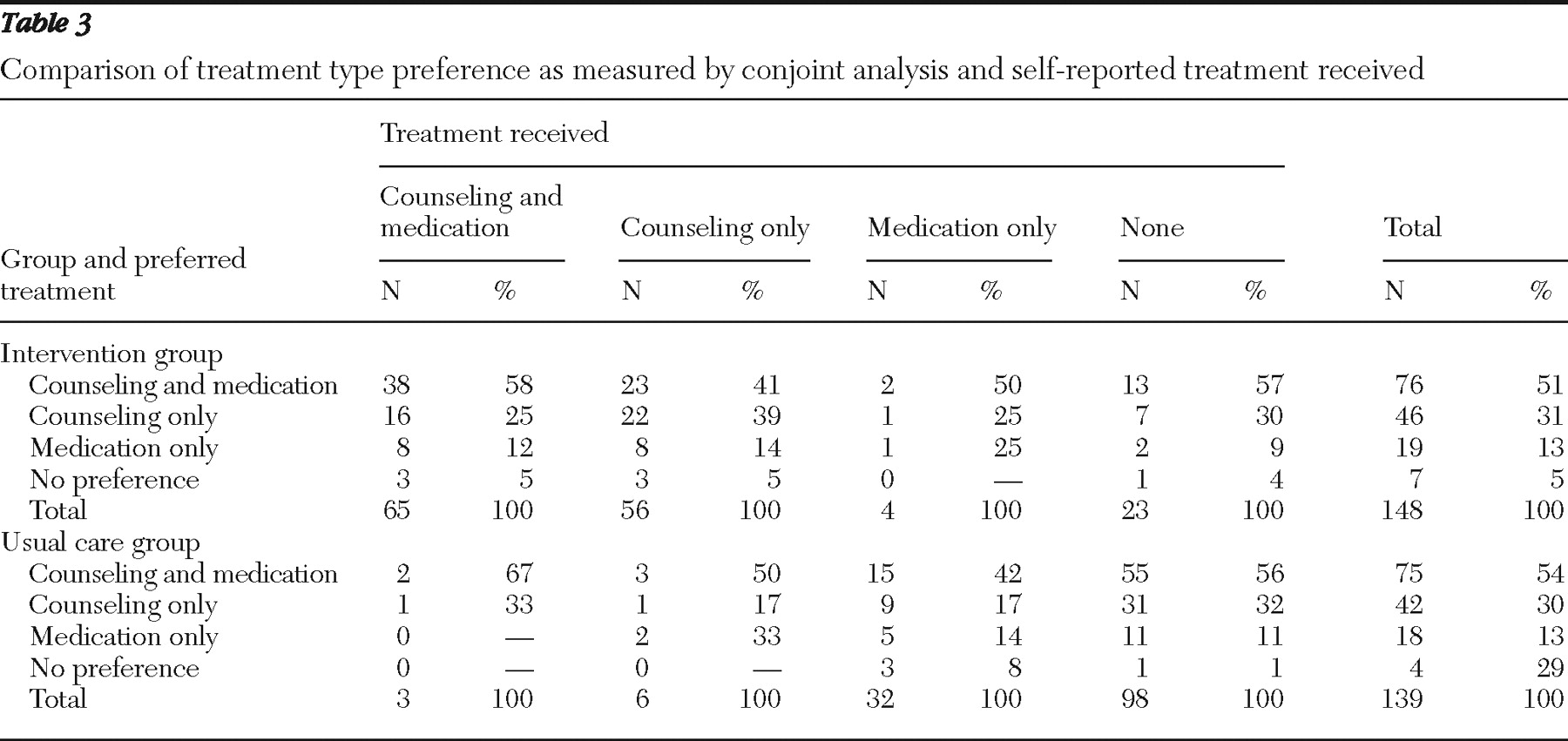
Table 3 shows stated conjoint preferences for treatment type and treatment received. A majority of patients in the intervention group reported receipt of counseling or combined counseling and medication, whereas a majority of patients in the usual care group reported receipt of medication alone or no treatment. In our logistic regression model predicting likelihood of receiving preferred treatment, compared with patients in the usual care group, patients in the intervention group had 21 times greater odds (odds ratio [OR]=20.7, 95% confidence interval [CI]=8.0–53.9, p<.001) of receiving preferred care. Among all participants, women (OR=3.9, CI=1.4–11.2, p=.011), patients referred by providers (OR=2.7, CI=1.3–5.6, p=.007), unemployed persons (OR=3.0, CI=1.4–6.4, p=.004), and English-speaking patients (OR=2.6, CI=1.2–5.7, p=.02) were also more likely than their respective comparison groups to receive preferred treatment.
Discussion
Low-income Latino primary care patients in this sample were more likely to prefer counseling or combined counseling and medication than medication alone for the treatment of depression. Patients preferred to remain in primary care for depression treatment over referral to specialty mental health, consistent with epidemiologic studies showing that a majority of Latinos receive depression treatment in primary care (
1 ). Patients also indicated that individual education sessions, telephone sessions, transportation assistance, and family involvement were barrier reduction strategies that would enhance their likelihood of accepting treatment.
Depression symptom severity and knowledge about counseling were associated with choice of treatment type, and previous experience with counseling also appeared to inform patient preferences for strategies to encourage entry and retention in care. However, we were unable to describe the association between these patient characteristics and specific treatment type or barrier reduction attributes, because interaction terms were not significant in our model, possibly because of limitations in sample size.
Patients receiving enhanced usual care were unlikely to receive counseling, the treatment preferred by most. Our collaborative care intervention, which promoted patient activation, included active outreach, accommodated patient preference, and provided on-site counseling, greatly increased the odds that patients received preferred treatment. However, even in the intervention group, stated preference did not match treatment received for all patients.
Mismatch between stated preference and treatment received may have several different causes. Because Spanish speakers were less likely than English speakers to receive preferred treatment, language or cultural barriers may have impeded patients from communicating or advocating for preferred treatment. Such barriers to obtaining preferred care may contribute to the observation that Latino immigrants with mental disorders and those with limited English proficiency have even lower rates of care compared with other Latinos (
1,
31 ). Participants referred by their providers may have been more able to communicate distress to providers than those recruited via waiting room screening, and primary care providers may have supported or advocated for patients to receive preferred treatment. Employed persons may have been less likely to receive preferred treatment because most were employed in low-wage jobs with little flexibility or sick leave, a salient barrier for those preferring counseling. Although treatment preferences of men and women were not significantly different, men were less likely than women to receive preferred treatment. This finding, along with observed low rates of depression care among men (
1 ), suggests the need for tailored outreach efforts to engage men in depression care.
An alternate explanation for mismatch between stated preference and treatment received may be a shift in preference over time, as a result of treatment exposure or influence of the depression care specialist's educational efforts or treatment recommendations. In future analyses, including qualitative studies, we will examine in detail the question of a shift in treatment preference over time and with treatment exposure.
Limitations of our study should be considered when interpreting our results. Our sample may not reflect preferences of Latino patients who are not in primary care, those with more education, those of different socioeconomic backgrounds, or those not of Mexican or Central American heritage. Although conjoint analysis has been shown to predict consumer behavior, has been used in low-income and Latino immigrant populations (
32,
33,
34 ), and is considered to be more accurate than standard survey methods (
35,
36 ), its ability to accurately assess treatment preferences among those with less treatment experience and knowledge may be limited. Although education about attributes is standard practice in conjoint analysis surveys, the content of the script may bias participants' responses or may not provide in-depth explanation of the treatment choices. Choices in the survey were matched to choices available in the intervention arm of the study (for example, treatment choices were limited to counseling, antidepressant medication, or both); thus results may not reflect preferences for other types of therapies and treatments or the option of no treatment.
Previous studies suggest that low-income patients and those with less knowledge about treatment are more likely to prefer watchful waiting to active treatment (
5 ), a preference that may influence entry into care. Baseline differences between the intervention and control groups in depressive disorder status and stigma may have contributed to differences in receipt of preferred care between the two groups that may not have been fully accounted for by controlling for disorder status, depressive symptom severity, and stigma in regression models.
Conclusions
Despite study limitations, our findings confirm that distress, treatment knowledge, and experience can influence patient treatment preferences among low-income Latino primary care patients. Our findings underscore the importance of including psychotherapy as a treatment option for Latinos in primary care and also suggest that a collaborative care intervention that accommodates patient choice and provides on-site psychotherapy in primary care can improve access to preferred care.
Sustaining collaborative care models than include psychotherapy would require public and private payers to reimburse for such services in primary care settings. Improving access to psychotherapy for Latino primary care patients will also require training culturally diverse, bilingual providers in psychotherapies shown to be effective for depression among persons from ethnic minority groups (
37 ). Some groups, including men, Spanish speakers, and employed persons, may require additional outreach, advocacy, and flexibility in order to meet their preferences. A recent pilot study suggests that telephone delivery of psychotherapy is effective for Latino primary care patients and may improve access to preferred treatment, especially among low-income employed persons and those with stigma concerns (
38 ). Although psychoeducation about depression and its treatment can be effectively delivered by trained nurses and social workers in primary care settings (
27,
39 ), more research is needed to develop culturally tailored psychoeducation approaches that can assist depressed Latinos in making informed treatment choices.