In Virginia, community service boards (CSBs) serve as a single point of entry into publicly funded mental health services, intellectual disability services, and substance abuse services, providing both outpatient and inpatient hospitalization. CSBs are part of a move toward an integrated system of care, which focuses on establishing community services and making more efficient and effective use of state facilities. Begun in 1968, CSBs were established by the Code of Virginia as local government agencies to function with input from locally appointed board members. Resources are allocated to each CSB by the Commonwealth on the basis of a calculated formula, and each CSB can apply for and obtain additional funding (such as federal grants and county funds). As such, the resources of all CSBs in the state are not equal. Forty CSBs are operating in Virginia and offer varying combinations of nine core services based on the recovery model (
1): emergency services, local inpatient care, outpatient care, case management, day treatment support, employment support, residential support, prevention and early intervention, and limited other services. Of these services, only emergency services and, subject to the availability of funds appropriated, case management are mandated by law.
Although the quantity and mix of outpatient services at each CSB vary significantly, how this variation influences the health of the population is unclear. This study sought to determine whether a greater availability and variety of community-based services are correlated with more outpatient service visits and lower hospitalization rates. Although some hospitalization is necessary to stabilize individuals in crisis situations, the question addressed in this study was whether services provided in the community can substitute for at least some hospitalization days.
Using a multivariate regression approach, we first examined whether individuals who live in regions with greater availability and variety of services obtain more services. Second, we analyzed the relationship between the use of outpatient services and the number of hospitalization days. We expected proxies for availability of regional services to be correlated with a greater use of outpatient services. Furthermore, we expected the variety of services available at a CSB to be positively correlated with the number of services that an individual obtains. Finally, we expected the receipt of more outpatient services to be correlated with fewer hospitalization days.
There is a large body of literature that has examined the extent to which community-based mental health services can offset total medical utilization. Mumford and colleagues (
2) surveyed the literature and found that 85% of the studies reviewed showed that a decrease in overall medical utilization was associated with psychotherapy. Alternatively, Sturm (
3) argued that extrapolation to the general population generally dilutes offsets and that, for underserved populations, access to more mental health services often results in greater overall medical utilization. These studies, however, focused on aggregate medical utilization, not utilization of mental health services.
Several studies have specifically linked use of community mental health services with hospital admissions. Shaeffer and colleagues (
4), for example, focused on two counties in Pennsylvania over a ten-year period and concluded that the introduction of enhanced community services reduced state hospital admissions. Several international studies have also found significant advantages to outpatient care. Pirkola and colleagues (
5) used small-area analysis and reported that the prominence of outpatient services relative to inpatient services was associated with lower suicide rates in Finland. Madianos and Economou (
6) found that community services in Athens, Greece, including medical monitoring, outreach, and day treatment, were effective at reducing hospitalization. Hyun and colleagues (
7) found that community services decreased the probability of rehospitalization and length of stay. These studies suggest that treating more patients in the community through outpatient services at CSBs could provide a substitute for hospitalization.
In addition to being influenced by availability, outcomes are influenced by the intensity of outpatient care. A randomized controlled experiment in North Carolina found that outpatient commitment, complemented by intensive treatment, improved health outcomes (
8). Individuals who underwent sustained outpatient commitment beyond the initial court order had 57% fewer readmissions and averaged 20 fewer hospital days (
9). However, mandatory outpatient laws vary across states and are frequently not applied. Our study did not focus on outpatient commitment, which is rarely used in Virginia, but we did investigate the importance of availability and variety of outpatient services.
Not all studies have found that additional outpatient mental health treatment reduces inpatient treatment. Kolbasovsky and colleagues (
10) used administrative data and found that more mental health hospital visits, longer hospital stays, and more outpatient service visits were associated with a higher probability of readmission. Although that study controlled for a person's diagnosis, it did not control for the severity of a person's mental illness. To account for the influence of a person's health status on initial care and subsequent readmission and to avoid biasing results, Figueroa and colleagues (
11) used an instrumental variables approach to control for how severity of illness affects both inpatient and outpatient care. They found that longer inpatient stays were significantly associated with reduced readmission rates.
In addition to medical care, community characteristics have also been correlated with hospitalization rates (
12). Konrad and colleagues (
13) estimated the need for mental health workers and found a significant variation in need for mental health professionals based on demographic and geographic characteristics. Ellis and colleagues (
14) examined variables that correlated with the supply of mental health professionals and found a higher ratio of professionals in high-income, urban, high-population counties. In order to account for the influence of community characteristics, our study controlled for several variables, including poverty, per capita income, and population density levels.
Understanding how outpatient mental health services are related to hospitalization rates has important implications for health outcomes, as well as for the state's budget. Community mental health services not only have the potential to allow individuals to avoid crises and remain in the community longer, but they can reduce the cost of hospitalization. A relationship between community services and hospitalization also suggests that some cost-saving measures, such as cutbacks in reimbursements for community services by Medicare, could ultimately increase the cost of hospitalization.
Methods
The information for this study was obtained from Virginia's Medicaid claims files, as well as from public records on CSBs. [Tables providing county-level details on Virginia's CSBs are provided in an online supplement to this article at
ps.psychiatryonline.org.] The study was reviewed by the University of Virginia's Institutional Review Board and received exempt status because all data were blind-coded and deidentified by Medicaid data analysts before being provided for this study. Data were analyzed with Stata 10.0 statistical software.
The Medicaid claims database consisted of all Medicaid recipients aged 18–64 who had a mental disorder diagnosis (ICD-9 codes 290–319) between July 1, 2005, and June 30, 2008. The primary data set consisted of 11,107 individuals who had a consistent reference number for the same visit, a complete year of data after their first CSB visit, and at least nine months of Medicaid coverage during the year. Persons with a hospital stay of six months or longer were excluded from the study. From these individuals, the second data set included only the individuals with at least two ICD-9 diagnoses of schizophrenia-related disorders (diagnosis 295) or affective psychoses (diagnosis 296), which we defined as serious mental illness (N=6,324). The second data set was intended to determine whether CSBs have a different effect on individuals with more serious diagnoses.
To understand the relationship between use of outpatient mental health services and use of inpatient services, we first estimated factors that explain the frequency of outpatient visits. Second, we analyzed whether the use of outpatient services was negatively correlated with the individual's time spent hospitalized.
Estimating the use of mental health services was complicated by the fact that a person's health status influences both inpatient and outpatient service visits. We controlled for the severity of illness by including both individual characteristics and community characteristics. Individual characteristics included age, race, sex, and whether the individual had a serious mental illness. Race and sex were both dummy variables. Race was divided into three categories—white, black or African American, and other. White was the uncoded control variable. Age was treated as a continuous variable. Community characteristics included per capita income and population density, which controlled for the socioeconomic status of the population in the CSB region (mean±SD population of 190,948±170,905).
Virginia's CSBs can be divided into three types: operative, administrative policy, and policy-advisory. In addition, there is a behavioral health authority (BHA) in Richmond. The BHA and the operative and administrative policy CSBs are guided and administered by CSB boards of directors with fiduciary and management authority. The policy-advisory CSBs advise local governments, leaving the provision of services to the government. We used a dummy variable to control for the type of CSB available in a community.
Results
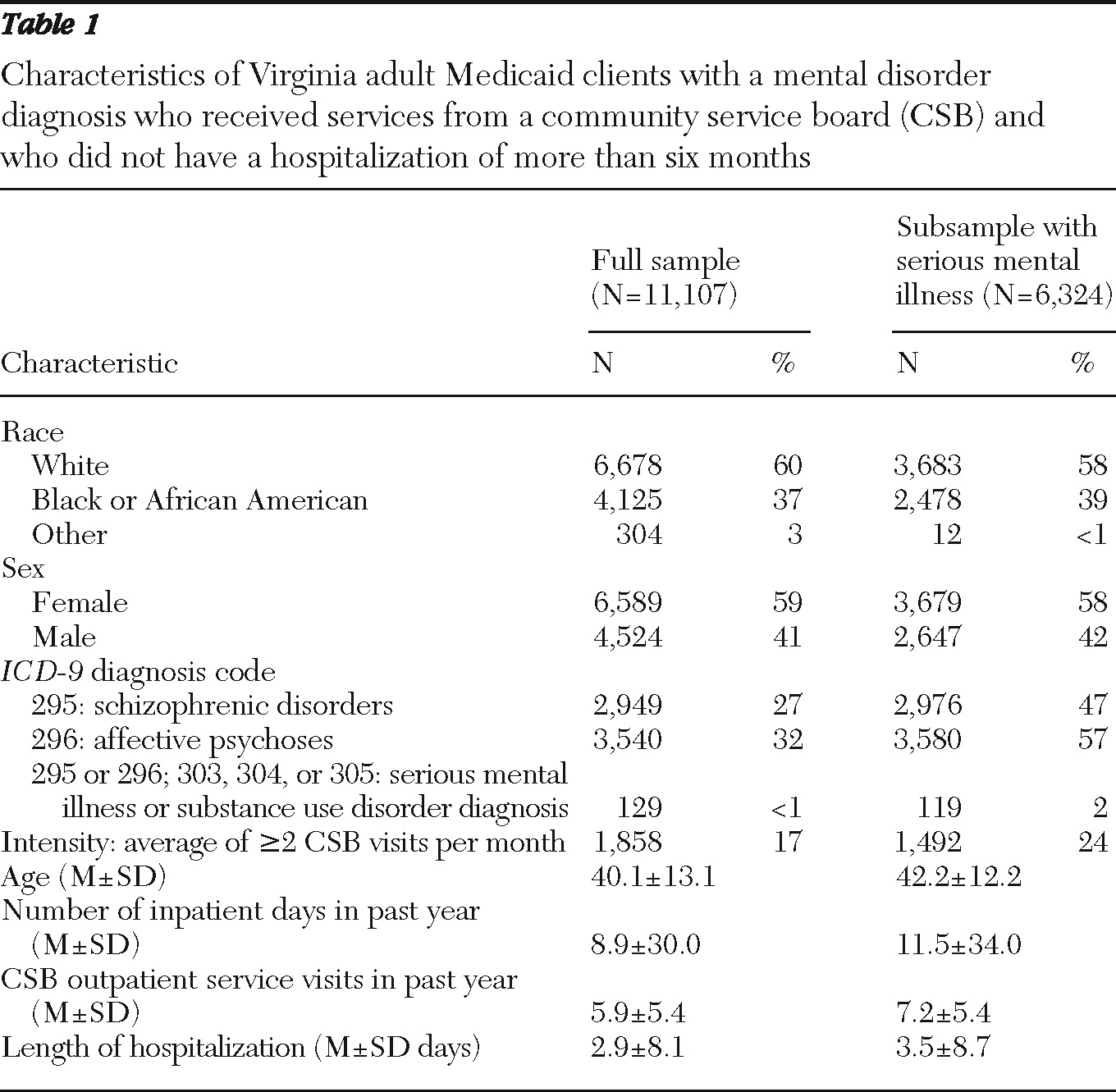
The composition of the final sample (
Table 1) was 59% female, 60% white, and 37% black or African American. Twenty-seven percent of the sample had at least two diagnoses of schizophrenia-related disorders (
ICD-9 code 295), and 32% had at least two diagnoses of affective psychoses (
ICD-9 code 296). The mean number of nights in a hospital was 8.9±30.0 nights per year. The average number of CSB outpatient service visits during the year after the index CSB visit was 5.9±5.4 visits per year.
Among individuals with a serious mental illness, the average cumulative number of days hospitalized in the past year was 12 days. Using chi square tests to compare proportions and t tests to compare means of the two populations, we found that race and age were statistically different, with the population with serious mental illness more likely to be nonwhite and older. Sex and average per capita income in the community were not statistically different between the full sample and those with a serious mental illness.
Virginia's CSBs vary in the quantity and variety of services provided. Ideally we wanted to capture the range of evidence-based interventions available, because CSBs could offer many services without clear effectiveness. The two measures of services available at CSBs, service index and current procedural terminology (CPT) codes, came from two sources. The crisis intervention service index is an unweighted count of the number of crisis intervention services available at each CSB and is based on the Mental Health Crisis Intervention Continuum Survey, conducted in November 2007. Although the index does not capture the relative importance of a service or the availability of noncrisis services, it provided an objective means to compare the variety of services available at each CSB. Alternatively, the CPT codes represent the different services that Medicaid has been billed for by each CSB. On average, CSBs billed 16.7±2.1 different CPT codes to Medicaid and provided 9.4±2.3 different crisis intervention services. Of CSB clientele, 57% had a serious mental illness.
Outpatient services
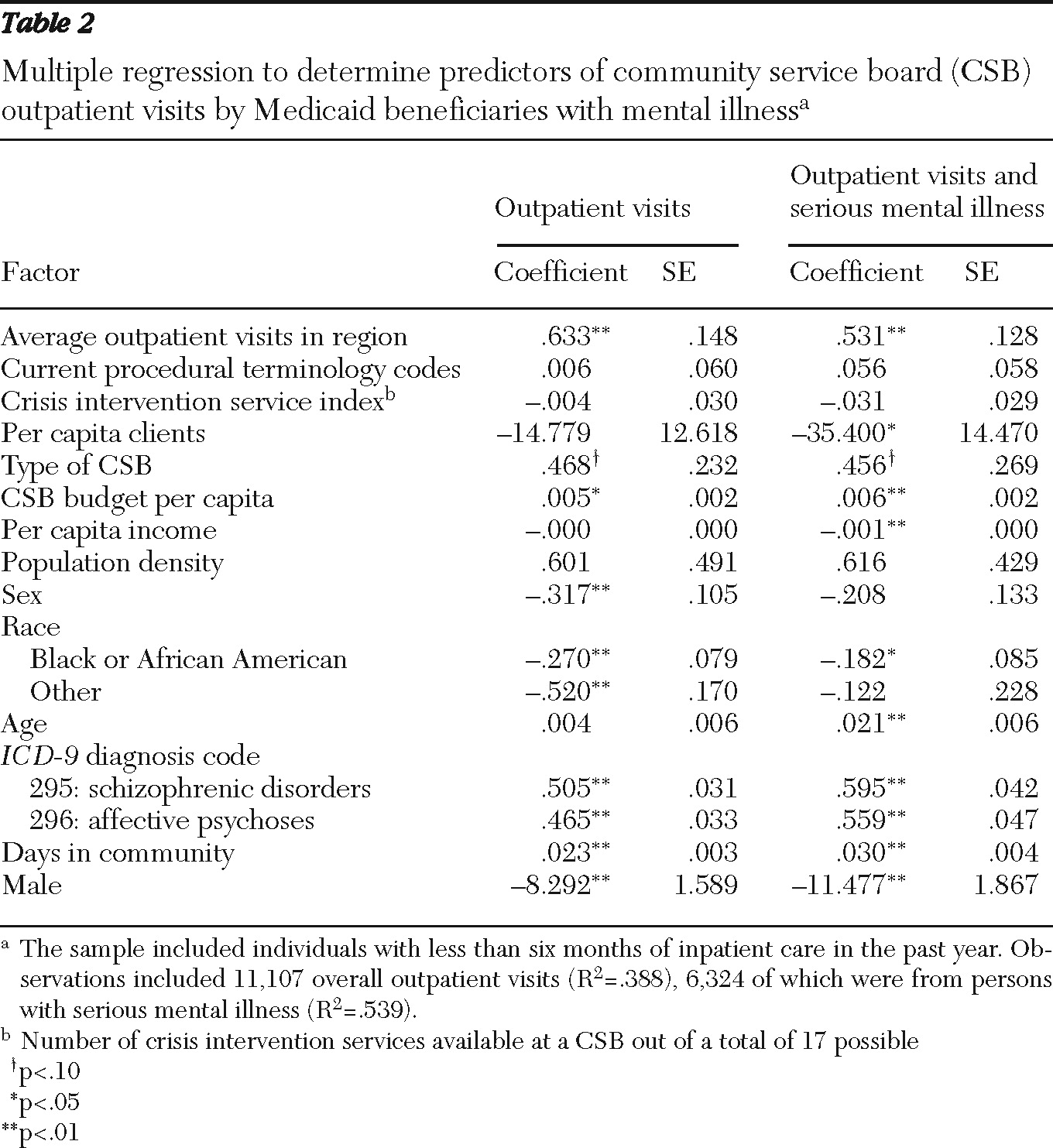
The empirical estimation revealed that the availability of community services was correlated with a greater frequency of outpatient CSB visits, which averaged 5.9±5.4 per year. Two of the proxies for availability of services, average number of CSB outpatient service visits in a region and the CSB budget relative to regional population ($133±$69 per capita for 1,684±114 clients per 100,000 population), were both strongly correlated with the number of outpatient visits (
Table 2). This result is consistent with the fact that Medicaid recipients receive more services when a larger quantity of services is available in a community.
Alternatively, the proxies used to measure the variety of mental health services that are available were not correlated with use of outpatient services by Medicaid recipients. Neither the variety of CPT codes billed to Medicaid nor the service index was correlated with CSB outpatient visits. We also examined each of the 17 index services as separate dummy variables and found that although some were significant, jointly they did not significantly improve the fit of the model. The lack of correlation may indicate that the quantity rather than the variety of services available affects hospitalization. Alternatively, our proxies for variety may not have adequately captured the services available.
In the full sample and the subsample with serious mental illness, being male increased the number of outpatient service visits, as did being white. The number of days spent in the community was also included to control for the amount of time that an individual could potentially have obtained outpatient services and, as expected, was positively correlated with the number of CSB visits.
For the full sample the characteristics explained nearly 40% of the variation in outpatient care observed across Virginia (R
2=.388). For the subsample of individuals with a serious mental illness, the explanatory variables explained just over half of the variation (R
2=.539) (
Table 2). The explanatory power suggests that many but not all of the important individual and regional characteristics were captured.
Inpatient care
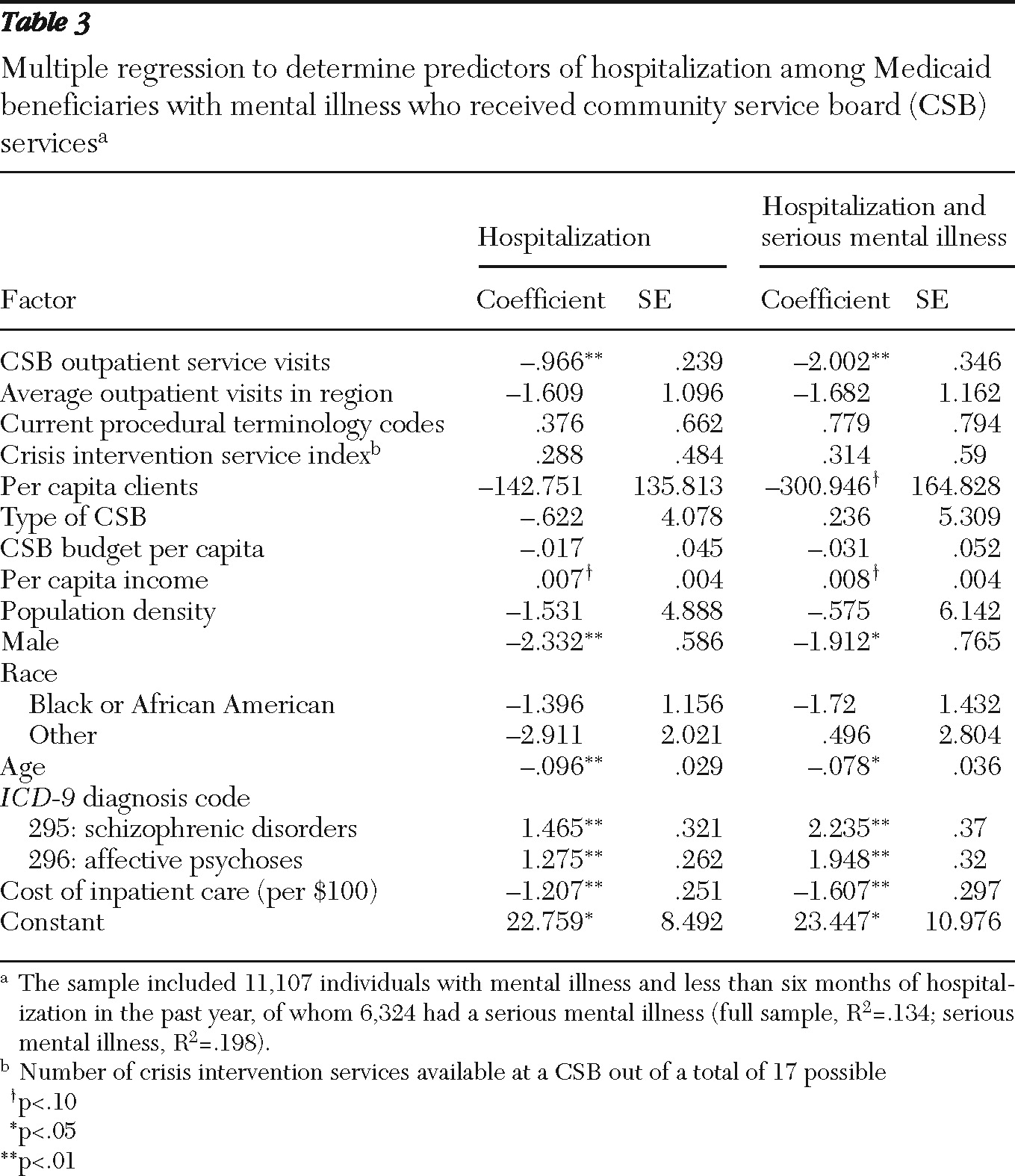
The next step was to examine how use of outpatient CSB services was related to the time that individuals spent hospitalized. As expected, the regression results revealed a negative correlation between inpatient and outpatient service visits (
Table 3). Although the data were not sufficient to draw conclusions about causality, these results are consistent with our hypothesis that outpatient CSB service visits reduce hospitalization days.
The average cost paid by Medicaid per region of residence was correlated with hospitalization days. Being male and being younger were correlated with more hospitalization. Race, however, did not factor into the likelihood of hospitalization. The availability and variety of outpatient services showed no correlation with inpatient days, possibly because the actual number of visits was also included in the regression. Finally, having a serious mental illness was significantly correlated with more hospitalization days.
Putting the results together, we found that an increase in availability of services in a region was correlated with increased use of outpatient services, which in turn was correlated with less time hospitalized. Although the results are consistent with community-based services' reducing hospitalization, further research is needed to identify causality and to control for possible changes in policies that may influence admissions, availability of services, and other factors that could affect both inpatient and outpatient care.
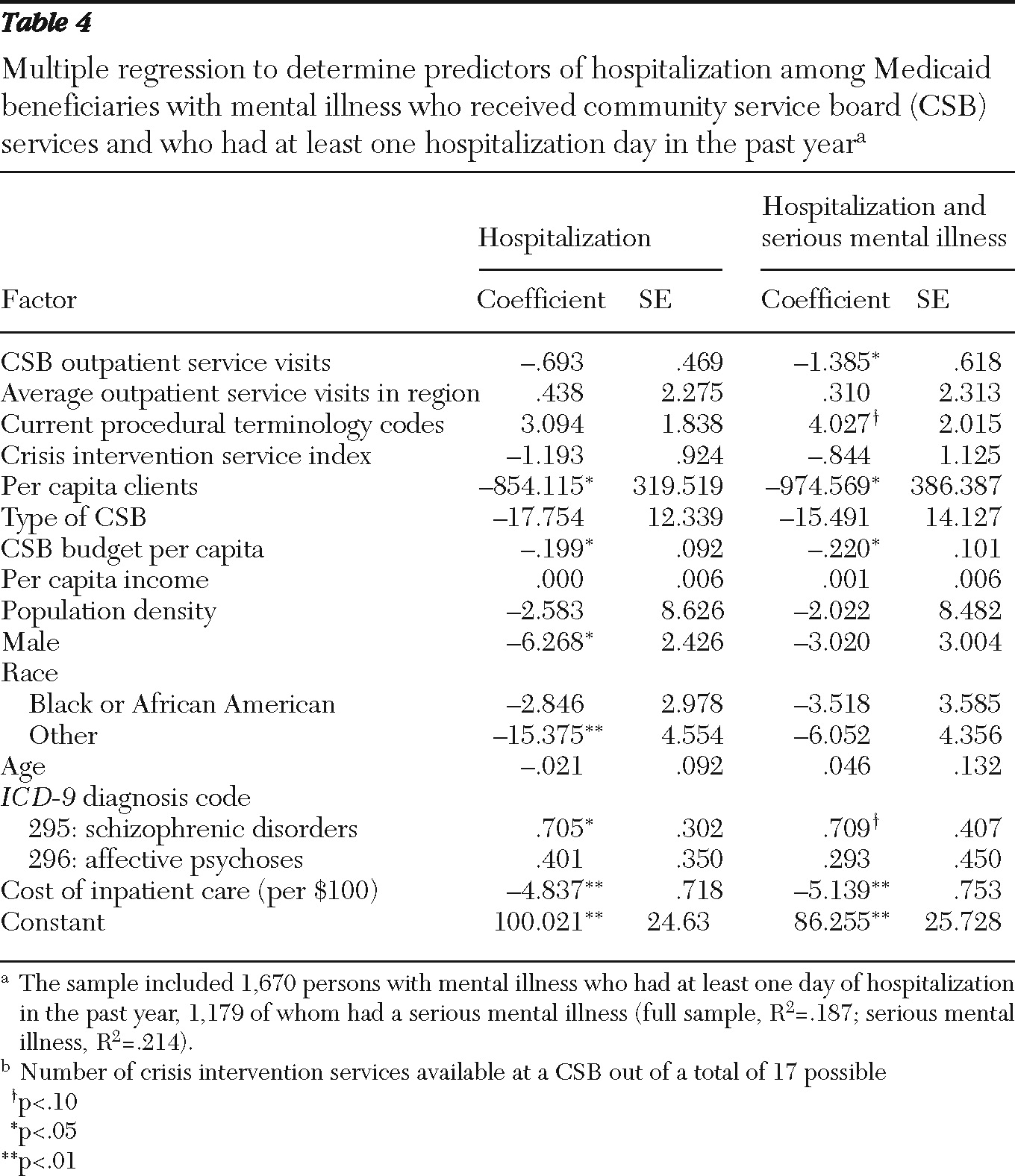
To further isolate the effects of outpatient service visits on inpatient days, we examined the subsample of individuals with at least one inpatient day. Excluding nonhospitalized individuals had the advantage of focusing only on those who clearly had the possibility of shortening their hospital stays. The disadvantage of this approach was that it potentially underrepresents the importance of outpatient services, in that the individuals who avoided hospitalization because of the presence of CSB services were inaccurately excluded. However, we have no means to distinguish between the individuals who were helped by the CSB and those who would not have been hospitalized regardless of CSB services.
The reduced sample of hospitalized individuals included 1,670 individuals from the full sample and 1,179 individuals from the subsample with serious mental illness. Estimating the model using the reduced sample revealed that those with serious mental illness and making CSB outpatient service visits had fewer hospitalization days (
Table 4). In addition, reduced availability of services, measured by per capita clients and CSB budget, was correlated with higher rates of inpatient days. The results are consistent with the hypothesis that the increased availability of outpatient services is correlated with a reduction in inpatient days among those with a serious mental illness.
Discussion
The study findings were consistent with our hypothesis that increasing the availability of CSB services in an area could reduce the need for hospitalization, at least among Medicaid recipients with a diagnosed mental illness. Although we identified a correlation between use of community services and hospitalization days, an important limitation of this study is the lack of a data set to allow identification of causality. Our data set did not permit us to determine the direction of the correlation, nor can we rule out a potential third factor that may have both variables in common. It would be valuable to revisit this issue with a longitudinal data set that would permit analysis of causal relationships.
A second limitation of this study is the lack of more comprehensive data on community mental health services. The measures used as proxies for availability—per capita clients and CSB budget—and for variety—CPT codes and service index—may not be the best proxies for the actual provision of services in a community. Better proxies, including quality of services, admissions policies, and overall consumer health outcomes, may illuminate why the variety of services was not a significant factor in predicting use of services.
Third, this study was limited to Medicaid recipients in Virginia who had at least one mental disorder diagnosis and made at least one CSB visit. Thus its general applicability is unclear. Fourth, there may be additional variables not included in this study, such as language literacy, an individual's distance from service providers, and other regional differences, that influence use of services.
Finally, this study did not address the costs of different services. A major policy implication of this study is that increasing the availability of outpatient services would reduce hospitalization, which presumably would reduce costs to the government. Data on the monetary trade-offs between inpatient and outpatient services would provide valuable information for policy makers.
Conclusions
People deserve care that provides the best clinical and functional outcomes. Beyond its cost, hospitalization is disruptive to the lives of individuals with a mental illness. Because community-based care allows people to continue to function in their daily activities, it has the potential to improve outcomes.
Using regional variations across Virginia, this study looked at the extent to which increased availability and use of community-based outpatient services were correlated with fewer hospitalization days. The results revealed that among Medicaid recipients greater availability of community-based services was correlated with more frequent outpatient visits. Furthermore, the frequency of outpatient visits was correlated with a decrease in hospitalization days. We did not, however, find a correlation between variety of outpatient services and length of inpatient stays, suggesting that it may be the quantity, not the type of service, that matters.
This study has important policy implications. Although more research is needed to establish causality and to identify the most effective outpatient services, it provides an initial glimpse into the extent to which community-based services can substitute for inpatient care. The results are consistent with increasing the availability of outpatient services as a means to reduce the need for inpatient care and allow individuals to remain longer in the community. Thus the results have the potential to motivate policies that encourage greater provision of community-based services as a means to improve health outcomes.
Acknowledgments and disclosures
The authors acknowledge support from the Department of Behavioral Health and Development Services and the Commission on Mental Health Law Reform of the Commonwealth of Virginia, as well as personal assistance from Rhonda Newsome, M.P.P., and Aaron Bloomfield, Ph.D.
The authors report no competing interests.