Mental problems represent one of the major causes of disability in the United States for people between the ages of 15 and 44 and are a prime driver for the use of health care services (
1,
2). The proximate cause of help-seeking behavior among people with mental illness is often related to the experience of general physical symptoms of both known and unknown origin (
3). Most patients experiencing physical symptoms obviously seek help first from their primary care provider, and those with coexistent physical and mental health symptoms account for as much as half of annual primary care visits (
4,
5). Because most people with mental disorders use primary care long before they seek specialty mental health services, primary care has been dubbed the “de facto mental health system” (
6). In up to 30% of cases presented (
5), the origin of physical symptoms experienced by primary care patients remained unexplained. In the past, these cases were referred to as medically unexplained physical symptoms or multiple unexplained physical symptoms (
7).
Recent studies that have examined the relationship between physical symptoms and mental illness have concentrated on the co-occurrence of these conditions within primary care practices and community settings and have largely focused on multiple unexplained physical symptoms (
8–
11). Such studies have indicated that presenting physical symptoms that do not have a clear medical explanation are much more disabling than those of physical illness or other mental disorders such as depression. These studies have also shown that the number of somatic symptoms presented is a clinical indicator of comorbid mental illness, most often anxiety or depression (
12,
13). In addition, some studies have suggested that ascertaining whether symptoms are medically explained is both time consuming and complicated and often proves a barrier in and of itself to the diagnostic process and the formulation of treatment (
11,
12,
14).
The study of the co-occurrence of physical symptoms and mental disorders and the prediction of outcomes such as service use have benefited from the development of somatic symptom indices for studies in primary care settings and community populations. The use of somatic symptom counts to identify comorbid psychopathology required cataloging lifetime experience of medically unexplained physical symptoms (
7,
15), a method later proven to be problematic because of the lack of reliable historical reporting and the absence of “gold standards” to define a symptom as medically explained (
10,
16). This led clinicians to limit their inquiry to currently experienced symptoms.
Recent studies by the World Health Organization and by Kroenke and colleagues (
17) have shown that within clinically defined populations, whether medically explained or not, as the number of physical symptoms increases so do the odds for coexistent psychiatric conditions (
10,
17,
18). As a result of these and other studies, the somatic symptoms workgroup for
DSM-5 has proposed to eliminate the medically unexplained distinction for the diagnosis of somatoform disorders (
19).
Using a list of 14 physical symptoms to investigate the association of physical symptoms and mental illness in a large community-based population, Escobar and colleagues (
14) found that regardless of medical explanations, having a high number of these symptoms was strongly correlated with the presence of common mental disorders such as depression and anxiety. Thus, regardless of explanation, having three or more physical symptoms was associated with psychopathology and service use.
Among the studies discussed thus far, the prevalence of physical symptoms and mental health conditions in primary care and community settings and the association of physical symptoms and health services use were analyzed retrospectively. Less is known about the prospective implications and usefulness of identifying prevalence of physical symptoms for treatment planning and predicting services use and cost. In addition, little information has been available on physical symptoms of patients with serious mental illness who present for admission to mental health specialty settings. This study explored the relationship between patients' serious mental illness and physical symptoms at the time of intake and the ability of the physical symptoms presented at intake to predict patients' mental health services use during a follow-up period among those treated at a community-based mental health center.
In the context of this article, it is important to emphasize that the physical symptoms of a patient who has a serious mental illness must not be considered less important than (or derivative of) his or her psychiatric symptoms or interpreted as somatization. People with a mental illness have more general medical comorbidities and die, usually from medical diseases, at a much earlier age than the general population. In particular, physical symptoms of persons with serious mental illness may result from untreated physical illness, especially because many persons with serious mental illness, including the patients in this study, lack access to primary care. Such symptoms may also result from psychotropic medication side effects, either directly (for example, medication triggers nausea or headache) or indirectly (for example, weight gain secondary to the use of second-generation antipsychotics may in turn trigger pain in the back or extremities).
Methods
Site, sample, and data
The subjects in this study were patients presenting for services at University Behavioral HealthCare (UBHC) of the University of Medicine and Dentistry of New Jersey. UBHC is one of the largest mental health specialty providers in the United States, serving about 15,000 individuals per year. The UBHC mental health delivery system has several outpatient and partial hospitalization clinics, case management, residential programs, an emergency room, and a small inpatient unit. The composition of the UBHC client base includes about 56% clients on Medicaid or Medicare and about 20% uninsured or self-pay clients. Data were obtained during intake calls on a toll-free number to a centralized Access Center that coordinates admissions to UBHC.
The Access Center at UBHC provides a centralized point of entry for all major UBHC behavioral health care services. Initial information and screening for these services are accessed statewide by calling a single toll-free 800 number. Mental health professionals handle these calls, carry out an initial assessment and triage, and schedule services at the appropriate level of care (for example, outpatient or partial hospitalization). During the period in which the study was conducted (August 2006 to September 2007), callers were asked to respond over the phone to the 15-item modified Patient Health Questionnaire (PHQ-15) about current general physical symptoms. This request occurred after the regular intake procedure for UBHC was completed and at a point where the caller and clinician would normally end the call.
Two modifications were made to the PHQ-15 for phone administration of the survey: The introductory question was changed slightly to “During the past month, have you been bothered a lot by [symptom]?” and a binary scale (yes-no) was used to catalog responses, instead of the traditional trichotomous scale of bothered not at all, a little, or a lot. Symptoms queried included (in order asked) stomach pain; back pain; pain in arms, legs, or joints (knees, hips, and so on); menstrual pain or problems; pain or problems during sexual intercourse; headaches; chest pain; dizziness; fainting spells; feeling heart pounding or racing; shortness of breath; constipation, loose bowels, or diarrhea; nausea, gas, or indigestion; feeling tired or having low energy; and trouble sleeping. Callers were read a script (available from authors upon request) stating that participation was not required to receive services; that they would not be identified in any reports describing their physical symptoms or other information, published or otherwise; and that they could stop the process at any time. The UMDNJ institutional review board approved this informed consent procedure before the study.
Additional information was tracked for the subset of patients making at least one visit after the intake phone call. The tracking period extended to January 2008, allowing the use of a 16-month tracking window for every patient entered into the study. The data tracked included psychiatric diagnosis, number of services used, and cost of services provided. Number of services used included outpatient visits, partial hospital days, and inpatient days. Tests, injections, and similar ancillary services were excluded. Patients not showing up for at least one appointment were excluded on the basis of lack of data for the variables of interest.
Overview of statistical analyses
During the study period, 1,160 of the 2,187 persons who called the Access Center were asked to participate in the study; 158 refused and 1,022 agreed and responded to the PHQ-15 over the phone.
Statistical analyses were based on a subset of patients who showed up at UBHC for at least one appointment (N=682). Patients who kept their first appointment reported a mean±SD of 6.3±3.4 physical symptoms, whereas the patients who were “no shows” reported 6.4±3.4 symptoms. This difference was not significant.
In order to eliminate frank confounding of physical symptoms with psychiatric symptoms, we eliminated “fatigue” and “sleep problems” from all statistical analyses, as Escobar had done previously in the case of his somatic symptom inventory. (Escobar's inventory is very similar to the PHQ-15. In fact, 12 of the symptoms are identical.) We omitted these items so our findings would be more comparable with those from the community study (
14). In addition to eliminating “fatigue” and “sleep problems,” Escobar and colleagues eliminated “headaches.” However, they added two pseudoneurological symptoms—“trouble swallowing/lump in throat” and “numbness or tingling in body or extremities”—because these symptoms had been found to be more discriminating for psychopathology in a previous study in primary care (
20). In addition to eliminating “fatigue” and “sleep problems,” we eliminated two other symptoms from the PHQ-15 rarely endorsed by males (“menstrual pain” and “painful intercourse”). These adjustments rendered the PHQ-15 in our study, in effect, a “PHQ-11.”
Statistical analyses performed included a comparison of patients who reported three or more symptoms with patients who reported fewer symptoms with respect to the following covariates: age, gender, language, diagnostic category, and service use and cost. Total scores on our PHQ-11 were also examined with respect to the same covariates. Statistical tests comprised t tests and F tests for continuous variables and chi square tests for discrete variables. Subsequently, logistic regression was used for a side-by-side comparison of two distinct thresholds for defining a “case” involving multiple physical symptoms: a cutoff of three or more symptoms versus a cutoff of six or more symptoms. For either set of thresholds, a binary dependent variable, corresponding to a particular threshold, was logistically regressed on all covariates, which were entered simultaneously. Finally, service use and cost were analyzed as a function of physical symptoms (threshold of three or more or six or more) and all other covariates, entered simultaneously in multiple regressions.
Estimates of costs of services were derived by multiplying units of service used by an estimated average cost for each service type (
21). The average cost amounts were derived from Medicare physician fee and hospital outpatient service reimbursement schedules. Starting with Medicare fees that were adjusted for the cost of living in New Jersey, we calibrated the Medicare fee amounts to reflect the average costs of outpatient mental health clinical programs at UBHC. Average annual costs for the outpatient mental health clinical programs at UBHC were drawn from accounting records. As a result of this calibration, summations of estimated service delivery costs across service categories accurately reflected the organization's total costs for those services (personal communication, Slade E).
Results
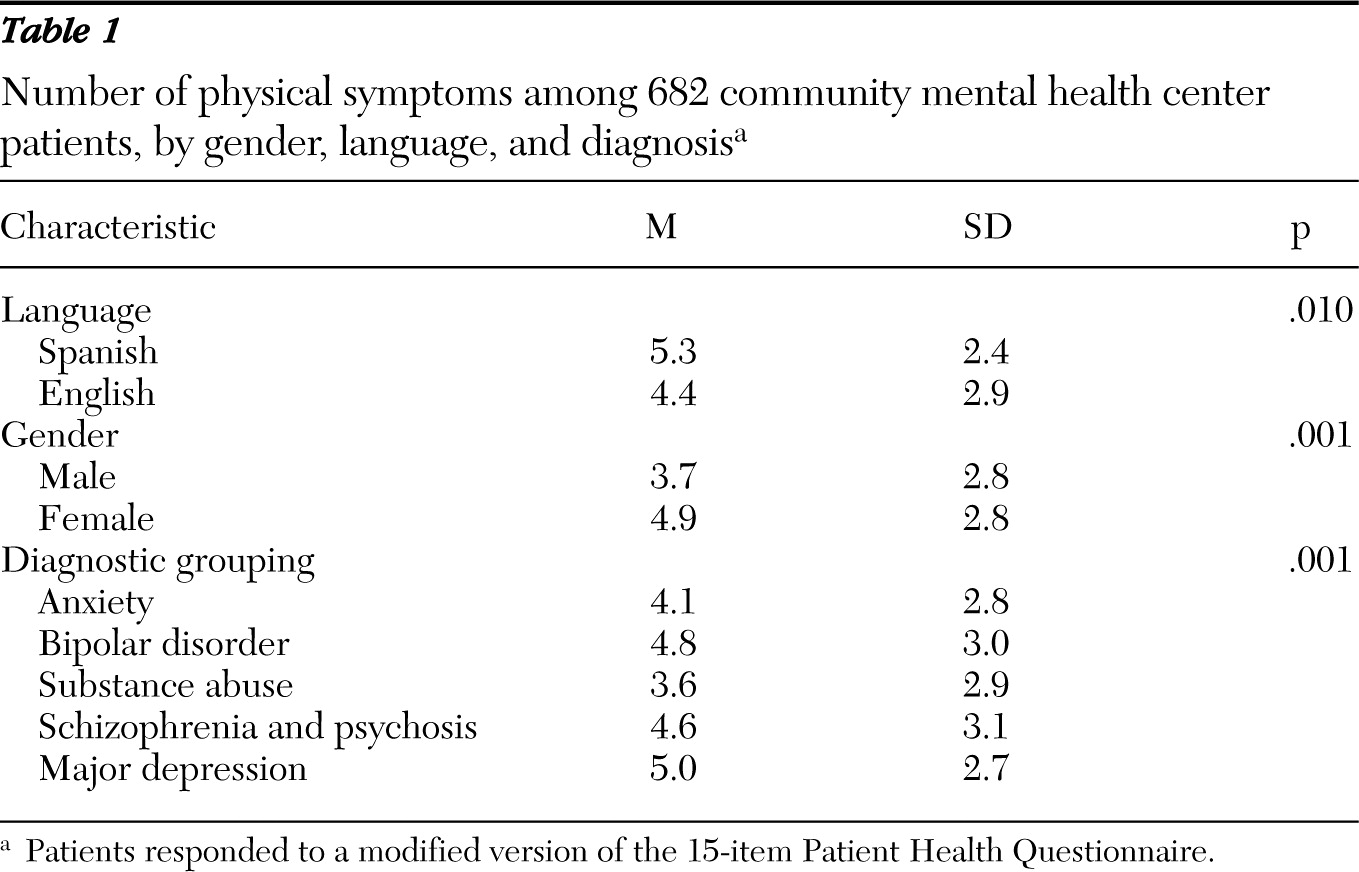
Pearson correlations between the total number of symptoms reported on our PHQ-11 and the two continuous covariates were .11 (p=.004) for age and .13 (p=.001) for number of services. Total number of symptoms by gender, language, and diagnostic category are presented in
Table 1. Differences in the total number of symptoms reported were significant for language (p=.010), gender (p=.001), and diagnosis (p=001). Significance levels were computed with analysis of variance for the latter and with t tests for the continuous variables.
In the sample of 682 patients whose data were available for analysis by virtue of the patients' having kept at least one appointment, 576 or 85% reported three or more general physical symptoms on the PHQ-15. As noted in the previous section, four symptoms were eliminated from the PHQ-15 prior to further analysis. Using this truncated inventory (PHQ-11) of physical symptoms, we found that 481 patients (71%) reported three or more symptoms and 257 (38%) reported six or more.
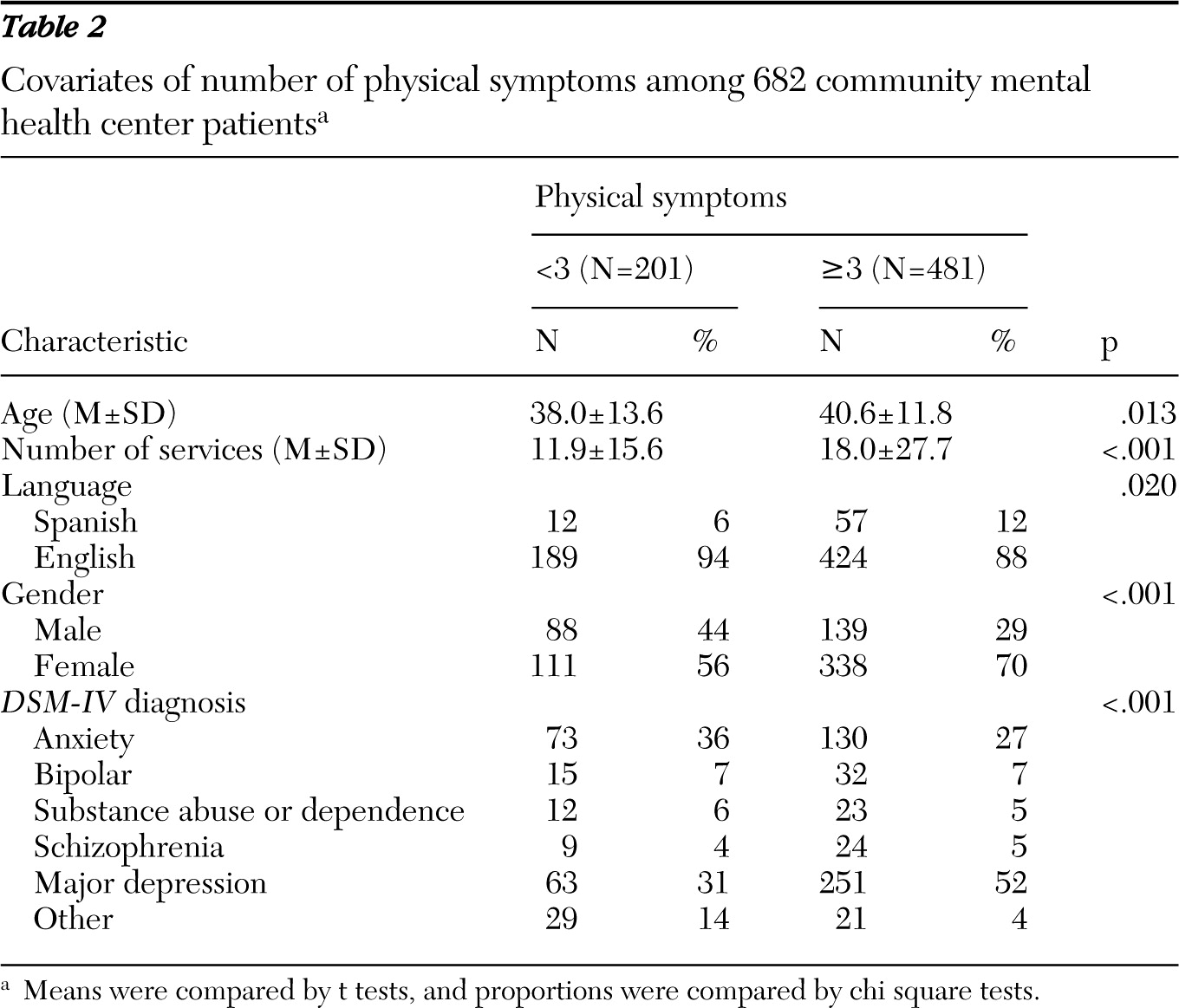
As shown in
Table 2, patients with fewer than three physical symptoms were younger than those with three or more, and they used fewer services. Also presented in
Table 2 by physical symptoms group are frequencies and percentages for language spoken (English or Spanish), gender (male or female), and diagnostic group. Diagnostic groups identified included anxiety, major depression, schizophrenia, substance abuse or dependence, bipolar disorder, and “other.” Included in the miscellaneous group were adjustment disorders, personality disorders, a small number (N=5) of cases of adult attention-deficit hyperactivity disorder, V codes, and disorders from a medical condition (N=3), as well as disorders that occurred in the sample only once. As shown in
Table 2, patients with three or more symptoms were significantly more likely to be female (p<.001) and to speak Spanish (p<.05). There was also a significant effect of diagnosis (p<.001), where “other” disorders were least likely to meet criteria for three or more symptoms and major depression was most likely to meet such criteria.
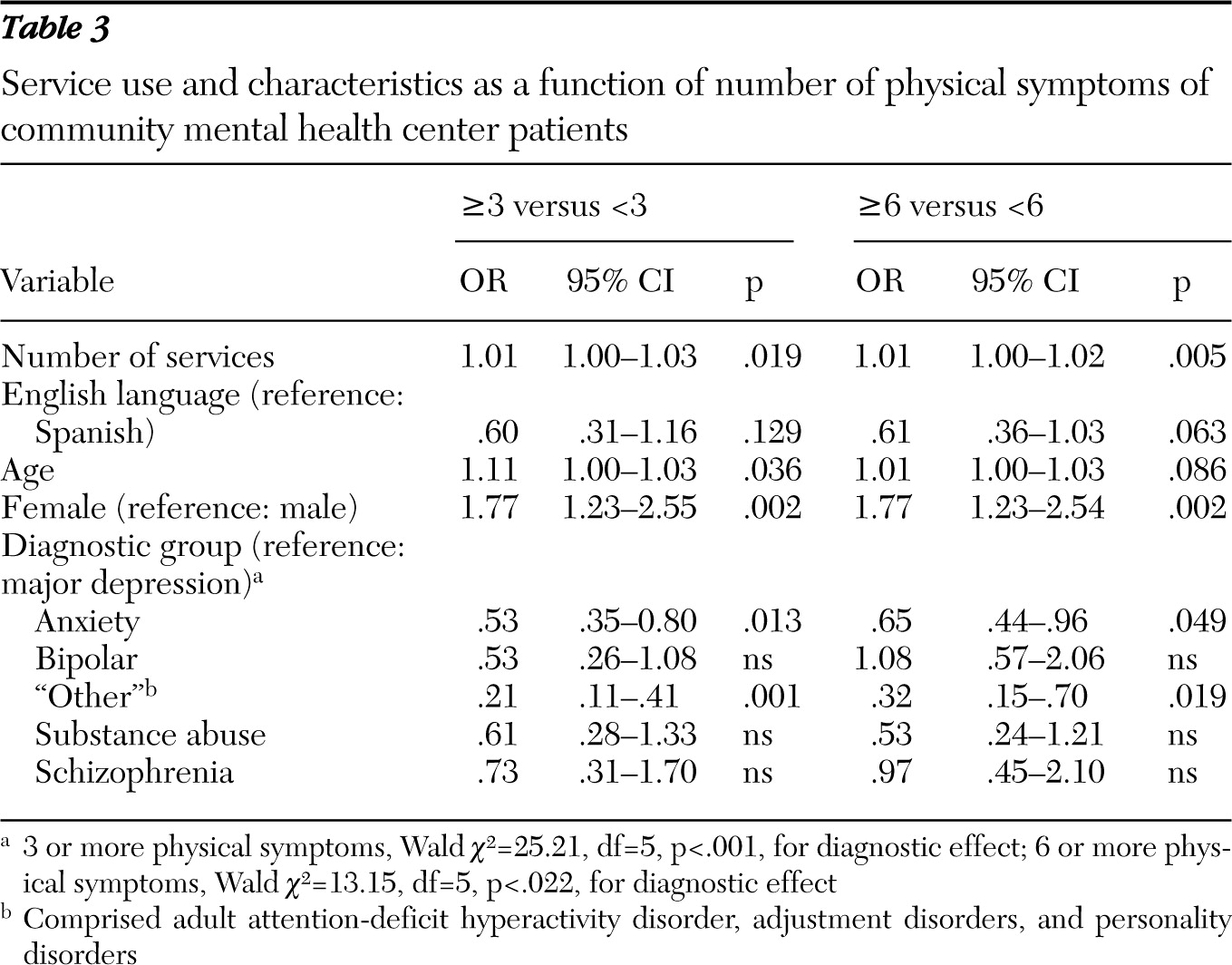
Table 3 enables a side-by-side comparison of the two distinct thresholds for defining a “case” involving multiple physical symptoms (three or more and six or more). For each threshold, we used logistic regression to relate a binary variable corresponding to whether or not a given patient met criteria for a case of multiple physical symptoms. There were two regressions, one for three or more and one for six or more physical symptoms. In each regression, all five covariates were entered simultaneously; hence, each odds ratio (OR) shown for a given regression controlled for all other covariates within that same regression.
As shown in
Table 3, statistically significant effects were found for number of services, gender, and diagnostic group in both sets of analyses but were not found for language. The effect for age was statistically significant with the threshold of three or more symptoms but not with the threshold of six or more symptoms. Logistic regression results indicated comparable ORs for each covariate in
Table 3, regardless of which cutoff was used to define a case.
Service use
Using multiple regression, we found that patients with three or more physical symptoms used significantly (p<.05) more services than did persons with fewer than three symptoms, after adjusting (via multiple regression) for all covariates listed in
Table 1 (F=5.16, df=1 and 663, p=.023). Adjusted mean service use for patients with three or more symptoms was 17.6 (95% confidence interval [CI]=13.6–21.5), whereas adjusted mean service use for patients with fewer than three symptoms was 12.7 (CI=8.0–17.4). In a parallel regression, patients with six or more symptoms were found to use significantly (p<.002) more services compared with persons with fewer than six physical symptoms (F=9.67, df=1 and 663, p=.002). Adjusted mean service use for patients with six or more physical symptoms was 19.8 (CI=15.4–24.2), whereas adjusted mean service use for patients with fewer than six physical symptoms was 13.7 (CI=9.6–17.7). Given these confidence intervals, the threshold of six or more symptoms appeared to be a better predictor of service use compared with three or more symptoms.
Significant Pearson correlations (p<.05) between individual symptoms and service use were, in order of decreasing magnitude, pain in legs or joints (r=.16), back pain (r=.15), stomach pain (r=.09), dizziness (r=.09), and shortness of breath (r=.09).
Service costs
We performed multiple regressions for service costs parallel to those in the previous section, using the same covariates as before, plus a binary variable corresponding to program type (inpatient and partial hospitalization versus outpatient).
Square root transformation reduced skew in cost data. We found that patients with three or more physical symptoms generated significantly (p<.005) more billable costs than did persons with fewer than three physical symptoms, after we adjusted (via multiple regression) for all covariates, including program type and diagnosis (F=7.95, df=1 and 654, p=.005). Adjusted mean service costs for patients with three or more physical symptoms were $1,315 (CI=$912–$1,790) with a median cost of $1,089, whereas adjusted mean service costs for patients with fewer than three physical symptoms were $983 (CI=$645–$1,414) with a median cost of $801. In a parallel regression, we found that patients with six or more physical symptoms generated significantly more costs than did patients with fewer than six physical symptoms (F=17.14, df=1 and 654, p=.001). Adjusted mean service costs for patients with six or more symptoms were $1,515 (CI=$1,069–$2,034), with a median cost of $1,203, whereas adjusted mean service costs for patients with fewer than six symptoms were $1,045 (CI=$697–$1,459), with a median cost of $899. Examining costs separately by program type for patients with fewer than six symptoms, we found that the median service cost for inpatient or partial hospitalization was $4,397, and for outpatient services it was $880. For those with six or more symptoms, the median inpatient or partial hospitalization cost was $22,127, and the median outpatient cost was $1,195.
Discussion
We found that a large majority of patients (over 80%) presenting to a community mental health center endorsed a relatively high number of physical symptoms. This was a much higher percentage than the one Escobar and colleagues (
14) reported in their large community sample (11%) and confirms that physical symptoms are an important component in the presentation of psychopathology, especially in a population seeking specialty mental health treatment. We found that the presence of high levels of physical symptoms was a significant predictor of service use and cost. Furthermore, the higher the level of reported physical symptoms, the more pronounced the increase in service use and cost, even after we controlled for the effect of patient diagnosis on service use and costs as well as for other confounds.
The association between physical symptoms and mental health service use and costs may have different explanations. The simplest one is that more impaired persons need more services and are more likely to use recommended services. However, it is well established that higher impairment does not always lead to acceptance of treatment or consistent follow-up. It should also be noted that the cost estimates provided herein are incomplete, given limitations in the data set. That is, we captured only mental health service use and costs and were not able to capture total health-related service costs. It is reasonable to assume that total costs for serious mental illness with physical symptoms would be higher than reported herein.
In any event, the fact that the number of physical symptoms was a significant predictor of mental health service use and cost, over and beyond diagnosis and other covariates, suggests that the number of physical symptoms reported at intake may prove useful as a screening tool. Of course, screening high on physical symptoms requires further investigation and assessment, because physical symptoms appear to consist of several components, any one of which would require further scrutiny. Some of these components, mentioned earlier in the introduction, involve comorbid physical illness and side effects of psychotropic medications, both direct and indirect. In addition, recent studies have shown a predictive correlation between physical symptoms, multiple unexplained physical symptoms, and prevalence of negative affectivity (
21,
22), which cuts across specific diagnoses and is an indicator of illness severity.
The fact that a majority of patients in this study presented with a significant number of physical symptoms also suggests that a sizeable subgroup of persons with serious mental illness seeking mental health services have significant general medical comorbidities. Consistent with the literature, these general medical illnesses may be underdetected and undertreated or treated nonoptimally in the mental health setting in cases where a connection between the patient and a primary care provider is nonexistent. Behavioral health care settings are not the most cost-effective settings for the delivery of general health care services (for example, pain management), but persons with serious mental illness all too often rely on these services because they have limited access to more suitable services, such as primary care (
23).
Conclusions
Given these realities, we believe it remains critical to improve the care of comorbid medical illnesses for persons with serious mental illness and suggest that the assessment of physical symptoms at intake may also prove useful in this context.
In summary, we suggest that the self-reporting of physical symptoms on a structured questionnaire such as the PHQ-15, which provides a simple way for patients to provide pertinent health information in a behavioral health care setting, can serve as a practical and useful screening tool. Physical symptom levels may screen not only for comorbid physical illness and iatrogenic symptoms but may also help to gauge negative affectivity levels and illness severity. As such, the assessment of physical symptoms early in treatment can serve as a simple, feasible, and powerful predictor of service use and cost in behavioral health care and, as a consequence, aid in treatment and program planning.
Acknowledgments and disclosures
This work was partially supported by grant P20MH074634 from the National Institute of Mental Health.
The authors report no competing interests.