The increased risk of cardiovascular disease among people with severe mental illness is now well established (
1,
2). Explanations include lifestyle factors such as diet, smoking, and inactivity (
3), as well as the obesogenic and diabetogenic effects of second-generation antipsychotics (
4,
5). Greater vigilance in the management of cardiovascular risk factors has the potential to reduce rates of cardiovascular disease among members of this group of patients, helping to meet national targets of reducing deaths from cardiovascular disease by 40% among people under age 75 (
6) and to address inequalities in health care (
7–
13).
Individuals with severe mental illness experience excess mortality, in part due to unhealthy lifestyles (
14), but they are equally likely compared with the general population to take advantage of an offer of screening for risk factors for cardiovascular disease (
15). However, risk reduction interventions designed for and tested in trials among the wider population may need to be altered to be acceptable to those with severe mental illness if similar benefits are to be achieved (
16).
In England these concerns, and increasing recognition of the importance of a patient's choice (
17), have motivated the National Health Service to shift toward a shared-care model for the management of severe mental illness in which primary care services increasingly take responsibility for developing and delivering mental health services (
18–
21). Both primary and specialty mental health care are provided free by the National Health Service, centrally funded solely through taxation (
22), under its founding principles of universality and equity (
23).
Under the National Service Framework for Mental Health (
18) general practitioners (family doctors) are expected to conduct regular reviews of the general medical health of patients with severe mental illness. Contracts with general practitioners, formalized in the Quality and Outcomes Framework for primary care services (
24), contain financial incentives to check smoking status and blood pressure annually and to offer smoking cessation advice. An intended effect of these contractual arrangements was to improve coordination across the interface of primary and specialty mental health care (
25).
Specialty mental health care in England is commonly provided by local community mental health teams (CMHTs) accountable to National Health Service mental health trusts covering specific geographic sectors. The system was designed to increase primary care capacity by encouraging CMHTs to collaborate with general (primary care) practices located in the same sector, which, in turn, are accountable to local National Health Service primary care trusts. CMHTs follow the Care Programme Approach, comprising assessment of a patient's health and social needs in outpatient psychiatric clinics, formal care planning, allocation of a key worker to each patient, and regular reviews (
26). The system, in place for more than 20 years, has standardized psychiatric care nationally and reduced patient dropout (
27).
In 2009 the National Institute for Health and Clinical Excellence (NICE) issued evidence-based clinical guidelines for treatment of schizophrenia that addressed management of risk of cardiovascular disease (
28). In keeping with the shared-care model, the guidelines clearly recommend that primary health care professionals monitor the general medical health of people with schizophrenia at least once a year, particularly their risk of cardiovascular disease and management of risk factors. The guidelines direct them to communicate screening results to any CMHT involved in the individuals' care so that care planning can incorporate interventions to reduce health risks. For primary care practitioners, the guidelines identify psychiatric patients as a target screening group, and for specialty mental health care practitioners, they underline the importance of considering general medical health in care planning.
The latest NICE guidelines for the management of bipolar disorder also recommend annual general medical health checks by primary care providers but fail to specify who is responsible for reduction of risk (
29). A similar omission from an earlier set of schizophrenia guidelines (
30) resulted in reports by English psychiatric teams of uncertainty about respective responsibilities, limited access to basic equipment, and a lack of confidence in the interpretation of abnormal screening results (
31). These experiences, and studies of implementation of NICE guidelines, highlight the importance of developing guidelines that unambiguously delineate the clinical responsibilities of primary and specialty mental health care team members (
32).
Research also shows that staff support of recommended guidelines is a key determinant of implementation (
32). Surveys indicate that although there is consensus about the need for cardiovascular screening of this group, views diverge about whether responsibility should lie in primary or specialty mental health care, or indeed outside the National Health Service (
33,
34). Qualitative research shows that although staff favor assigning responsibility for screening of presence and management of risk factors for cardiovascular disease to primary care providers, patients prefer to be screened by a CMHT (
34). Studies on a wider scale are needed to explore how to reconcile staff and service users' views within the English model of shared care.
We undertook a survey of patients and staff in southern England to assess current practice and attitudes related to screening and reduction in risk factors for cardiovascular disease, preferences for service provision, and perceived barriers to service uptake.
Methods
Measures
Survey questionnaires were developed through a process of group discussion and piloting among health professionals, lay people, and service users. Separate versions were developed for primary care staff, CMHT staff, and service users. Questions for staff included whether they currently discussed cardiovascular disease risk factors with their patients with severe mental illness, whether they offered risk reduction interventions, how important they considered assessment of cardiovascular health, which services they were prepared to provide, how often they performed the screening and in what setting, how results were communicated, and whether they anticipated obstacles to implementation and if so, to name them.
Service users were asked about prior receipt of screening for and interventions to reduce risk of cardiovascular disease, views on the value of the screening, preferred setting and frequency of screening, and anticipated barriers to attendance. Views were assessed by using forced-choice response formats and Likert scales. Ethics approval was obtained from the North West Multi-Centre Research Ethics Committee. All National Health Service trusts involved gave their approval for participation, and sampling involved a process of individual informed consent.
Setting and participants
Geographical areas were chosen to balance urban and rural settings. Randomly generated numbers were used to select 100 primary care practices and 30 CMHTs from all National Health Service primary care trusts and mental health trusts in Avon (the West Country), North Central London, and North West London. In 2005 questionnaires were sent individually to staff of these organizations, comprising 353 general practitioners (family doctors), 100 practice nurses (primary care nurses), and 391 CMHT staff (including consultant psychiatrists, trainee psychiatrists, community psychiatric nurses, social workers, occupational therapists, psychologists, and team managers).
For ethical reasons, service user questionnaires were distributed to patients by CMHT care coordinators or staff at psychiatry outpatient clinics associated with 30 randomly selected CMHTs located in the same geographic areas in which staff surveys were distributed. However, given that the CMHTs distributing the service user questionnaires were identified by generating random numbers, they were not necessarily the same as the teams that participated in the staff survey.
Completed questionnaires from all three groups were returned in prepaid envelopes and responses were coded. Because questionnaires were completed anonymously, no reminders could be sent to nonresponders. Descriptive analyses were conducted using SPSS, version 14.0, for Windows.
Results
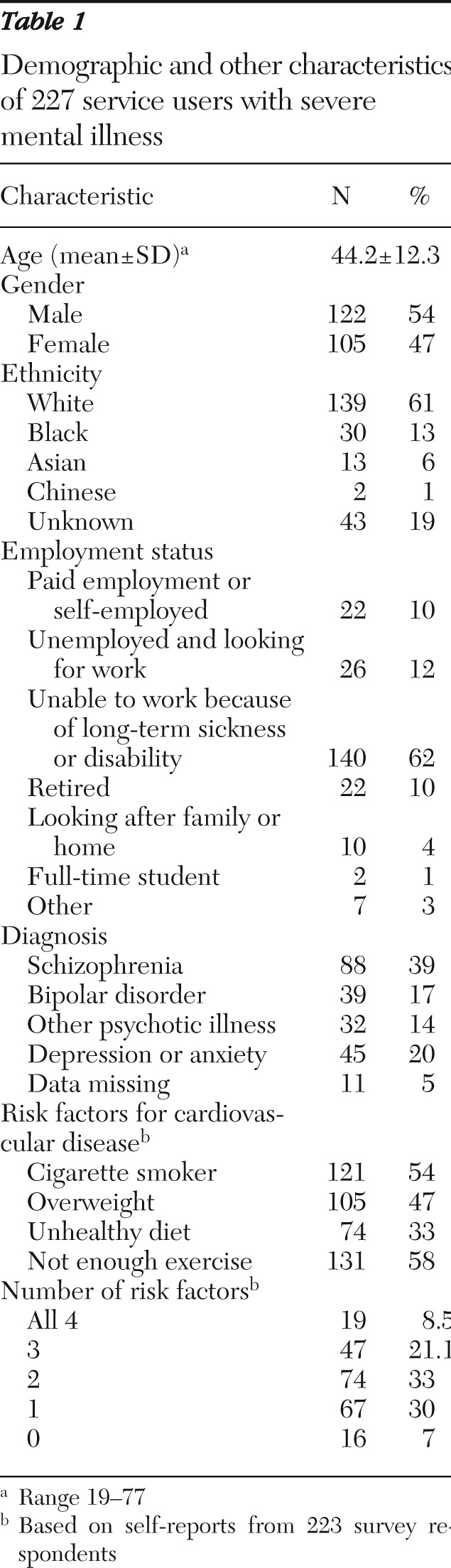
Surveys were distributed to 453 primary care staff and 391 staff of CMHTs (
Table 1). Responses were received by 143 (31%) primary care staff and 166 (42%) CMHT staff. Among the primary care staff, 106 (74%) were general practitioners and 36 (25%) were practice nurses. Their mean±SD age was 47.1±8.8 years (range 27–71), and they had been in practice for 12.8±9.7 years; 52 (36%) were men, 84 (59%) were women, and data about gender were unavailable for seven (5%).
Among the CMHT staff, 49 (30%) were community psychiatric nurses, 41 (25%) were social workers, 32 (19%) were psychiatrists (consultants and trainees), nine (5%) were occupational therapists, nine (5%) were psychologists, 12 (7%) were team managers or leaders, and 13 (8%) were other staff. Their mean age was 41.9±10.04 (range 25–63), and they had been in practice for 22.3±22.9 years; 64 (39%) were men, 99 (60%) were women, and data about gender were unavailable for three (2%).
Completed questionnaires were returned by 227 service users, but the number distributed to service users could not be ascertained reliably. Demographic and other characteristics of the respondents are shown in
Table 1.
Importance of cardiovascular screening
A majority of service users (N=202, 89%) agreed that routine provision of heart checks for people with mental health problems would be good policy, five (2%) disagreed, and 20 (9%) had no opinion.
Primary care and CMHT staff were asked to rate the importance of screening individuals with severe mental illness for cardiovascular disease compared with other work they undertake on behalf of these patients on a scale of 1 (not at all important) to 10 (very important). Among primary care staff, the median score was 7 (mean 6.8±2.0). The importance of cardiovascular screening among these patients received a median score of 8 (mean 7.05±1.93) when compared with the importance of screening other patients for cardiovascular disease.
CMHT staff rated the importance of screening for cardiovascular disease among patients with severe mental illness compared with their other work with these patients with a median score of 5 (mean 5.7±2.7). Asked whether these patients should be screened regularly for heart disease, 91 (55%) answered nearly always, 59 (36%) answered sometimes, and 11 (7%) answered never or rarely.
Current practices for cardiovascular screening
Staff were asked about the types of health promotion advice they usually offered, where appropriate. Among primary care staff, advice was usually offered about healthy eating (N=121, 85%), exercise (N=116, 81%), gym referral (N=23, 16%), weight reduction (N=113, 79%), and stopping smoking (N=133, 93%). Ten staff (7%) provided advice about other forms of help, three staff (2%) provided no advice about these forms of help, and data were missing for three staff (2%).
A total of 27 (19%) primary care staff reported that they nearly always discussed risk factors for cardiovascular disease with service users; 63 (44%) reported discussing them sometimes, and 50 (35%) rarely or never discussed them. Thirty-four (24%) staff reported nearly always screening for risk of cardiovascular disease; 75 (52%) reported screening sometimes, and 31 (22%) reported rarely or never screening. Data about discussion of and screening for risk factors were missing for three (2%) primary care staff.
Among CMHT staff, advice was usually offered about healthy eating (N=141, 85%), exercise (N=148, 89%), gym referral (N=125, 75%), weight reduction (N=125, 75%), and stopping smoking (N=115, 69%). Fourteen staff (8%) provided advice about other forms of help, eight staff (5%) provided no advice about these forms of help, and data were missing for three (2%) staff.
A total of 58 (35%) reported that they nearly always discussed risk factors of cardiovascular disease with service users; 60 (36%) sometimes discussed them, and 32 (19%) rarely or never discussed them. Thirty-one (19%) nearly always provided screening for cardiovascular disease risk; 25 (15%) provided screening sometimes, and 96 (58%) never provided screening. Data about discussion of and screening for risk factors were missing for 16 (10%) and 14 (8%) of CMHT staff, respectively.
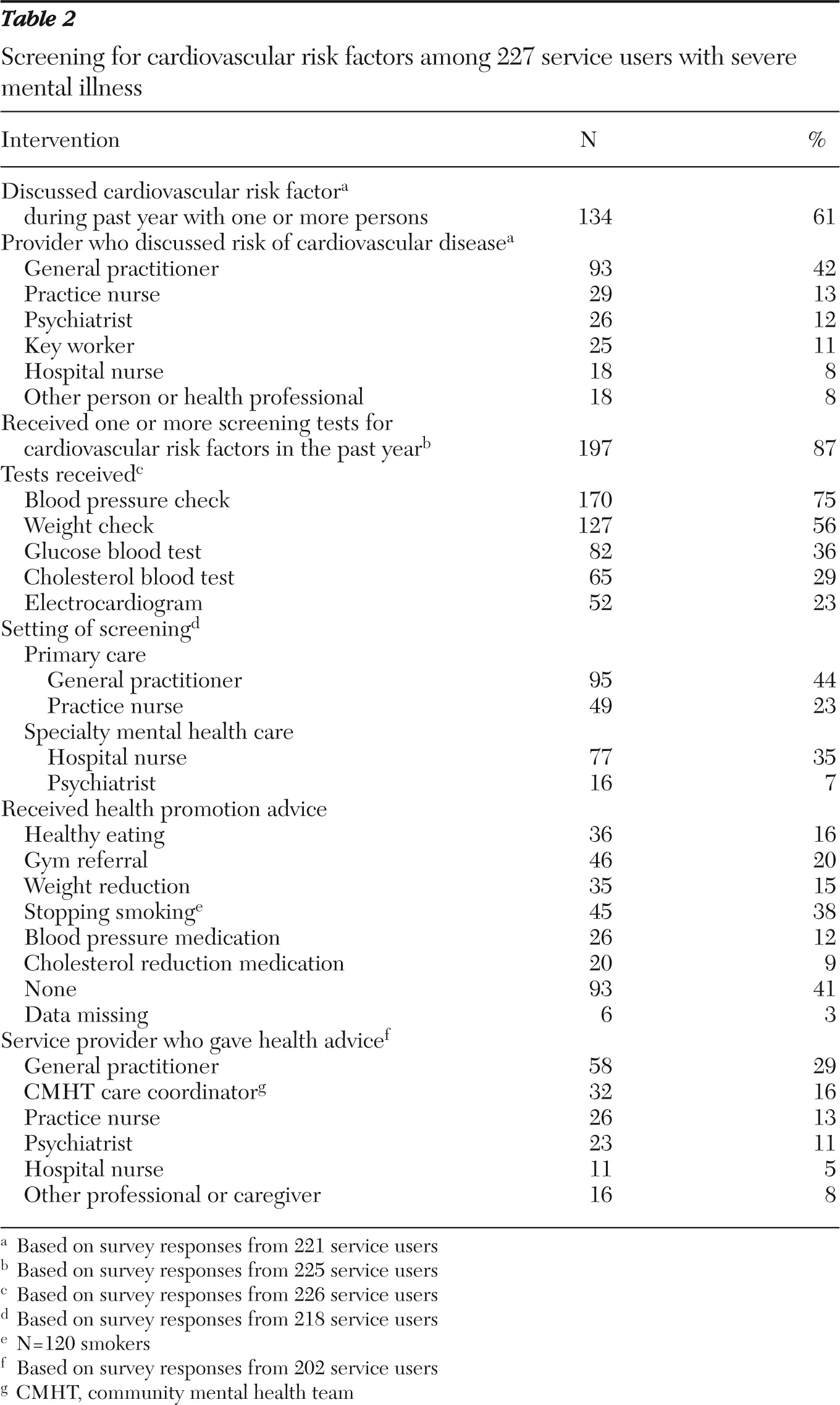
Table 2 summarizes service users' receipt of screening for cardiovascular disease and advice about health promotion or lifestyle interventions during the previous year. A majority of the 221 respondents (N=134, 60%) had discussed risk factors with one or more professional. Of 225 respondents, 197 (87%) had received one or more screening tests for cardiovascular disease during the previous year, predominantly in the course of primary care. Among 218 respondents, 95 (44%) were screened by a general practitioner and 49 (23%) by a primary care practice nurse.
Just under half of service users (41%) stated that they had received no health promotion advice during the previous year. Of 120 smokers that responded, 45 (38%) had received advice about quitting, and 28 (27%) of the 105 respondents who reported being overweight had been offered weight loss advice.
Acceptability and frequency of cardiovascular screening
A total of 173 (76%) service users indicated that they would arrange an appointment for screening for cardiovascular disease, and 186 (82%) said they would attend one.
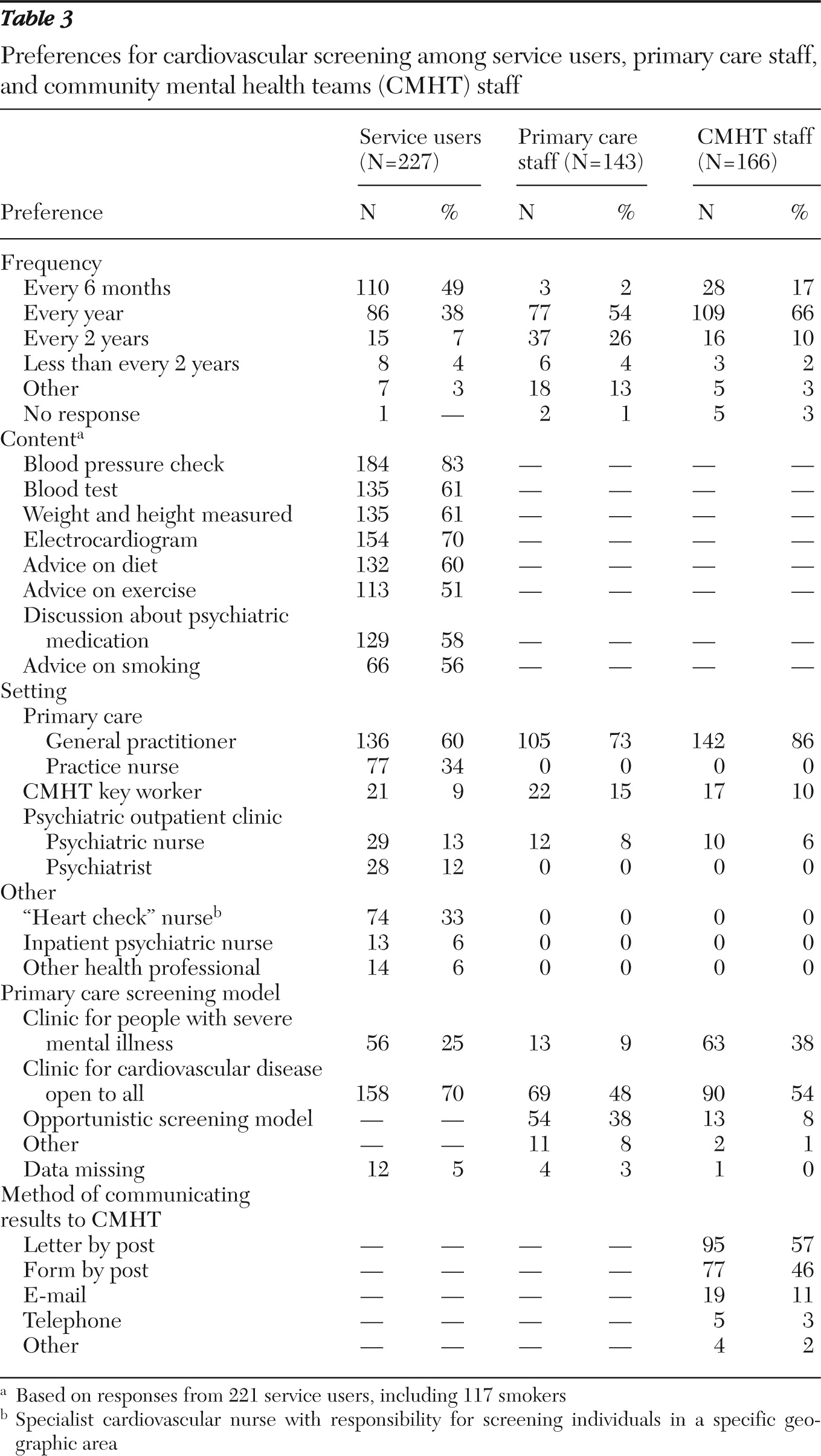
Table 3 indicates the components of screening and advice that they would be prepared to accept and their preferred frequency.
Both groups of service providers and service users preferred that cardiovascular screening occur at least annually. A majority (N=158, 70%) of service users preferred that screening take place in a primary care setting open to all rather than at a clinic exclusively for people with severe mental illness. A total of 111 (67%) of the 166 CMHT staff who responded wanted more involvement in the general medical health of their patients, but 142 (86%) of 166 respondents believed that primary care was the best setting for cardiovascular screening, as did 105 (73%) primary care staff.
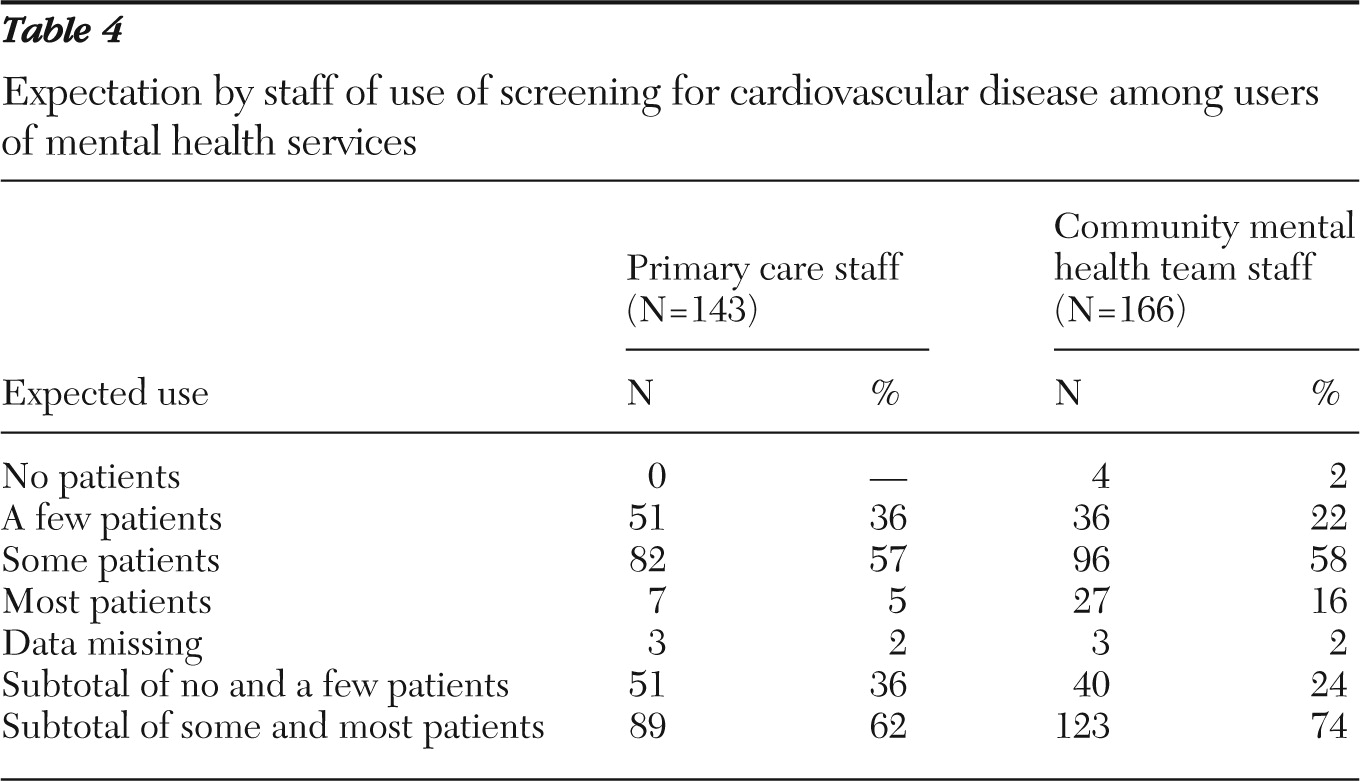
Both groups of staff anticipated good screening uptake (
Table 4). A minority (N=4, 2%) of CMHT staff expected that patients would not attend screening, but everyone else expected at least a few patients would participate.
Preferred interventions
Service users were asked about their preparedness to attempt a range of healthy lifestyle changes with the help of a nurse or doctor. Interest in risk reduction interventions appeared lower than levels of interest in screening. Of the 118 smokers who responded, 51 (43%) indicated that they were prepared to try to stop smoking by using tablets or nicotine patches. Of 104 overweight respondents, 66 (64%) were prepared to try eating a healthier diet, 73 (70%) were prepared to exercise more, and 84 (81%) were prepared to try losing weight. A total of 74 (33%) service users reported unhealthy diets, and 59 (80%) were prepared to attempt healthier options. Not getting enough exercise was reported by 131 (58%) service users, but 101 (78%) were prepared to exercise more.
Service users preferred to receive help with lifestyle changes at a primary care (general) practice (N=90, 40%), at the CMHT base (N=70, 31%), at a day hospital or day center (N=118, 52%), or other site, including a recreation center (N=15, 6%). They identified difficulty travelling (N=79, 35%), time pressures (N=63, 28%), a general dislike of courses or group work (N=51, 23%), and a concern that they might begin to worry too much about their health (N=30, 13%) as barriers to obtaining help with making lifestyle changes. Only four (2%) said that they did not care about the health of their heart.
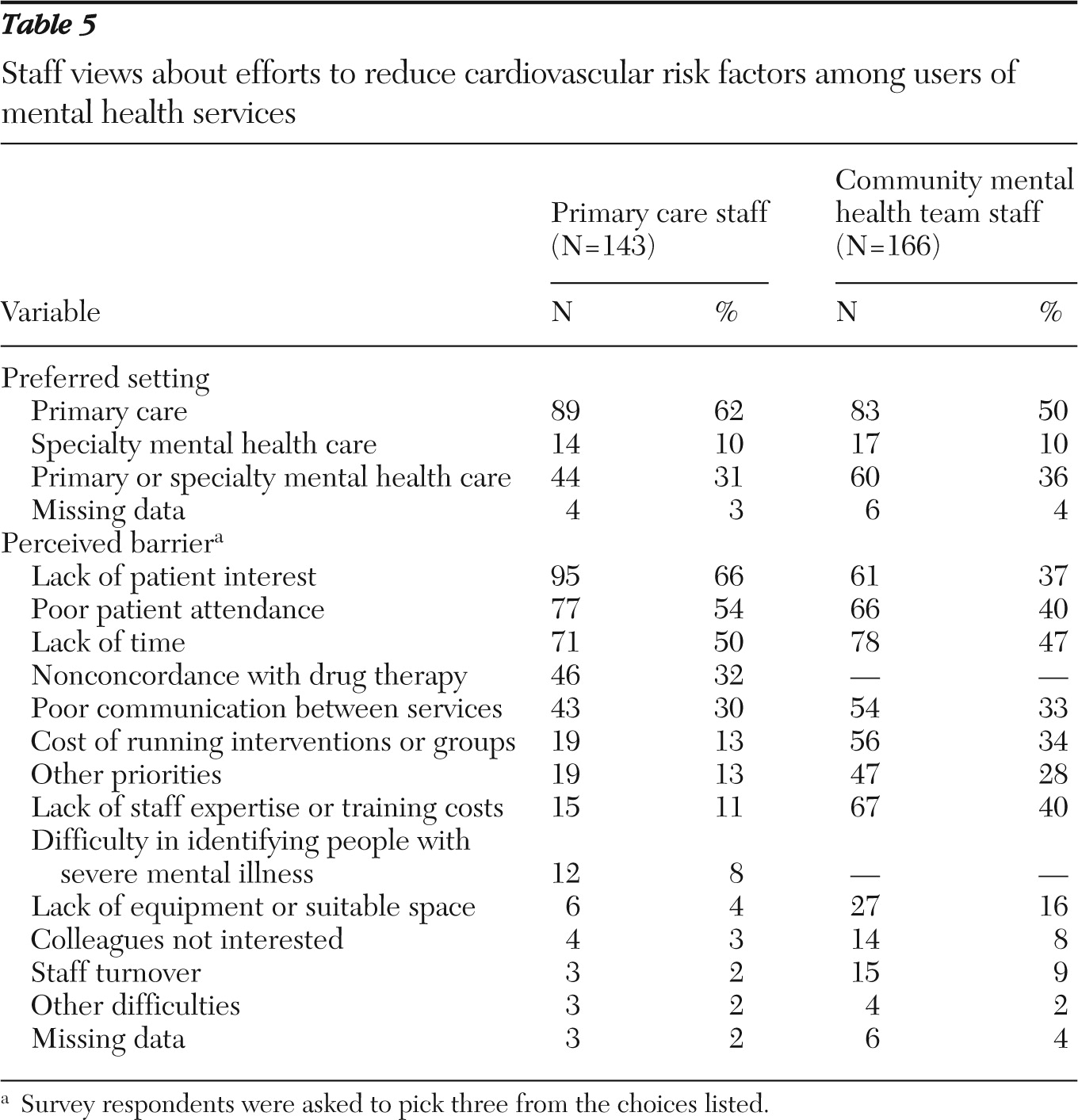
Both groups of staff expressed a preference for using primary care as the setting for risk reduction interventions for people with severe mental illness (
Table 5). Primary care staff tended to identify patient-related factors as barriers to implementation of interventions to address cardiovascular disease risk factors, whereas CMHT staff were more likely to blame staff-related factors.
Discussion
This survey of primary care staff, mental health staff, and service users with severe mental illness showed that all three groups placed value on cardiovascular health checks for people with severe mental illness. This finding replicated previous research demonstrating service users' high commitment to attending a cardiovascular disease screen (
15).
We found that CMHT staff reported more frequent discussion of risk factors for cardiovascular disease with service users than did primary care staff, but that primary care staff assessed risks of cardiovascular disease more routinely. High proportions of primary care and CMHT staff reported routine provision of lifestyle advice.
Although these findings appear encouraging, evidence from the United Kingdom, the United States, and Australia reveals suboptimal screening coverage for this patient group. Gaps in screening persist despite widespread awareness among stakeholders of its importance and recommendations for its use in evidence-based guidelines (
12,
35,
36). In our survey, more than one-third of service users had not discussed their risk of cardiovascular disease with a professional, and their estimates of the provision of cardiovascular risk reduction interventions fell short of staff estimates. This finding points to the importance of understanding supply-side and demand-side barriers to integrated mental health care in England in order to identify acceptable means of addressing them (
37).
Agreement about the respective roles and responsibilities of primary and specialty mental health care staff is an important determinant of willingness to supply or utilize a service, primarily because it confirms acceptability. For staff it reduces replications, omissions, and professional disputes, and for psychiatric patients it identifies the least stigmatizing model (
38). This survey showed general agreement that screening and reduction of risk of cardiovascular disease should be provided as part of primary care, in contradiction of previous qualitative research showing that patients favored a CMHT setting (
34). Provision of these services by primary care staff appeared to be the norm in this sample, but respondents' views about obstacles to uptake suggested explanations for the evident gaps in coverage. The barriers identified also indicate where further research is needed to identify incentives for achieving reduction of cardiovascular disease risk within a shared-care model.
Service users in this survey displayed a marked mismatch between their level of interest in screening for risk factors for cardiovascular disease and their preparedness to engage in interventions to reduce risk. Difficulty adopting healthy behaviors despite good intentions is a public health challenge for the wider population (
39,
40), but mass marketing material to promote healthy choices (
41) may not be suitable for people with severe mental illness. Evidence suggests that educational programs for these patients should incorporate repetition and individual or group discussions with a key worker to reinforce messages about the likely benefits of risk reduction interventions (
11). Such strategies would be deliverable through the Care Programme Approach, as discussed below.
In this sample, individuals' readiness to change modifiable cardiovascular risk was governed by factors such as travel, time, and an aversion to structured interventions. Their preference for receiving screening at generic primary care screening clinics rather than at clinics specifically targeted toward psychiatric patients highlighted the value they placed on minimizing stigma. Further qualitative research would help investigate specific factors that contribute to the apparent reluctance among individuals with severe mental illness to participate in risk reduction work. Factors to explore, which are likely to vary among ethnic groups, include the appropriateness of the format and language used in current interventions; the adequacy of incentives; self-perceptions of risk (
42); and expectations about the pace of behavior change. The results of this research could be used to adapt interventions found to be successful in the general population to the needs of people with severe mental illness, just as adaptations are made for any other subgroup at risk of cardiovascular disease (
43). Intervention studies, including trials of the contingency management approach (
44), would quantify the impact of incentives on outcomes such as service uptake and cardiovascular health.
Incentives are also important when considering supply-side barriers to implementation, particularly if guidelines confer additional workload on primary care staff or CMHTs (
12). Although in England, the Quality and Outcomes Framework already contains financial incentives to address most aspects of screening for risk of cardiovascular disease (
24), the opportunity exists to expand screening in the future by adding lipid checks and addressing risk factors such as smoking and obesity. Our findings indicated that specialty mental health care staff may be willing to assist in providing screening and motivating service users to attend screening and adopt lifestyle changes. As noted, 70% of CMHT staff wanted more involvement in the general medical health of these patients.
CMHT staff also held more optimistic views than primary care staff about service users' engagement in risk reduction. Under existing Care Programme Approach arrangements, CMHT staff in regular contact with clients are well placed to review the monitoring information provided by primary care providers and encourage patients to address risk factors. Approaches might include motivational enhancement (
45) and exercise groups promoting social connectedness (
46). The advantages of such work include reduction of cardiovascular risk, increased social engagement, enhanced social capital, reduced stigma, improved mental health, and better social functioning.
Finally, clinical audit has been shown to improve screening provision for psychiatric patients by facilitating organizational change (
47). The detailed approach of audit, with its emphasis on what is feasible locally, allows for local views to be factored into service provision, and practice suggests that it may be an acceptable way for local teams to adopt NICE clinical guidelines on mental health (
48).
The study had strengths and limitations. The main strengths of the study were the random selection of primary care practices and CMHTs and the anonymous nature of the responses, which enhanced disclosure of the views of relevant stakeholders in rural and urban areas. It addressed current practice and preferred models of care, including a realistic consideration of the components of any screening and risk reduction program, and the providers best suited to offer them. It has direct relevance to implementation of current policy.
Response rates of between 31% and 42% for staff were to be expected for a survey of this kind, but the method did not allow for determination of a response rate among service users because the number of surveys that were distributed could not be tallied. A response bias is possible—for example, among service users motivated to improve health care services, staff who recognized a need to improve in this area, or staff concerned that service changes might increase workload. Respondents may also have been influenced by a desire for social acceptability, leading them to overestimate the degrees of preparedness to provide or engage in screening and risk reduction activities. These biases could limit generalizability. Although the results reported here are related to the NICE schizophrenia and bipolar guidelines, respondents included service users who had diagnoses of schizoaffective, depressive, and anxiety disorders. The data did not include objective measures of the severity of mental illness or of cardiovascular risk.
Conclusions
These results suggest that in England risk of cardiovascular disease among individuals with severe mental illness is managed mainly in primary care but that coverage is incomplete. The views of staff and service users indicated broad support for this service arrangement. However, the barriers to uptake they perceived indicated how such gaps might be addressed. For example, service users' attitudes suggested that research into incentive structures for persons with severe mental illness within different ethnic groups could be used to help design services that are more likely to achieve screening and risk reduction targets. Staff attitudes indicated that there may be capacity for psychiatric professionals to support primary health teams in this work as part of the Care Programme Approach.
Acknowledgments and disclosures
This research was supported by Medical Research Council trial platform grant G0301032. The authors thank all staff and service users who took part in the research, the CMHT staff who helped with service user recruitment, and the National Health Service mental health trusts and primary care trusts for their agreement to participate. [A complete list of participating trusts is available in an online appendix to this report at
ps.psychiatryonline.org.] They also thank Elaine Wong, R.G.N., who coordinated distribution of service user questionnaires, at clinics and by CMHT staff, and who coded survey responses.
The authors report no competing interests.