Access to care from mental health providers has been judged unsatisfactory in many countries where adequacy of treatment, in particular for depression and anxiety disorders, has been reported as inadequate (
1–
4). Changes in public mental health services that target unmet needs for treatment and seek to provide more appropriate and more effective treatments and services have been under way in the United Kingdom since 2007 and in Australia since 2006 (
5–
7). These measures aim to improve access to psychological treatment by training more psychologists to provide psychotherapy and by ensuring financial coverage for psychological treatment of patients referred by general practitioners and psychiatrists. Such measures are expected to change the roles of psychiatrists and nonpsychiatrist mental health providers.
Data from the European Study of the Epidemiology of Mental Disorders (ESEMeD) indicated that in all the countries participating in the survey, general practitioners were the most frequently consulted professionals by persons with mental health problems (
8). The study found considerable differences in use of mental health services provided by nonpsychiatrist mental health professionals (psychologists, psychotherapists, counselors, and social workers) and by psychiatrists. These differences were attributable to the respective roles and training of the two groups and to reimbursement policies and gatekeeping arrangements (
8).
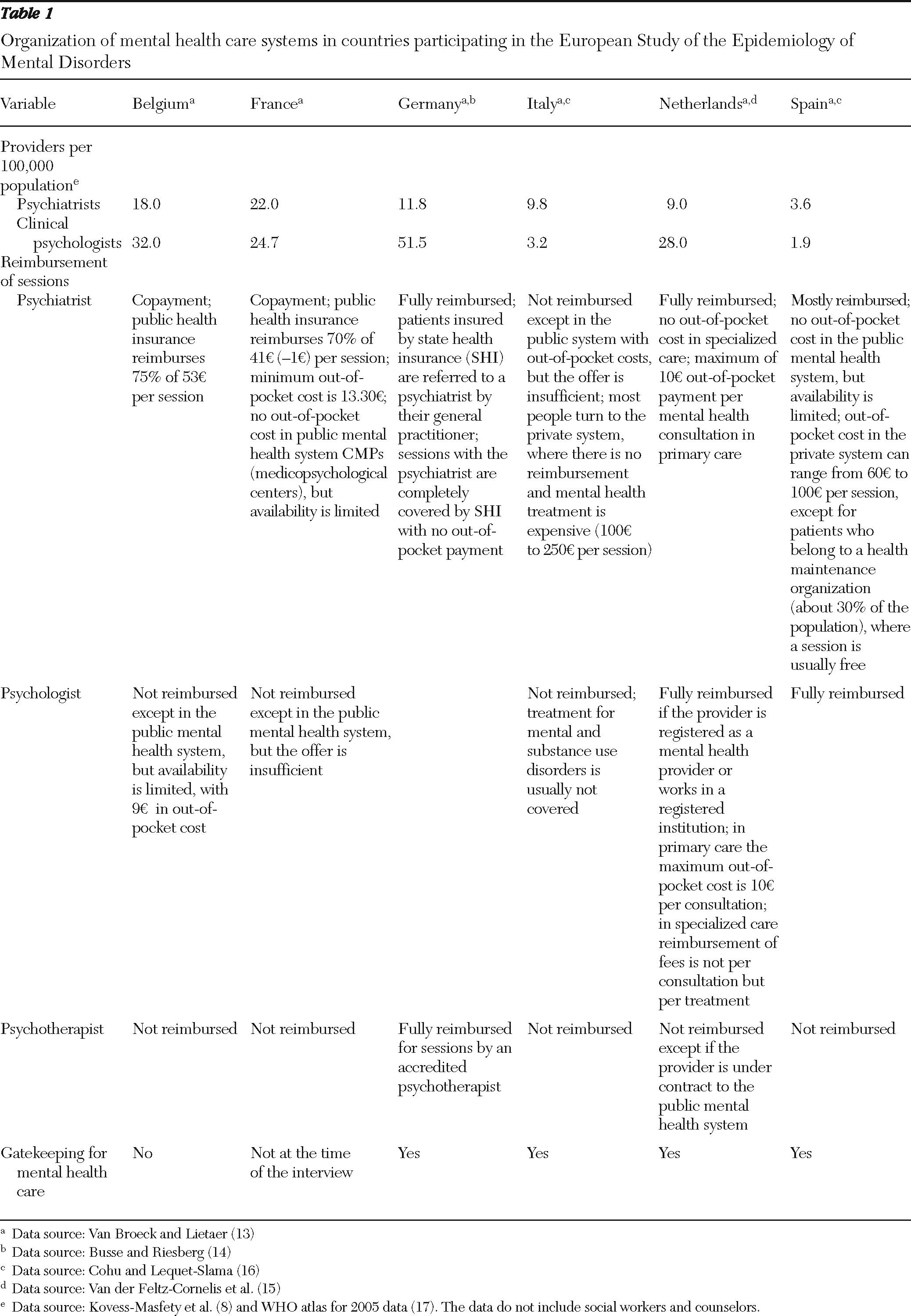
Use of mental health services provided by a psychiatrist or by a nonpsychiatrist professional depends on many factors. National policies affect the population density of professionals per capita, the availability of practitioners, and the level of out-of-pocket costs. In addition, the presence or absence of gatekeeping arrangements has an effect on the type of provider consulted (
1,
4,
8–
13). For example, in Germany, the Netherlands, and Spain, sessions with psychiatrists and psychologists are fully or largely reimbursed by public and private health insurance. In France and Belgium, patients pay moderate out-of-pocket costs for consultations with psychiatrists. In Italy, consultations with psychiatrists are expensive and generally not reimbursed. In Italy, France, and Belgium, sessions with psychologists are not reimbursed. At the time of the ESEMeD survey (2001–2003), only France and Belgium did not have gatekeepers in their mental health system (
14–
17).
Table 1 summarizes information about the organization of mental health care systems in ESEMeD countries.
The type of provider consulted also depends on sociodemographic, clinical, and cultural factors; the degree of stigmatization; and mental health literacy (
1,
18–
23). For example, some studies have indicated that males are more likely to use services provided by psychiatrists than by nonpsychiatrists (
18,
19). Individuals with mood disorders and those with the most severe disorders more often consult psychiatrists than nonpsychiatrist professionals (
21,
23).
In Europe little is known about use of mental health providers, particularly nonpsychiatrist mental health professionals, especially in regard to reimbursement rates and frequency and duration of sessions. Moreover, the mental health provider category is generally studied without distinction between psychiatrists and nonpsychiatrist professionals (
1,
24,
25). In addition, little information is available about the relationship between psychotropic drug consumption and use of mental health providers in Europe (
3,
26).
From the perspective of mental health system planning, the roles assigned to these professionals are of utmost importance, because psychiatrists are less numerous than nonpsychiatrist mental health providers and their longer medical training is more costly. Because psychiatrists are physicians able to prescribe, they generally treat individuals with the most severe disorders or those requiring psychotropic medication, and nonpsychiatrist providers are expected to deal with the remaining patients. In addition, in systems that provide better reimbursement for visits to psychiatrists than to nonpsychiatrist providers, the characteristics of patients who use the respective providers may differ from what would be expected on the basis of clinical criteria.
In a context of increased demand on mental health systems and restricted resources, a comparison of patterns of use of service provided by psychiatrists and nonpsychiatrist professionals seems worthwhile, as does the exploration of general practitioners' role in referral. ESEMeD data enabled such an investigation because the survey collected information on clinical and social factors and on service use in participating countries, where certain features of mental health systems vary.
The purpose of this study was to describe patterns of use of mental health providers—psychiatrists and nonpsychiatrist mental health professionals—in six European countries. First, sociodemographic and clinical factors and psychotropic drug consumption associated with use of each type of provider were identified. Second, the study analyzed the influence of national mental health policies (practitioner availability, practice characteristics, gatekeeping arrangements, and reimbursement systems) on use of provider type.
Methods
Samples and data collected
Data were from ESEMeD, which is a part of the World Health Organization World Mental Health Survey Initiative (
27). ESEMeD was a cross-sectional survey of the noninstitutionalized, general adult population of Belgium, France, Germany, Italy, the Netherlands, and Spain. Face-to-face, computer-assisted interviews were conducted between 2001 and 2003 with the Composite International Diagnostic Interview (CIDI), version 3 (
28). A stratified, multistage, clustered-area, probability sample design was used. A total of 21,425 individuals were interviewed. The overall response rate in the six countries was 61.2% (from 45.9% in France to 78.6% in Spain). A two-phase interview procedure was used. In the first phase, all respondents were screened for the most common mood and anxiety disorders. Those who reported symptoms of specific mood and anxiety disorders and a random sample of 25% of those who did not underwent the second phase of the interview. In the study reported here, data from the second phase were used, which included 8,796 individuals. A detailed description of methods is provided elsewhere (
29,
30).
Mental disorders
The CIDI was used to assess the presence of mental disorders according to
DSM-IV definitions and criteria (
31). Moderate to good agreement between the CIDI, version 3, and clinical diagnoses based on the Structured Clinical Interview for DSM-IV (SCID) has been demonstrated (
32). The disorders considered in this study were mood disorders (major depressive episode and dysthymia), anxiety disorders (social phobia, specific phobia, generalized anxiety disorder, agoraphobia with or without panic disorder, panic disorder, and posttraumatic stress disorder) and alcohol abuse or dependence.
Severity
Mental disorders identified by the CIDI were classified into three severity groups—severe, moderate, and mild. Disorders with highest severity level were alcohol dependence with a physiological dependence syndrome; suicide attempt in conjunction with any other disorder; and severe role impairment as the result of a mental disorder in at least two areas of functioning, as measured by a score of 8 or higher on disorder-specific Sheehan Disability Scales (SDS) (
33). Disorders were classified as moderate if the respondent had alcohol dependence or at least moderate interference in conjunction with any other disorder in any SDS domain (a score between 4 and 7 out of a possible score of 10). All other disorders were classified as mild (
1).
Service use
In the interview sections on use of services and for each mental disorder diagnosis, all participants were asked about their use of services for mental health problems during their lifetime and in the past year. The lists of providers include psychiatrists and “other mental health professionals,” such as psychologists, psychotherapists, social workers, and counselors. Self-reported information on the frequency and duration of sessions with mental health providers was collected for the previous 12 months. Respondents who reported use were asked whether their physician referred them to these providers.
Psychotropic drug use
ESEMeD methods used to document psychotropic drug use have been described previously (
24,
34). All respondents were asked about use of any psychotropic medication in the previous 12 months. To minimize possible recall bias and help respondents recall their drug use, a standard booklet with high-quality illustrations of psychotropic medications was provided. We report use of the main psychotropic drug classes.
Statistical analysis
The proportion of individuals who used the services of mental health providers was expressed in absolute numbers and percentages with 95% confidence intervals (CIs). Individual data were weighted to account for the different probabilities of selection and to restore age and gender distribution of the population within each country and the relative size of the population across countries (
34). Multiple logistic regression analysis identified factors associated with use of psychiatrists and nonpsychiatrist professionals; factors included sociodemographic characteristics (gender, age, country of residence, marital status, employment status, income, urbanicity, and level of education) and clinical characteristics (mood disorder, anxiety disorder, and alcohol abuse). Associations were expressed as odds ratios (ORs) with their CIs and tested for statistical significance with the chi square test. Use of providers was studied for a 12-month period to ensure that use and sociodemographic and clinical factors, psychotropic medication consumption, and levels of practitioner availability during the same time period. Because it provided better statistical power, lifetime use was analyzed to study the evolution of use of mental health providers and to determine the impact of clinical factors. All analyses were performed with Stata SE11 software.
Results
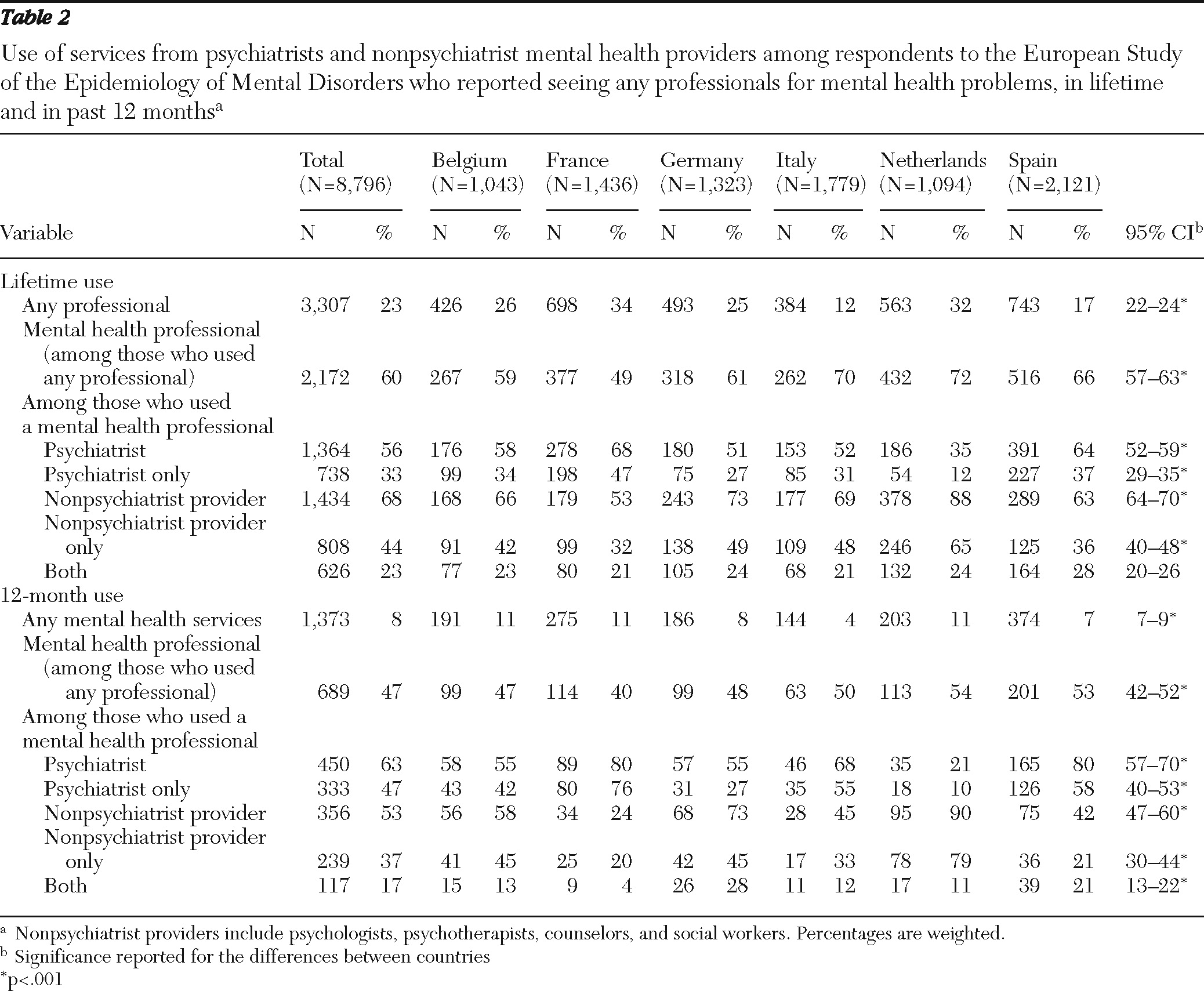
As shown in
Table 2, 23% of the 8,796 respondents used some type of service for a mental health problem during their lifetime (weighted percentages are reported). Among these users of any services, 60% consulted mental health care providers. Among these, 56% reported use of services from psychiatrists and 68% reported use of services from nonpsychiatrist mental health professionals, and 23% reported use of services from both provider types. Use of mental health providers in the previous 12 months was reported by 47%. Of these, 63% visited psychiatrists, and 53% visited nonpsychiatrist providers; 17% reported used of services from both provider types. It is noteworthy that lifetime and 12-month use differed by the type of provider; use of psychiatrists was more frequently reported in the more recent period. No differences in sociodemographic or clinical characteristics were found between those who used both types of professionals in the previous 12 months and those who used only one.
Distribution by country
As shown in
Table 2, use of mental health providers varied considerably between countries. Higher rates of use of psychiatrists were found in France (lifetime, 68%; 12-month, 80%) and Spain (64% and 80%, respectively), whereas lower rates were found in the Netherlands (35% and 21%). Higher rates of use of nonpsychiatrist providers were found in the Netherlands (88% and 90%) and to a lesser extent in Germany (73% and 73%). Rates of use of nonpsychiatrist providers were much lower in France (53% and 24%).
Sociodemographic and clinical factors
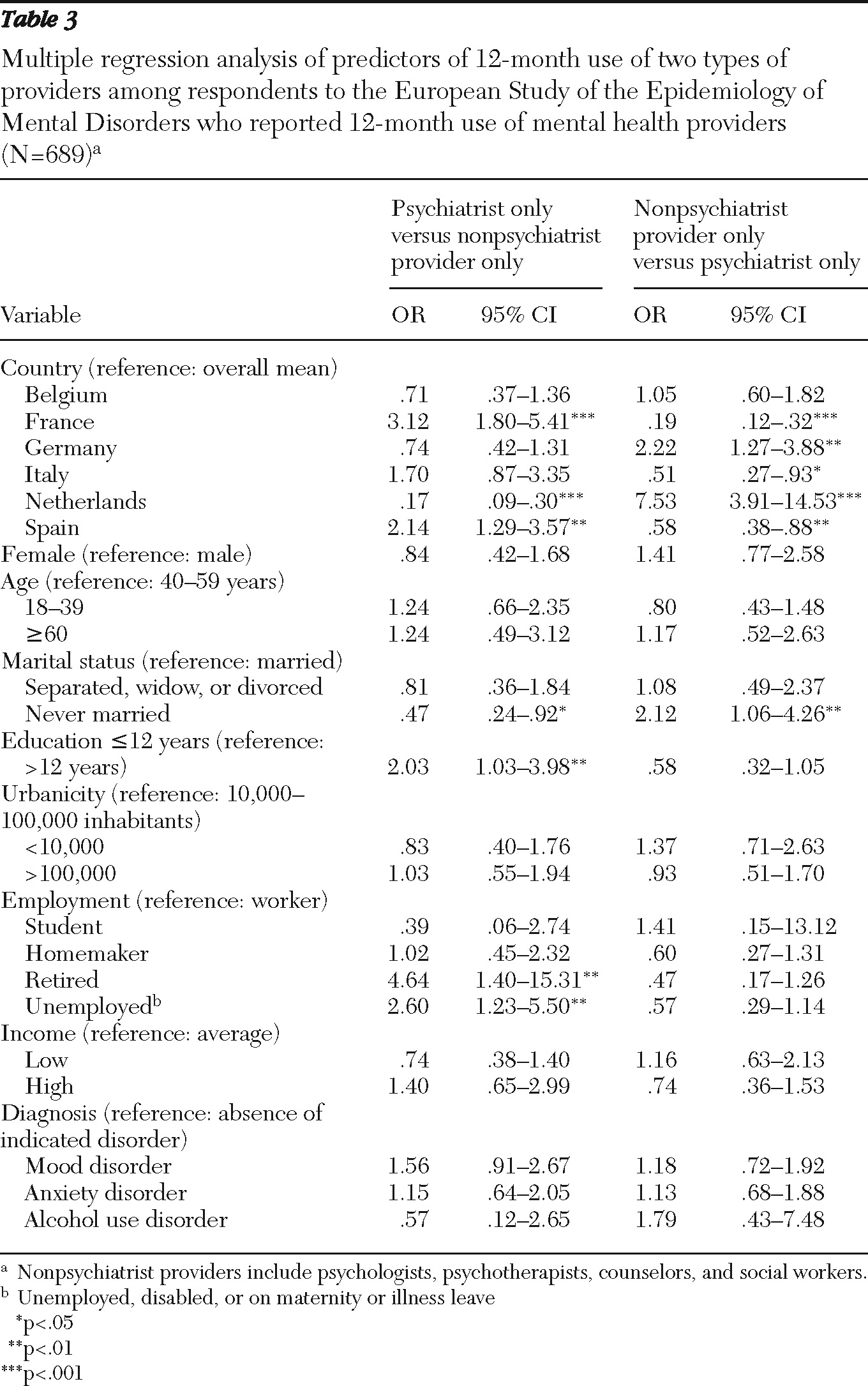
Table 3 presents the results of multiple logistic regression analyses, adjusted for sociodemographic and clinical factors. The analyses showed that respondents who were retired (OR=4.6) or unemployed (OR=2.6), who lived in France (OR=3.1) or Spain (OR=2.1), and who had 12 years or less of education (OR=2.0) were more likely to have sought help from a psychiatrist than from a nonpsychiatrist provider only, whereas those living in the Netherlands (OR=.2) and those who had never married (OR=.5) were less likely to have used a psychiatrist only.
A similar analysis of variables associated with lifetime use of psychiatrists or with nonpsychiatrist providers only showed that respondents with a lifetime mood disorder were more likely to have consulted psychiatrists (OR=2.5, CI=1.9–3.4; p<.001) than nonpsychiatrist providers only (OR=.7, CI=.5–1.0; p=.05), whereas participants with a lifetime anxiety disorder were more likely to use nonpsychiatrist providers than psychiatrists only (OR=1.8, CI=1.3–2.5; p<.001).
Regression analyses that adjusted for country, gender, and age indicated that patients who had 12-month disorders with the highest level of severity were more than three times as likely to have consulted psychiatrists than nonpsychiatrist providers only (OR=2.8, CI=1.4–5.8, p<.001).
Another analysis that adjusted for country, gender, and age, revealed that respondents who used psychotropic medication were more than five times more likely to have consulted psychiatrists only than nonpsychiatrist providers only (OR=5.5, CI=3.0–10.0 p<.001).
Finally, multiple logistic regression stratified by country and adjusted for gender and age showed that respondents who consulted psychiatrists only were more likely to use psychotropic drugs in Spain (OR=2.8, CI=1.1–7.2, p=.03) than in Germany (OR=.37, CI=.2–.7, p<.01). Among respondents who consulted nonpsychiatrist providers only, people living in France were the most likely to use psychotropic drugs (OR=2.6, CI=1.1–6.6, p<.05).
Practitioner-population ratios and system characteristics
As shown in
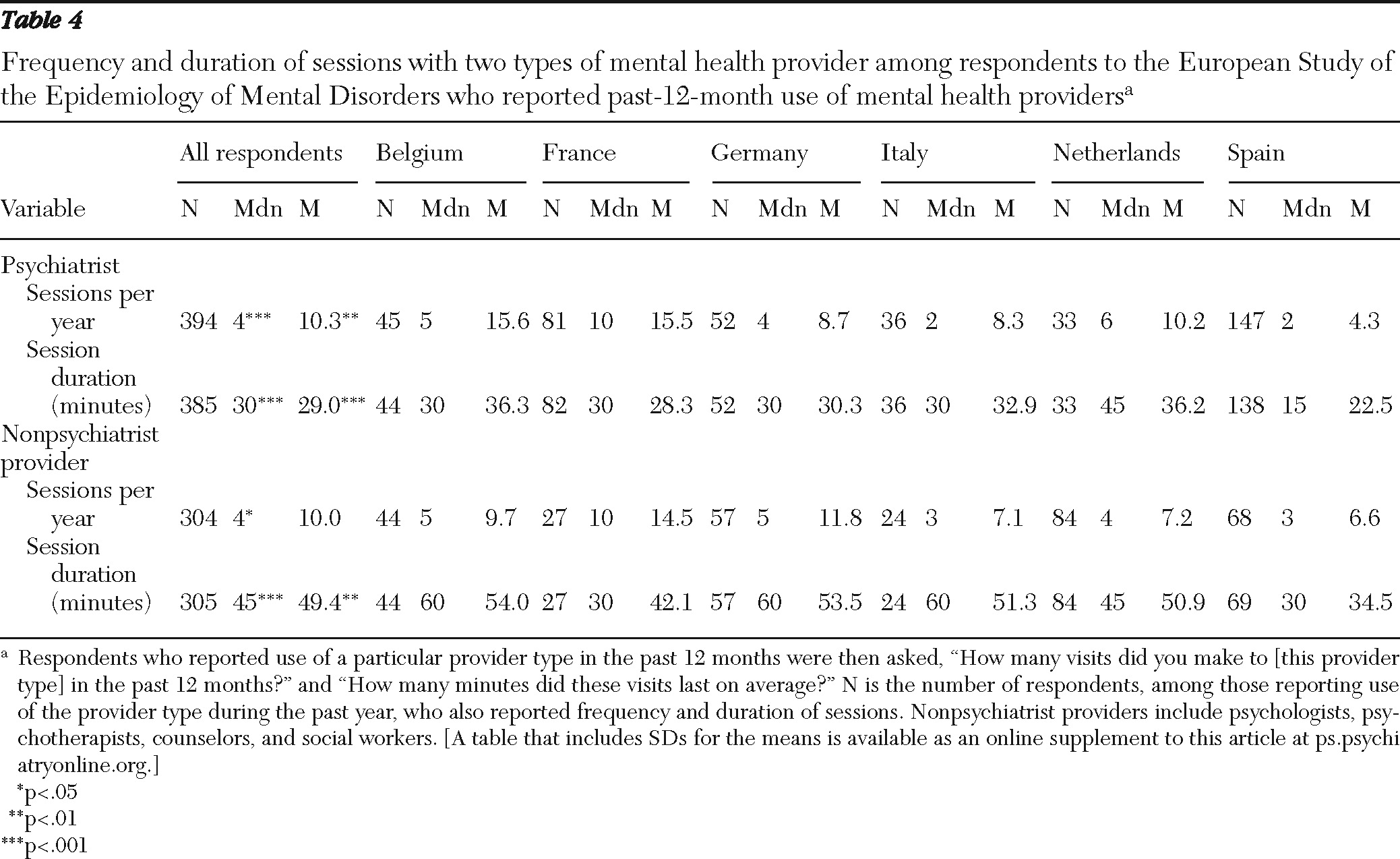
Table 4, among respondents who reported use of services from psychiatrists or from nonpsychiatrist providers in the past 12 months, the overall median frequency of sessions with psychiatrists was four per year, with a median duration of 30 minutes, and the overall median frequency of sessions with nonpsychiatrists providers was four per year, with a median duration of 45 minutes.
However, large differences were found between countries (
Table 4). These differences, combined with the differences in practitioner-population ratios (
Table 1), indicate different levels of availability of psychiatrists and clinical psychologists. For example, France has a high practitioner-population ratio (22 psychiatrists per 100,000 inhabitants [
Table 1]), but because the pattern of practice is based on numerous sessions per patient, practitioner availability is reduced. In contrast, in Spain, where the ratio is low (3.6 psychiatrists per 100,000 inhabitants [
Table 1]) but where the pattern of practice involves fewer sessions, availability is increased. This means that the density of mental health providers as measured by population ratios is not a straightforward indication of availability and should be adjusted on the basis of practice patterns.
Physician referral to mental health providers
Respondents who were referred to a mental health provider by a physician were about twice as likely to consult only psychiatrists compared with only nonpsychiatrist providers (OR=1.8, CI=1.2–2.3, p<.001, N=1,501), especially in France (OR=6.7, CI=2.7–17.1, p<.001), Belgium (OR=3.8, CI=1.4–10.3, p<.01), and Spain (OR=2.2, CI=1.1–4.7, p<.05), as indicated by a multiple logistic regression analysis stratified by country and adjusted for gender and age.
Discussion
The results of this study should be interpreted within the context of certain limitations. First, self-report of past events, particularly lifetime events, is particularly prone to recall bias. Second, use of psychologists could not be distinguished from use of other nonpsychiatrist mental health providers because the questionnaire grouped psychologists in a single category with psychotherapists, counselors, and social workers. Third, our analyses did not control for reimbursement and intracountry availability of the providers studied. Fourth, frequency and duration of sessions were self-reported by a small subsample of respondents, with large variations between countries. Therefore, measures of the effects of availability and mental health policy on use of mental health providers require refinement.
Despite these limitations, our results confirm that rates of consultation of psychiatrists and nonpsychiatrist mental health providers varied significantly across ESEMeD countries and that patterns of use were influenced by sociodemographic and clinical factors and health care system characteristics.
Age was not found to influence use of either type of practitioner. However, retired people were more likely than other groups to use psychiatrists, as reported in previous studies of elderly persons (
35), and students tended to use only nonpsychiatrist providers, as noted in previous studies of young people (
36).
Access to specialized mental health care has been found to increase with economic and educational status (
1,
18,
36–
38). However, it should be noted that level of income does not play the main role in Europe (
37).
Our study showed that among ESEMeD respondents who used mental health providers, those with mood disorders were more often treated by psychiatrists, which has been found in studies in North America (
9,
21,
38). Our findings suggest that patients with anxiety were more likely to consult nonpsychiatrist mental health providers. Studies have found that in both Europe and the United States, patients with severe disorders are more likely to use psychiatrists (
1,
23). Our multiple logistic regressions did not find an association between having an alcohol use disorder and using mental health services. Similarly, other studies have shown that individuals with alcohol- and drug-related disorders were the least likely to use mental health services (
8,
26,
37).
The literature shows a constant rise over the past three decades in the use of mental health providers, especially psychiatrists. In some countries, such as the United Kingdom, the increase might be attributable to the role of general practitioners as gatekeepers for specialty care; they are more likely to refer patients to psychiatrists than to other mental health professionals (
39). Health care professionals are increasingly aware of mental disorders, and consumer demand for specialty care has been stimulated by their awareness of programs for screening and access to care (
12,
19,
38).
Moreover, as studies in the United States have shown (
23,
40,
41), our study seems to show a relative increase across ESEMeD countries in treatment by psychiatrists and a relative decrease in treatment by nonpsychiatrist mental health professionals, especially in France, Spain, and Italy, as indicated by comparisons of lifetime and 12-month reports. However, these results should be interpreted with caution because a recent French study (
42) revealed that in the Paris area, where the density of psychiatrists is highest, seeing psychologists for depression increased over the past two decades while seeing psychiatrists has remained stable.
Use of various mental health providers is influenced by mental health policies (density of professionals, effective availability of those professionals, reimbursement policies, and referral practices) (
1,
4,
8,
18). Our results support the notion that effective availability may be a more important factor than density of professionals. The countries where the mental health providers were the most accessed, the Netherlands and Italy, did not have the highest density of mental health providers. On the contrary, in France, where mental health providers were the least accessed, the density is highest. Our results also suggest that fully reimbursing sessions with psychiatrists (as in Germany and the Netherlands), compared with requiring a moderate out-of-pocket outlay from patients (as in France, Belgium, and Spain) or a high out-of-pocket outlay as in Italy, does not necessarily increase rates of use. In contrast, in countries that do not reimburse for sessions with nonpsychiatrist mental health providers (France, Belgium, and Italy), use of those providers was lower than average, especially in France.
In addition, in some countries, such as France and Belgium, consultations with nonpsychiatrist mental health providers involved higher out-of-pocket costs than treatment by psychiatrists, and our results highlighted the effectiveness of this incentive.
Use of psychiatrists was higher in ESEMeD countries without gatekeeping systems (France and Belgium) and also when respondents were referred by a physician to a psychiatrist (France, Belgium, and Spain). However, a high level of reimbursement combined with gatekeeping (Germany and Spain) did not seem to lead to much more use, especially in Spain. Persons who were referred by a physician to a nonpsychiatrist provider were more likely to consult this type of professional (as in the Netherlands) than those who were not referred to this type of professional (as in France and Spain).
Conclusions
Our study suggests that there is no simple model of associations between characteristics of mental health care systems and patterns of service use and, ultimately, to best-practice access to care for most of the population. Cultural and socioclinical factors, such as interest in various types of therapy, as well as some aspects of national mental health policies, such as the practitioner-population ratio, effective practitioner availability of psychiatrists and nonpsychiatrists, a gatekeeping system, and reimbursement policies, affected patterns of use of each mental health provider. These comparisons highlighted the role of the organization of the care system in providing optimal access to adequate care for common mental disorders by giving a distinct role to each type of mental health provider and by coordinating access to them in terms of workforce availability and financial support.
Recent measures related to recommendations developed by the United Kingdom and Australia to improve adequacy of treatment and access to care for persons with anxiety and depressive disorders (
5–
7) could be taken as a model in some of the ESEMeD countries, especially in France and Belgium, which do not reimburse sessions with psychologists, as well in Spain, where, as in France, general practitioners' scores are low for adequacy of treatment of depression and anxiety disorders (
3,
4). To follow international practice guidelines (
43,
44), several measures should be implemented in the ESEMeD countries as required: use primary care physicians as gatekeepers; as suggested in a recent French report (
45), provide better training of general practitioners in the treatment of anxiety and depression; reimburse visits to psychologists up to eight sessions per year, in line with recommendations of professional organizations (
43,
44); and restrict psychiatrist consultation to the most severe and complex cases, using psychiatrists as consultants and a background resource for general practitioners and nonpsychiatrist mental health providers.
Implementing this set of recommendations would facilitate general practitioners' collaboration with psychiatrists and qualified nonpsychiatrists as providers of psychotherapy to improve the adequacy of mental health treatment and services by increasing the availability of mental health providers. These measures will require strong commitment from health authorities and active participation of professional organizations, as well as widespread public information campaigns, such as the recent campaign on depression by the French Institut National de Prévention et d'Éducation à la Santé (
46), which was partly inspired by the “Defeat Depression” campaign in the United Kingdom.
Acknowledgments and disclosures
The ESEMeD project is funded by the European Commission (contracts QLG5-1999-01042 and SANCO 2004123); the Piedmont Region (Italy); Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028); Ministerio de Ciencia y Tecnologáa, Spain (SAF 2000-158-CE); Departament de Salut, Generalitat de Catalunya, Spain;Instituto de Salud Carlos III (CIBER CB06/02/0046, RETICS RD06/0011 REM-TAP), and other local agencies and by an unrestricted educational grant from GlaxoSmithKline. The World Health Organization World Mental Health (WMH) Survey Initiative is supported by the National Institute of Mental Health (R01-MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the U.S. Public Health Service (R13-MH066849, R01-MH069864, and R01-DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, GlaxoSmithKline, and Bristol-Myers Squibb. This report was prepared under the auspices of the World Health Organization
ICD-11, Chapter 5 (“Mental and Behavioural Disorders”), Epidemiology Working Group, which is co-chaired by Somnath Chatterji, M.D., and Ronald Kessler, M.D. A complete list of WMH publications is available at
www.hcp.med.harvard.edu/wmh. Financial support was also received from French CNAM-TS (Caisse Nationale d'Assurance Maladie, des Travailleurs Salariés [French National Public Health Insurance for Employees]). None of the funders had any role in the design, analysis, interpretation of results, or preparation of this article. The views and opinions expressed are those of the authors and should not be construed to represent the views of the sponsoring organizations, agencies, or governments. The authors thank the staff of the WMH Data Collection Centre and Data Analysis Coordination Centre for assistance with instrumentation, fieldwork, and consultation on data analysis.
The authors report no competing interests.