Recent studies have documented that a large proportion of psychiatric patients have significant general medical comorbidity (
1). In addition, studies have shown the relative dissatisfaction of nonpsychiatric physicians with referrals to psychiatrists (
2). To examine these issues from the psychiatrist's perspective, in 1998 the American Psychiatric Association's Practice Research Network (PRN) gathered data on the nature and frequency of outpatient referrals from nonpsychiatric physicians to psychiatrists. This column examines the distribution of psychiatrists' patients who have a regular source of general medical care and the proportion of these patients about whom the psychiatrists communicated with the medical care provider.
Surveys were sent to 531 psychiatrist members of the PRN. A total of 435 psychiatrists returned the survey, of whom 413 reported spending time in an outpatient setting. For 368 of the respondents, data on type of outpatient setting where they spent time were available from a 1996 survey, and, for purposes of this analysis, these psychiatrists were divided into four groups according to where they spent the most hours. The groups were individual practice (N=180), group practice with other psychiatrists (N=29), group practice with other mental health disciplines (N=119), and group practice with other providers in mental health and general medicine (N=40).
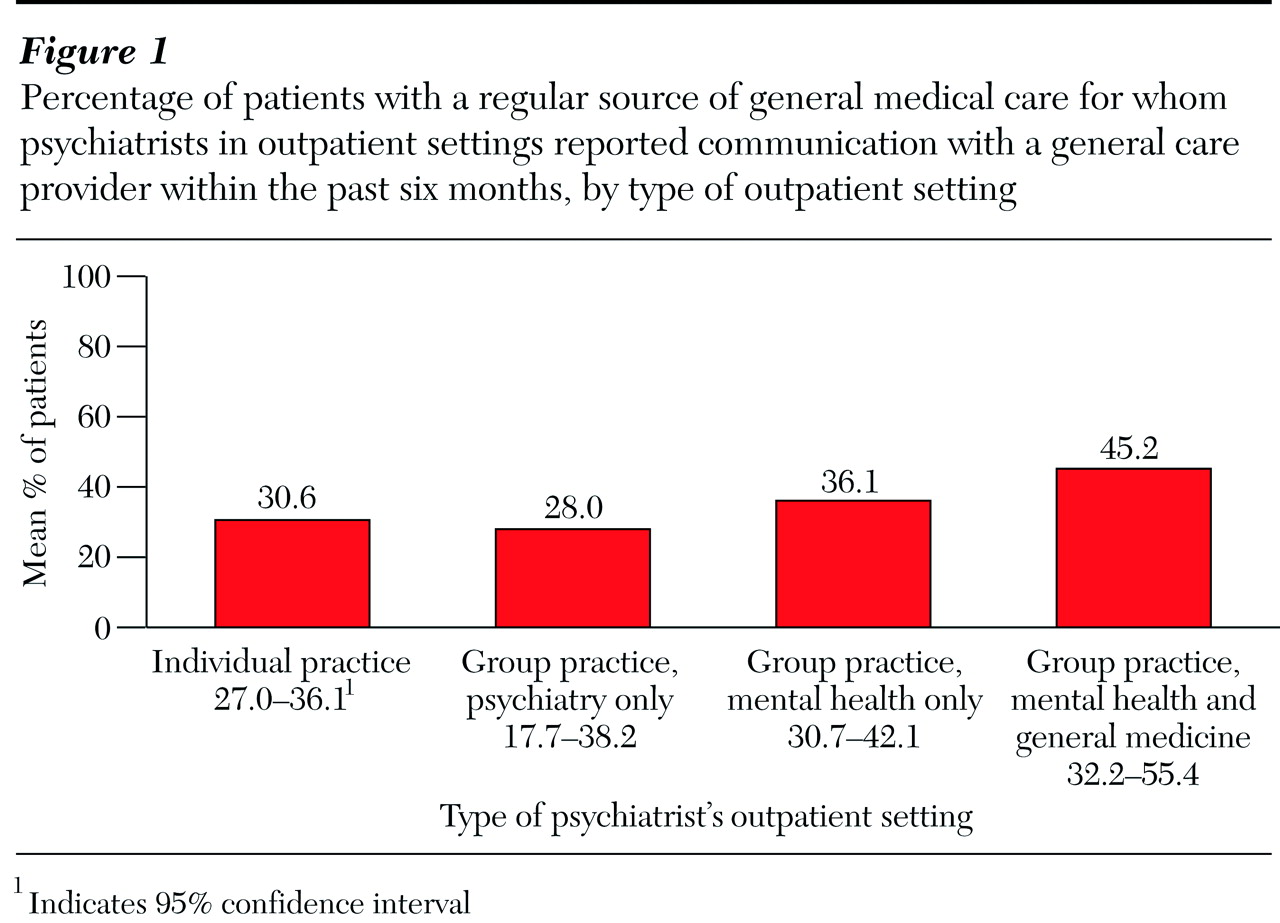
Overall, the psychiatrists indicated that 74.8 percent of their current patients had a regular source of general medical care and 21 percent did not. (In 4 percent of the cases, the psychiatrist did not know.) The percentage of patients with a regular source of care differed little between settings, ranging from 72.3 percent of patients seen in group practice with other psychiatrists to 76.5 percent of patients seen in individual practice. For 35 percent of patients who had a regular source of general medical care, the psychiatrist reported having communicated with the other physician within the past six months. As
Figure 1 shows, communication was highest in group practices that included providers in both mental health and general medicine.
In summary, approximately three-fourths of psychiatric patients were receiving general medical care from another provider, but in most cases psychiatrists were not in regular contact with the other provider. The study showed a trend toward increased communication in practices that included both general medical physicians and psychiatrists. These issues will be explored in future PRN studies.
Acknowledgments
The Practice Research Network acknowledges the support of the John D. and Catherine T. MacArthur Foundation and the Center for Mental Health Services. The authors thank Allen Dietrich, M.D., John Williams, M.D., Tom Oxman, M.D., and Paul Nutting, M.D., for their contributions to this study.