Although psychiatric problems are prominent in general medical care, psychiatry and primary care medicine, for the most part, are not integrated. This separation has been created and maintained by several factors including medical specialization, a prevailing model of mind-body dualism, differences in languages and practice styles, and the stigma of mental illness. More recently, the gap separating psychiatry from primary care has been further widened as a result of mental health "carve-out" insurance plans that finance mental health services separately from general medical benefits in an effort to control costs.
Mental health carve-out plans have resulted in some short-term cost reduction, but often by limitation in benefits. Carve-out plans also reinforce the separation of psychiatry from the rest of medicine. This separation poorly serves the majority of patients with mental health problems who receive a large proportion of their care in the general medical sector rather than in the mental health sector (
1,
2). Patients with mental disorders constitute 5 to 20 percent of general medical patients and are one and a half to two times as likely to visit a medical setting as are patients without those disorders (
3,
4). However, there is a significant lack of attention to mental disorders in general practice, and most cases are poorly recognized or undertreated (
5,
6,
7,
8,
9,
10).
Psychiatric problems have a significant impact on the presentation and course of many medical symptoms and disorders (
11). Depression is a common problem, with an estimated prevalence of 12 percent in primary care practices (
12). Furthermore, depression has been shown to adversely affect the course of patients with a variety of medical disorders (
13,
14). Both generalized anxiety disorder and panic disorder are common among patients treated in medical practice and often present as somatic symptoms that may lead to ongoing medical interventions (
15,
16). Tobacco, drug, and alcohol use are associated with significant health care costs and are often treated inadequately despite good evidence that a positive medical cost offset can be obtained from their treatment, particularly from treatment of alcoholism (
17,
18).
Despite the prevalence and impact of behavioral problems, few primary care programs are tightly coupled to psychiatry programs. Most primary care physicians are frustrated when they attempt to refer patients to the mental health sector or attempt to integrate their care with mental health care. Despite growing economic evidence of the value of integration, financial incentives maintain the gap, and these incentives continue to deter efforts to create more integrated care models. To overcome this gap providers must believe in the value of integration, but, more important, payers must initiate shifts in financial incentives to promote change in practice among providers. This paper discusses the financial incentives that influence efforts to integrate psychiatric care and primary care.
Varieties of incentives
In daily practice, physicians face forces that are intended to modify treatment based on payment (
19). By examining the financial incentives that operate in a variety of practice scenarios, providers can more effectively analyze the barriers to integration and understand the need for new fiscal structures to meet new opportunities.
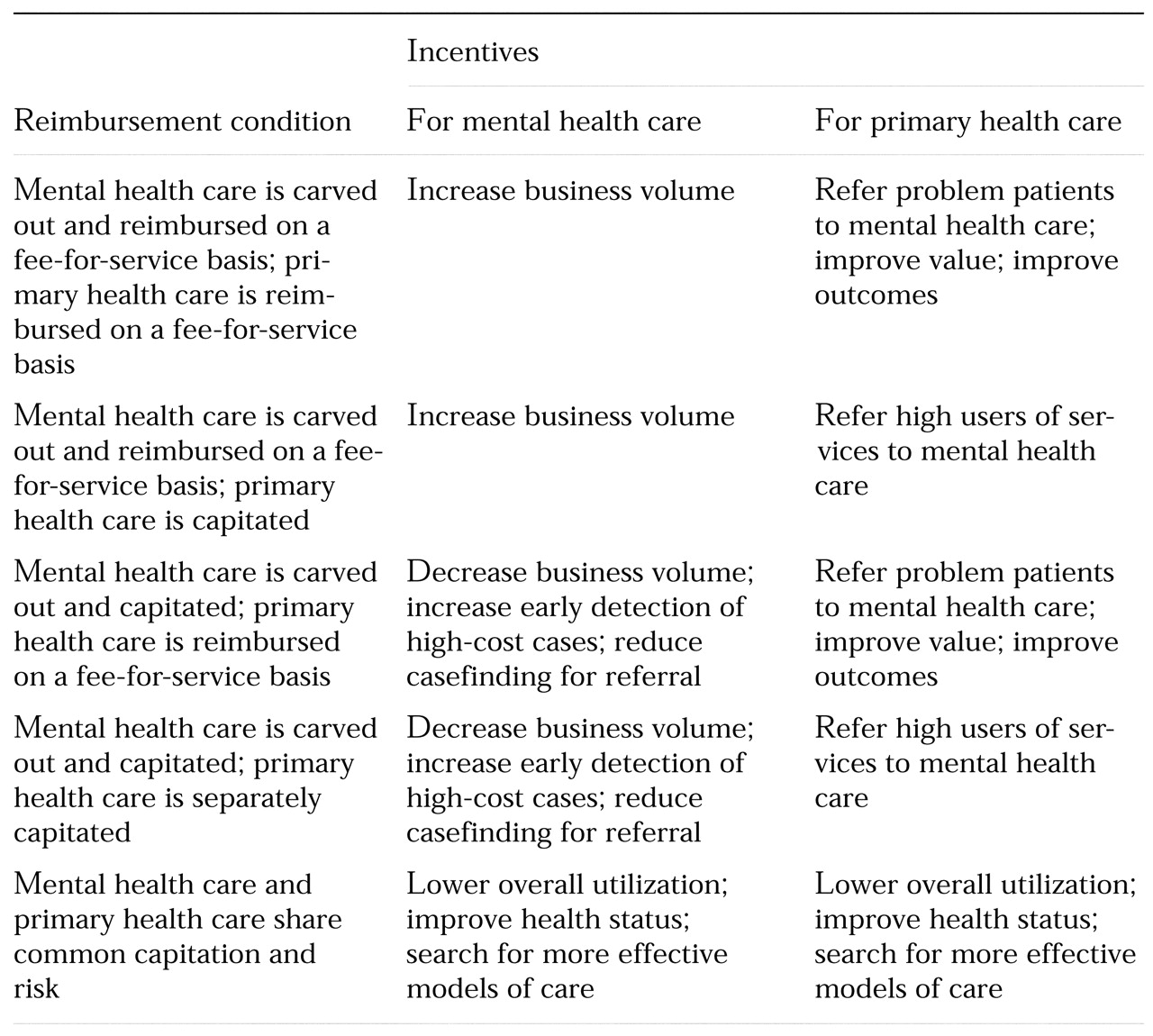
Table 1 summarizes the major reimbursement conditions that govern clinical practice. The combinations of conditions linking psychiatry and primary care determine the forms that clinical services take or maintain.
Two major reimbursement conditions have governed much of mental health care. Under the first condition, coverage of mental health care is carved out from coverage of primary health care, mental health care is usually managed through utilization review, and clinicians are paid on a fee-for-service basis. Under the second condition, coverage of mental health care is carved out, and care is managed through utilization review, but payment to clinicians involves some type of capitation or risk-sharing arrangement.
Similarly, two major reimbursement conditions have governed primary care practice. Under the first condition, primary care is paid for on a fee-for-service basis with varying amounts of utilization review. Under the second condition, payment for primary care involves some type of risk-sharing arrangement.
Less common is a third type of reimbursement in which both mental health care and primary health care participate in a shared-risk arrangement. This arrangement is the only current model that provides incentives for integrating psychiatric care and primary health care.
Traditional reimbursement
The combination of the first reimbursement condition governing mental health care and the first condition governing primary care represents the pairing of "traditional" incentives. Psychiatrists operate within a fee-for-service model. Because high volume is rewarded, psychiatrists do what they can to build and maintain referrals through personal contacts, quality initiatives (improving accessibility and communication), or a more flexible approach to practice (moving locations or changing office hours).
The primary care providers also have an incentive to build business volume. Therefore, they are likely to refer patients to psychiatry only if such referrals increase their throughput of patients. Such primary care providers may refer time-consuming cases, problem cases, or cases with problematic insurance coverage. Some primary care providers find that a close relationship with psychiatry improves the perceived value of their practice. Some patients value the collaboration, and staff may feel less frustration finding and making referrals. Some primary care providers take pride in establishing an informal integrated model of care and believe that such services improve patient outcomes.
However, apart from the values of individual physicians, no incentives are built into the payment system for identifying cases that could benefit from integrated care. In almost all cases, the extra time and effort required to create integration are not reimbursed. Collaborative treatment planning and coordination coded in the Current Procedural Terminology rarely triggers payment. Furthermore, most programs have lacked the information systems to target patients with a history of high utilization of services or suboptimal outcomes who might benefit from integrated care.
In general, under these reimbursement conditions, primary care providers complain that they cannot find a psychiatrist to whom patients can be referred or cannot easily make an appointment with one and that they often do not hear back from the psychiatrist about the outcome of the referral. Psychiatrists who are already busy have little incentive to spend extra time communicating with a primary care provider. In the overall health care plan, utilization management, if it occurs, is external to the providers and consists of containment by preauthorization and concurrent review, with excessive dependence on denial of care.
Mental health carve-out plans
When mental health care is carved out but psychiatrists continue to receive fee-for-service payment and primary care is capitated, psychiatry continues to have the incentives related to fee-for-service payment that were described in the preceding section. However, primary care providers under capitation have a clearer incentive to identify and move high utilizers out of their practices into the mental health sector. Psychiatry, with fee-for-service payment, does not mind receiving such referrals, assuming they come with insurance coverage and have not exceeded their annual or lifetimes limits for mental health care.
For the overall health care plan, such shifting of patients from primary care to mental health may result in more efficient and effective psychiatric treatment for some patients (
20). At the same time, the overall plan may become concerned about any systematic attempts to identify and refer psychiatric cases, because such increased case identification could increase overall costs. Besides concurrent review mechanisms, the overall plan will employ benefit limits as well as increased copayments and deductibles to discourage utilization. Plans will have little incentive to systematically identify psychiatric cases or to try to detect underutilization of psychiatric services.
Capitated mental health care
When mental health care is carved out and capitated and primary care is reimbursed on a fee-for-service basis, the situation dramatically changes for the psychiatrists. This combination of reimbursement conditions is common because mental health benefits have been shifted into alternative financial models earlier than general medical benefits. Primary care providers continue to have fee-for-service incentives while psychiatrists labor under a system involving capitation that forces them to reconsider their incentives.
Under capitation, psychiatrists must manage a population within a limited amount of money. They no longer have the incentive to build business volume. They become ambivalent about building bridges with primary care providers because of concern that the primary care providers will start to identify and refer more cases, thus cost-shifting cases out of the medical benefit into the mental health capitated budget.
At the same time, psychiatry must also be concerned that inadequate treatment of psychiatric disorders by primary care providers may bring patients who are more severely ill, and therefore more expensive to treat, when referrals do take place. For example, a primary care provider may unsuccessfully treat a severely depressed patient for several months and refer the patient only after the emergence of a psychotic component requiring a hospitalization, which could have been prevented by more effective earlier treatment.
Because primary care providers treat a population of patients with a variety of insurance arrangements, psychiatrists also face the dilemma of wanting to discourage some referrals and encourage others. The psychiatrist who discourages referrals because of a capitation issue thus faces the probability that the primary care provider's fee-for-service business will go also elsewhere. The incentive for the overall plan would be to shift business (and risk) into the mental health sector, because the dollars at risk there are capped and predetermined no matter how much care is provided. Once the mental health sector has a capitation system, insurance plans would tend to become interested in new initiatives to educate primary care providers and new ways to "reduce" inappropriate prescribing of psychotropic medication by primary care providers.
Separate capitation
When mental health care is carved out and mental health care and primary care are separately capitated, the most intense cost-shifting tensions emerge. Psychiatrists have the incentive to limit referrals, but this incentive is tempered by the possibility that more severely ill patients may be referred at a later stage of illness. Primary care providers have the incentive to shift care into the mental health sector. Psychiatrists who had previously been strong proponents of primary care screening and referral of mental health problems now feel that their medical colleagues are perfectly capable of providing mental health care. After all, many psychiatric interventions help control medical benefit expenditures more than expenditures for psychiatric problems.
Under separate capitation, both parties become acutely aware of spending under their capitation budgets, and collaboration becomes the victim. Separate capitation is, therefore, inherently unstable and should lead psychiatrists and primary care providers to discuss the possibility of shared capitation, under which true integration of mental health care and primary health care can develop.
Shared-risk model
Shared capitation—in which mental health care and primary health care share common capitation and risk—is the only model that provides true financial incentives for integration of care. The incentives of both sides are aligned in a shared motivation to lower overall utilization, improve patients' overall health status, and search for more effective integrated care models. Integration with financial risk sharing can be approached from either a global or a selective perspective. In the global perspective, mental health and primary care allocations are combined with common provider payment withholds and incentives based on the total performance of the integrated care system. In the selective perspective, costs for subgroups of patients with histories of high utilization of services are identified, and gain-sharing is based on exceeding specified performance targets.
Discussion and conclusions
Primary care providers often do not have the time, training, or incentive to provide necessary components of behavioral health care. Depressed patients in the primary care setting receive some counseling in less than 50 percent of cases, and less than 10 percent are referred to mental health specialists (
21). The specialty-oriented, fee-for-service system of the past has reinforced neglect of psychiatric problems through poor reimbursement for psychiatric codes and incentives to pursue medical diagnostic testing. For example, patients with medically unexplained symptoms often receive repeated medical testing before consideration of whether an underlying depression or anxiety disorder could account for the symptoms. A shared-risk model avoids cost-shifting battles and creates new incentives that reward recognition and treatment of behavioral problems that would otherwise lead to more extensive utilization of primary health care or psychiatric care.
Psychiatric problems affect resource utilization through increased length of stay (
22,
23) and problems in long-term recovery (
24,
25,
26,
27). In general, however, psychiatric comorbidities are not recognized and are poorly documented (
28,
29). Psychiatric consultation for medical inpatients with psychiatric complications has been shown to produce a positive cost offset (
30,
31) and can improve the effectiveness of treatment (
32,
33,
34). Although a growing body of evidence suggests that psychiatric treatment can reduce outpatient (and inpatient) medical utilization (
35), more randomized prospective trials of psychiatric interventions for medical outpatients are clearly needed (
36).
The large numbers of psychiatric problems among patients in primary care will require some shifting in the allocation of financial resources. Only about 2 to 4 percent of overall medical expenditures are now accounted for by expenditures in the mental health sector outside the primary care setting (
37). However, it is estimated that another comparable amount is spent on mental health care within the general medical sector, and that beyond that amount, $81 million is spent on the medical symptoms resulting from behavioral health disorders (
38). These dollars can be used more efficiently if care is integrated (
39,
40). New efficiencies will emerge from elimination of unnecessary interventions, shifts in utilization of primary health care, and savings from lowering duplicative administrative costs.
The shared-risk model has existed for years in staff-model HMOs. These organizations have the opportunity to think in terms of overall costs and also have a captive (employed) provider group for whom care management standards can more easily be promulgated and monitored. Nevertheless, such organizations usually operate by limiting mental health services utilization, with little effort to create cross-discipline interventions. These interventions—for example, those reported by Katon and associates (
41) involving intervention with high utilizers—seem limited to a small number of programs with academic interests. The barriers that remain include the prevailing dualistic model of illness, lack of educational attention, the stigma of mental illness, and the separate cultures of psychiatry and general medicine (
42).
Besides the long-standing barriers to integration, financial pressures are now making every provider wary of further decreases in the pool of patient care dollars. Primary care providers will be wary of losing potential reimbursement to increased mental health services unless they feel they can benefit from the cost savings in utilization of primary health care. The groups that control mental health dollars tend to protect their shrinking pool of dollars rather than face the unknown of collaboration with primary care. These struggles contain the opportunity for a renewed recognition of the interaction of the physical and mental life of patients and the need for a reintegration of care. This impulse to address the mind-body connection more effectively is probably part of the impetus behind the recent explosion of interest in alternative medicine. Finally, although research into cost-benefit results is likely to be a strong driving force, it is also important to consider the integration of psychiatry and medicine because it addresses patients' problems most comprehensively and sensibly.
Acknowledgment
The author thanks Joel Kaufman, M.D., for comments on the manuscript.