Parenting a child with a serious mental illness, such as schizophrenia or bipolar disorder, presents major lifelong challenges. To be sure, parents may provide decades of extended caregiving, especially during times when their adult child's debilitating psychiatric symptoms produce ongoing obstacles to social and occupational functioning and independent living (
1,
2 ). As parents age, they confront the dual stressors of having to cope with the challenges of having an adult child with serious mental illness while dealing with their own aging-related changes in health, such as physical disability and greater vulnerability to illness (
3,
4,
5 ). In addition, older age is a stage in the life course when parents become increasingly concerned about the future care of their son or daughter with mental illness (
6 ).
Prior studies have largely focused on the substantial toll of caregiving (
7,
8,
9 ). This body of research suggests that older parents of adults with serious mental illness experience, on average, high levels of burden and elevated general medical symptoms and psychiatric symptoms (
10,
11 ). The impact of caring for an adult child with serious mental illness is often framed in terms of subjective burden, which is conceptualized as the range of negative emotional reactions to caregiving (
12,
13 ).
Past research has concentrated mainly on the negative impact of parenting an adult child with serious mental illness in later life; a more balanced perspective is one that recognizes the potential for personal growth associated with the caregiving role. Indeed, although later stages of the life course may involve unprecedented difficulties for parents of adults with serious mental illness, later life may also present unique opportunities for positive parenting experiences, including personal growth and a greater awareness of family strengths (
14,
15,
16 ).
In contrast to burden, personal gains associated with caregiving correspond to the degree to which family members experience positive transformations as a result of coping with their relative's mental illness (
17 ). For instance, caring for a child with mental illness has led some parents to experience a deepening sense of self-awareness and inner strength (
16 ). Parental caregivers have reported becoming stronger, more tolerant, less judgmental, and more sensitive and empathetic toward others over time (
18 ). In addition to targeting caregiver distress, interventions have aimed to enhance caregiving experiences (
19 ). Understanding the family's experience of personal gains and the role of the adult with mental illness in contributing to these gains has taken on a new significance in light of efforts to transform the mental health system of care on the basis of recovery principles.
A number of studies have focused on the relationship between the stressors of caregiving and parental well-being (
20,
21 ). One of the major challenges for parents of adults with serious mental illness is providing ongoing support with activities of daily living, often referred to as objective caregiving burden. The research is inconclusive on the relationship between subjective burden and the objective burden associated with providing hands-on care and supervision. Whereas some researchers report that when persons with mental illness have a greater need for help with activities of daily living, their caregivers report higher levels of subjective burden (
22 ), others report only a weak relationship between the amount of assistance or supervision needed by the family member with mental illness and the caregiver's experience of subjective burden (
23,
24,
25 ). Living with an adult child with serious mental illness may be especially challenging for older parents. In a longitudinal study of the end of in-household caregiving among aging mothers of adults with serious mental illness, Seltzer and colleagues (
9 ) found that stress in the caregiving context predicted the end of living together and that mothers reported significantly lower levels of subjective burden after the adult child's move out of the house.
Whereas subjective burden tends to be most associated with the demands of caregiving, personal gains appear to be associated with parental resources, in particular parents' level of social support. Indeed, research has begun to raise awareness of supportive resources that promote positive family experiences in serious mental illness (
15,
16,
17 ). Family members of persons with serious mental illness have demonstrated a pattern of coping in which they first turn to other family members and close friends for support and then seek help from others with similar experiences (
26 ). In addition to the benefits derived from confiding in a family member or close friend, seeking support from others who are facing similar challenges can foster mutually supportive environments that promote mastery and growth. Indeed, support group participation is positively associated with caregiving gains among families that care for a member with mental illness (
17 ). Furthermore, adults with serious mental illness can themselves be a source of support to aging parents. Greenberg (
27 ) found that when adults with schizophrenia were able to reciprocate through the provision of instrumental and expressive support, parents experienced less subjective burden.
In this study, we first examined the factors associated with personal gains among older parents of adults with serious mental illness. We then examined the factors associated with subjective burden, using the same sample of parents to examine both outcomes. Because literature suggests that personal gains are associated with parental resources (specifically, level of social support) and that burden tends to be associated with stressors in the caregiving context, we hypothesized that parental stressors (such as child's poorer health, greater parental care provided, and parent and child living in the same household) would be most strongly associated with parental feelings of subjective burden, whereas parental resources (such as the child's assistance to the parent, availability of confidants, and support group membership) would be most strongly related to personal gains after we controlled for background characteristics (including parent's age, gender, and education and child's gender).
Methods
This study involved secondary analysis of data drawn from the Wisconsin Longitudinal Study (WLS), which is a random sample of over 10,317 Wisconsin high school graduates and their randomly selected siblings, who have been followed for approximately 50 years (
28,
29 ). The WLS sample was recruited before they became parents and thus was independent of their child's psychiatric diagnosis. This study therefore does not suffer from the potential selection biases that arise in studies that recruit participants after their child has developed a mental illness.
The WLS includes four waves of data collection from the original respondents, in 1957, 1975, 1993, and 2003–2005, and from subsequent interviews with their randomly selected siblings in 1977, 1994, and 2005–2007. In 1957 respondents average age was 18, and at the subsequent points of data collection their average ages were 36, 52–53, and 64–65, respectively. We chose to focus this analysis on the fourth wave of WLS data collection, when most respondents were in their mid-60s, because a major aim of our study was to examine subjective burden and personal gains among older parents of adults with serious mental illness. At this fourth wave, respondents completed a one-hour telephone survey and a self-administered questionnaire. Informed consent was obtained for all study participants. The institutional review board of the University of Wisconsin-Madison approved all the procedures for the protection of human subjects.
Participants
Using a series of screening procedures in the telephone interview, we identified 196 original and sibling respondents who were parents of an adult with serious mental illness (specifically, bipolar disorder or schizophrenia) with whom they had telephone or face-to-face contact during the year before the interview. We excluded 34 parents because they did not return the extended mailed questionnaire for parents of adult children with disabilities from which the dependent variables in the study were drawn. An additional 51 parents were excluded because they had missing data on key study variables. Thus this study is based on 111 parents of adults with serious mental illness. These 111 parents were compared with the 85 parents who were lost to attrition because of missing items in the telephone survey or the mailed questionnaire. There were no differences between the two groups with respect to parental age, gender, marital status, or household income and the child's age. However, participants were more likely than nonparticipants to have adult sons with serious mental illness versus daughters ( χ 2 =5.64, df=1, p<.05).
Measurement
We examined two dependent variables: subjective burden and personal gains. Personal gains was assessed by a scale adapted from Pearlin (
30 ) and used in a previous study of family caregiving in mental illness (
17 ). The scale comprises ten items that assess the degree to which respondents experienced positive change as a result of coping with their child's mental illness (for example, "How much have you gotten a better idea of what is important in life?" and "How much have you become aware of your inner strengths?"). Respondents indicated their response to each item on a 4-point Likert scale (from 0, not at all, to 3, a lot). Individual items were summed to obtain a personal gains score, with higher scores indicating more personal gains (Cronbach's
α =.95).
Subjective burden was measured by Zarit and colleagues' Burden Interview (
31 ), a measure derived from studies on the impact on families caring for adults with mental disorders living in the community (
32,
33 ) and used in numerous studies to assess the caregiver's perception about or appraisal of the burdens associated with the caregiving role (including time demands, financial strains, lack of privacy, and adverse health consequences) (
9,
10,
34 ). Each of the 29 items is answered with use of a 3-point Likert scale ranging from 0, not at all true, to 2, extremely true. Individual items were summed to derive a total score, with higher scores indicating greater burden (Cronbach's
α =.87).
Parental stressors. This study measured three potential stressors associated with characteristics of the adult child with serious mental illness. First, parents rated their child's overall health on a 5-point scale ranging from 1, very poor, to 5, excellent. Second, parents reported on a 4-point Likert scale (from 0, none, to 3, a lot) the extent to which their child needed help in eight activities of daily living (such as preparing meals, transportation, money management, and help with taking medications). For those tasks for which the adult child needed help, a follow-up question asked whether the parent helped with the task. The amount of parental help provided was a count of the number of daily living tasks with which the parent reported providing assistance. Because few parents helped with more than three activities of daily living, each respondent was categorized as providing no help with tasks of daily living, scored 0; helping with one task of daily living, scored 1; helping with two tasks, 2; or helping with three or more tasks, 3. Finally, parent-child living arrangement was measured by a single item indicating whether the adult lived with his or her parent (0, living apart; 1, living in the same household).
Resources. Three measures of social support were included as indicators of parental resources. The child's contributions to the parent's life was adapted from the patient contribution module of the Family Burden Interview Schedule (35). Using a 4-point Likert scale (0, not at all, to 3, a lot), respondents indicated how much assistance their adult child with mental illness provided to them during the past 30 days in nine areas, such as preparing meals, helping with household chores, listening to the parent's problems and providing advice, and providing companionship. Items were summed and a mean was computed to derive a total score, with higher scores indicating that the adult child provided a greater degree of help to the aging parent (Cronbach's α =.90). Number of confidants was measured by summing two items in which the respondent indicated whether he or she had a family member, friend, or both for sharing private feelings and concerns (0, no confidants; 1, one confidant; 2, two confidants). A high score of 2 confidants indicated that the respondent had both a family member and a friend with whom he or she could confide. Finally, parents were asked to indicate whether they were members of a support group (1, members; 0, nonmembers).
Four background characteristics were included as control variables: the parent's gender (0, female; 1, male), education (0, some college; 1, college graduate), and age, measured as a continuous variable, and the child's gender (0, female; 1, male).
Analysis
Bivariate correlations were computed with the Pearson product-moment correlation coefficient to examine the intercorrelations between the study independent variables (specifically, background characteristics, parental stressors, and parental resources) and the dependent variables (subjective burden and personal gains). To test our primary hypotheses, we ran two separate multiple regression analyses with subjective burden and personal gains as the dependent variables. Analyses were calculated with SPSS software, version 17. Given the relatively small sample and large number of predictors, preliminary analyses were conducted to reduce the number of independent variables in the model. Because the background characteristics were conceptualized as control variables and were not significantly correlated with the dependent variables, and because dropping them from the model did not substantively change the findings, we excluded them from the final regression models.
Results
Characteristics of parents and adult children
The parents of the adult children with serious mental illness had a mean±SD age of 63.9±3.5, and 62% (N=69) were mothers. With regard to marital status, 69% (N=77) of the parents were married, 19% (N=21) were divorced, and 12% (N=13) were widowed. A majority (N=69, 62%) had at least some college education, and 38% (N=42) earned a college degree. The median income for the parents was $46,248, reflecting the retirement status of most respondents.
The average age of the adults with serious mental illness was 37.7±5.8. Forty-one percent (N=45) were women, and only 23% (N=25) were married at the time of the survey. Most adult children had a primary diagnosis of bipolar disorder (N=76, 69%). They began having mental health problems when they were 18.1±8.8 years old and were diagnosed as having a serious mental illness at age 22.5±8.08. Almost three-quarters (N=80, 72%) of the adults had at least weekly contact with their parents by telephone or in person; most (N=82, 74%) lived in independent settings (such as apartments or houses). The characteristics of this sample are similar to those found in other studies of adults with serious mental illness (
24,
36 ).
Correlations
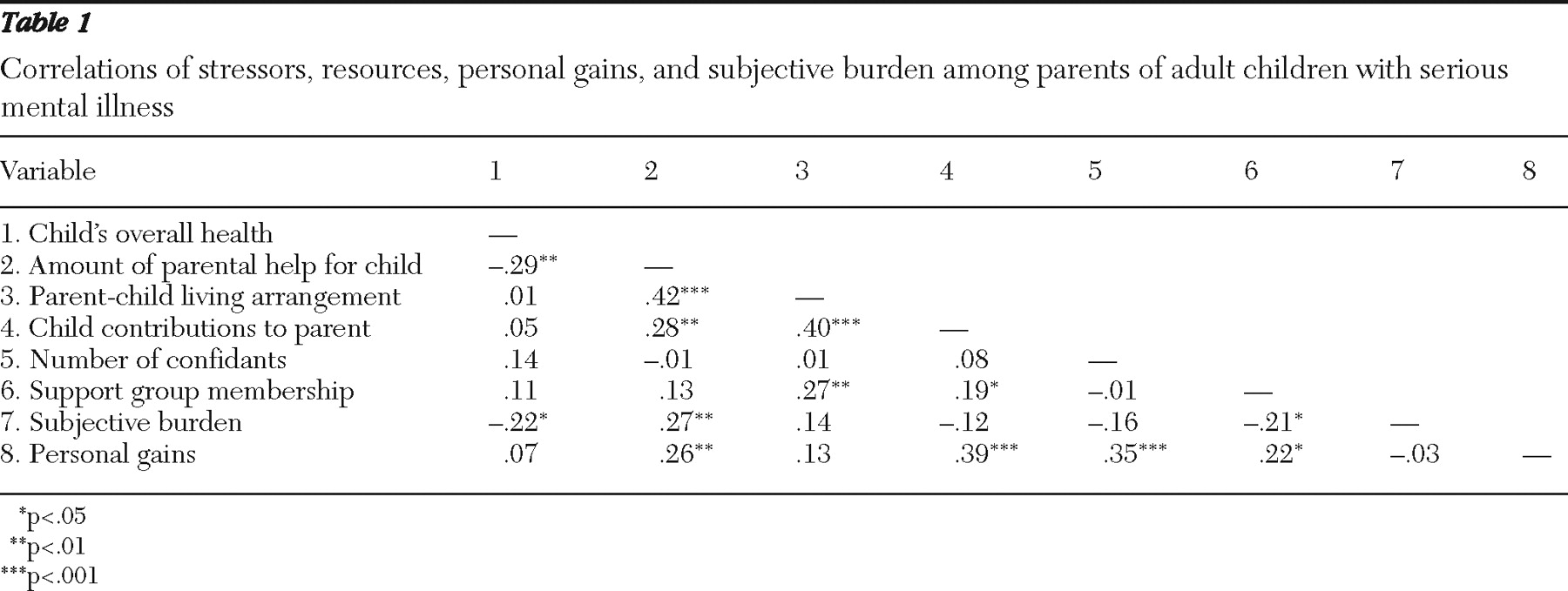
Table 1 reports the correlations between the measures of parental stressors and resources and subjective burden and personal gains. The child's contributions, the parent's number of confidants, and the parent's support group membership were each positively and significantly correlated with personal gains for the parent. Also, parents who provided more help to their child with mental illness reported more gains than parents who were less involved in helping their child. A finding of interest is that the amount of help the parent provided was significantly correlated with the amount of assistance the child provided to the parent, suggesting reciprocity in the relationship. Parental reports of better overall child health and support group membership were significantly correlated with lower levels of subjective burden, whereas the amount of parental help was significantly correlated with higher subjective burden. There was no significant correlation between subjective burden and personal gains.
Effect of stressors and resources on personal gains
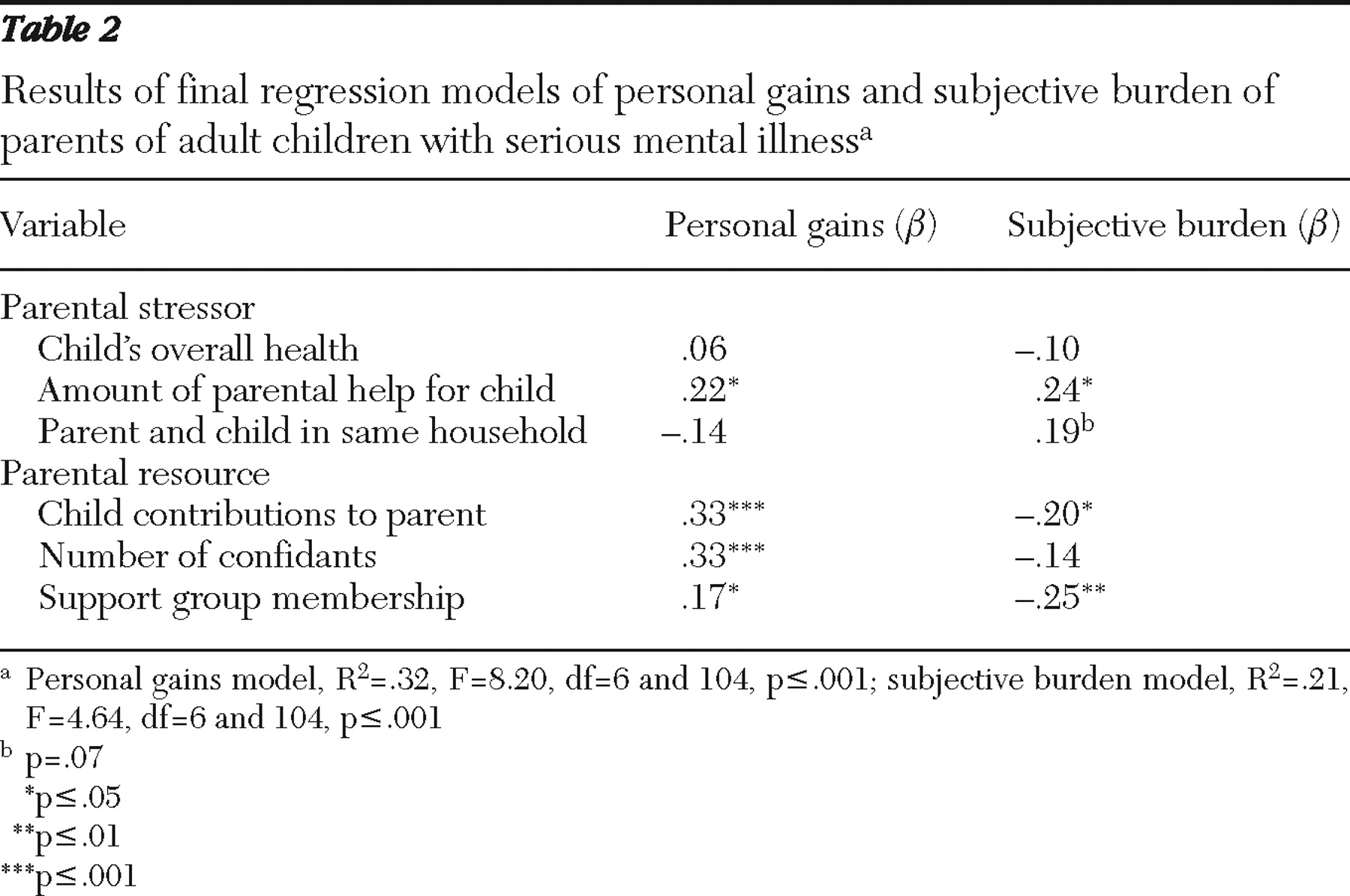
The results of the regression analysis are shown in
Table 2 . The overall regression model accounted for 32% of the variance in personal gains. Consistent with the bivariate relationships, parents who provided more assistance to their child with daily tasks experienced higher levels of gains than those who were less involved in assisting their child.
In terms of resources, parents who reported that their adult child with mental illness provided more assistance to them (with chores or with emotional support) experienced higher levels of personal gains. Consistent with our expectations, having more confidants was significantly associated with experiencing a higher level of personal gains. Finally, parents who participated in a support group reported significantly higher levels of gains.
Effect of stressors and resources on subjective burden
As shown in
Table 2, the overall regression model accounted for 21% of the variance in subjective burden. Among the parental stressors, parents who provided help to their adult child with a greater of number of daily living tasks reported significantly higher levels of subjective burden. There was a trend for parents who lived with their child to report higher levels of subjective burden than were reported by parents who lived apart. In terms of resources, the child's contributions to the parent's life were negatively and significantly associated with subjective burden. Parents reported lower levels of subjective burden when their adult child provided higher levels of instrumental and emotional support. Parents who were members of support groups, such as the National Alliance on Mental Illness (NAMI), reported, on average, lower levels of subjective burden.
Discussion
In this study we identified factors associated with subjective burden and personal gains among older parents of adults with serious mental illness. The stressors that were positively associated with subjective burden included the amount of help the parent provided to the child with activities of daily living, often referred to as objective burden, and living together in the same household. These findings are consistent with past research (
9,
22 ), and they underscore the potential lifelong challenges of coping with a child's mental illness. However, findings from this study also contribute to the growing evidence of the role of adults with serious mental illness as a source of support to their aging parents. The adult's contributions to their aging parent's life appeared to be particularly important in reducing burden and increasing gains. Receiving help from an adult child with serious mental illness not only may be an important source of tangible support for aging parents but also may serve to promote personal gains, as parents witness their child with mental illness assume increasing responsibility within the family. Furthermore, the positive and significant association between the amount of help the parent provided to the child and the amount of support the adult child provided to the parent suggests a degree of reciprocity in the relationship between aging parents and their adult child with mental illness that has rarely been discussed in the literature. It may be especially rewarding for older parents when reciprocal relationships are formed with adult children with serious mental illness who showed little capacity to reciprocate during earlier stages of their illness.
Findings from this study have implications for recovery-oriented services that strive to improve the self-efficacy and self-esteem of persons with serious mental illness as well as enhance the coping abilities of family members. According to Anthony (
37 ), recovery is a way of living a satisfying, hopeful, and contributing life beyond the catastrophic effects of mental illness. Gingerich and Mueser (
38 ) asserted that families often play a critical role in supporting persons with serious mental illness in the process of recovery. Thus mental health interventions that facilitate reciprocity between persons with serious mental illness and their family members may serve the dual purpose of helping persons with serious mental illness engage in meaningful life activities while also reducing feelings of subjective burden and promoting feelings of personal growth among the family members who care for them.
The finding that support group membership was positively related to personal gains and negatively related to subjective burden emphasizes its value for older parents of adults with serious mental illness. Participation in support groups (such as NAMI) through education and mutual support encourages parents to become advocates for their loved one, fight the stigma of mental illness, and take on various leadership roles. Thus it was not unexpected that family members who participated in support groups would report greater personal gains (such as learning new skills, developing a greater inner strength, and developing new friendships). Also, support groups provide a forum for sharing their child's journey of recovery from mental illness, which may help parents become more aware of their own growth and development through their personal journey in coping with their child's illness.
One of the unexpected findings in this study was the positive association between the amount of help the parent provided, often referred to as objective burden, and the parent's perceptions of personal gains. To our knowledge, the relationship between objective caregiving burden and personal gains among parents of adults with serious mental illness has not been examined in prior research. One plausible explanation for these findings is that the very stressors that tax parental caregivers may paradoxically challenge them to develop additional internal and external resources to cope successfully. This is in line with the concept of stress-related growth, which refers to the positive life changes that people make as a result of their struggles to cope with negative events and adverse situations (
39,
40,
41,
42 ). High levels of stress-related growth characterized by improved relationships with family and friends, a clearer sense of one's own strengths and resilience, and changed priorities and values have been documented among people facing a variety of stressful situations, including health problems (such as heart attacks and cancer), sexual assault, and bereavement (
43 ).
There are emerging qualitative reports of family members of persons with serious mental illness who indicate that giving care increased their feelings of resilience, improved their sense of self-worth, enhanced coping effectiveness, and provided them with a greater sense of purpose in life (
18,
44,
45 ). As Marsh and colleagues (
16 ) have pointed out, many families emerge from coping with the challenges of caregiving with a renewed sense of resiliency and personal strength. This may be especially true for older parents, who may have adapted to caregiving challenges over time by acquiring the resources and skills needed to cope effectively with their child's mental illness.
Our study had a few limitations. Although the design of the WLS circumvents many limitations associated with self-selected samples, there are two ways in which the initial recruitment procedures of the WLS might affect the generalizability of our findings. First, the racial composition of the WLS (99% white) reflects the composition of the Wisconsin population in the 1950s. Second, because all of the original respondents and the vast majority of sibling recruits (93%) completed high school, they were better educated than the general population of Wisconsin 18-year-olds in the 1950s, because 25% of 18-year-olds in Wisconsin at that time did not complete high school.
In addition, parents of children with disabilities completed the supplemental interview and self-administered questionnaire on their caregiving experience only if they had at least one telephone or face-to-face contact with their child in the year before the interview. Ninety-one (91%) of the respondents had at least monthly telephone or face-to-face contact with their son or daughter with mental illness, and 53% had contact several times a week or more. Thus, although there was considerable variability in the frequency and type of contact between the parents and their child with mental illness, the generalizability of study findings is limited to parents who continue to be involved in the life of their child.
Another study limitation is the use of parental reports of a child's diagnosis. It is possible that parents may have underreported the incidence of their children's mental illness because of the stigma associated with a mental illness diagnosis. Our sample was limited to those who self-identified as a parent of an adult with serious mental illness, and we confirmed this status through an extensive set of follow-up questions.
Nevertheless, the randomly selected community-based sample is a major strength of this study. In addition, the study sample of parents in their mid-60s provides a rare opportunity to examine the subjective burden and personal gains experienced by parents of adults with serious mental illness in later stages of the life course. Future replications of this research should include larger samples of older parents with varying degrees and types of contact with their adult children with serious mental illness to further investigate the heterogeneity in the experience of burden and gains among this unique group of parents.
Conclusions
Little research attention has been given to the experiences of older families coping with the challenges of serious mental illness. Only a small number of evidence-based interventions described in the published literature specialize in supporting aging parents of adults with serious mental illness. However, families—in particular, older parents—often provide a critical safety net of community support to adults with serious mental illness, which may become compromised as parents grow older (
46,
47 ). Empirical evidence about the strengths and vulnerabilities of families coping with serious mental illness in later life is needed to inform recovery-oriented services that can address the needs of older families.
Acknowledgments and disclosures
Preparation of this article was supported by grants R01-AG20558 and P01-AG21079 from the National Institute on Aging, grant T32-MH65185 from the National Institute of Mental Health, grant P30-HD03352 from the National Institute of Child Health and Human Development, and grant T32HS000011 from the Agency for Healthcare Research and Quality.
The authors report no competing interests.