Between the years 2000 and 2030 the number of older adults with major psychiatric illnesses is expected to more than double, from seven million to 15 million (
1). Mental illnesses among older adults are associated with functional disability (
2–
4), cognitive impairment (
5,
6), compromised quality of life (
7–
10), increased health care utilization and costs (
11–
13), barriers to preventive care (
14), and poor health outcomes (
15,
16) and mortality (
17–
19). However, mental illnesses among older adults are often unrecognized, untreated, or undertreated (
2,
20–
24).
Researchers have identified many barriers that contribute to poor access to and inadequate utilization of mental health services by older adults with mental illness, such as fear of stigmatization (
2,
25,
26), negative beliefs about mental illness (
27), limited knowledge about mental illnesses and mental health services (
28), mismatch between the current system of care and the needs and preferences of older adults (
21,
29,
30), a fragmented system of mental health care for older persons (
2,
21), and financial costs for mental health services (
2,
21,
23). Underdetection of mental health problems and suboptimal treatment with overreliance on pharmacotherapy in primary care settings are also often reported (
21,
24,
31,
32).
However, recent developments may significantly increase care seeking and use of mental health services among older adults. For example, researchers have found that younger cohorts of older adults view mental health problems and treatments more favorably than older cohorts (
33). Other relevant developments include increased public knowledge about mental health problems and aging (
22), advances in effective treatments for geriatric depression and cognitive symptoms of dementia (
21), increased use of alternative mental health services (
34–
37), as well as collaborative care for late-life depression in the primary care setting, resulting in greater access to mental health services (
31,
32) and improved treatment outcomes (
31).
Thus it is important to estimate the current prevalence of mental health problems among community-dwelling older adults in the United States and to understand their use of mental health services. Although one peer-reviewed study used national data to examine mental health service utilization among older adults, the data for the study were collected more than a decade ago (
38). Two recent government reports indicated that the prevalence of past-year serious psychological distress was lower among older adults than among younger adults; however, among adults with serious psychological distress, older adults have a lower rate of mental health treatment than younger adults (
39,
40). However, none of these studies (
38–
40) examined factors associated with serious psychological distress and mental health services use among older adults.
To address these gaps in knowledge, this study first estimated the prevalence of past-year serious psychological distress among community-dwelling older adults in the United States by using combined data from the 2004–2007 National Surveys on Drug Use and Health (NSDUH). Combined data provided a much larger sample and more precise estimates for this population than the previous studies (
38–
40). Second, we investigated indicators of health status and sociodemographic characteristics that are associated with serious psychological distress among older adults. Third, this study examined receipt of mental health services among older adults with serious psychological distress. Finally, we assessed indicators of health status and sociodemographic characteristics that are associated with receipt of mental health services in this population.
Methods
Data sources and sample
This study analyzed data from 9,957 adults aged 65 and older who participated in the 2004–2007 NSDUH, nationally representative surveys of the civilian, noninstitutionalized U.S. population. Although NSDUH does not sample persons residing in institutional group quarters, such as nursing homes and other long-term care facilities, those living in their own residences, including those in retirement communities, are included. The NSDUH is a face-to-face survey conducted at the respondent's home. The average interview response rate among adults aged 65 or older for the 2004–2007 NSDUH was 66%. Approximately 8%–9% of selected older adults were unable to participate in the survey because they were judged to be mentally or physically incapable. Further description of the survey is available on the Web site of the Substance Abuse and Mental Health Services Administration (
41).
Measures
Past-year serious psychological distress.
The NSDUH measures past-year serious psychological distress with the K6 scale, a nonspecific psychological distress indicator of past-year mental health problems, such as anxiety and mood disorders (
42–
44). The K6 asks about the frequency of each of six symptoms of nonspecific psychological distress during the one month in the past 12 months when the respondent was at his or her worst emotionally. Respondents with a score of ≥13 (possible range 0–24) are considered to have serious psychological distress (
42). The K6 has desirable internal consistency (
45) and is strongly predictive of adult serious mental illness (
44,
46).
Past-year mental health service use.
NSDUH also asks respondents to report their past-year experiences with mental health services, including the receipt of “traditional” mental health services (outpatient or inpatient mental health treatment or use of prescription medication for a mental health problem) or “alternative” mental health services (for example, from an acupuncturist, chiropractor, herbalist, in-person support group or self-help group, Internet support group or chat room, spiritual or religious advisor, telephone hotline, or massage therapist).
Indicators of health status.
NSDUH includes data on the respondent's self-rated health (excellent, very good, good, fair, or poor), the number of past-year general medical conditions that the respondent was told by a medical professional that he or she had, and the number of emergency room visits (for any reason) in the past year (none, one, two, or three or more). On the basis of
DSM-IV criteria (
41,
43), the NSDUH also assesses whether a respondent had a past-year major depressive episode and a past-year substance use disorder (alcohol or illicit drug) because mental health and overall health are associated with substance use (
47–
49). These measures have good validity and reliability (
50–
52).
Sociodemographic characteristics.
This study also included the following sociodemographic variables in the analyses: age (65–74, 75–84, and ≥85), gender, race-ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), education status (less than high school, high school, some college, or college graduate or above), marital status (married or nonmarried), health insurance (Medicare, Medicare plus private insurance, Medicare plus Medicaid, or other types), annual family income (<$20,000, $20,000–$49,999, $50,000–$74,999, or ≥$75,000), and metropolitan statistical area (yes or no).
Analytic strategy
Descriptive analyses were conducted to estimate the prevalence of past-year serious psychological distress and receipt of mental health services among community-dwelling older adults. Multivariate logistic regression modeling was applied to investigate characteristics associated with serious psychological distress among older adults and factors associated with their mental health service utilization. To create and finalize a logistic regression model, we considered both indicators of health status and sociodemographic factors for guiding the potential variable selection and the Hosmer-Lemeshow goodness-of-fit tests for determining the adequacy of the fit of the model (
53). Analyses used SUDAAN software (
54) to adjust for the complex sample design and sampling weights of the NSDUH.
Results
Characteristics of the study sample
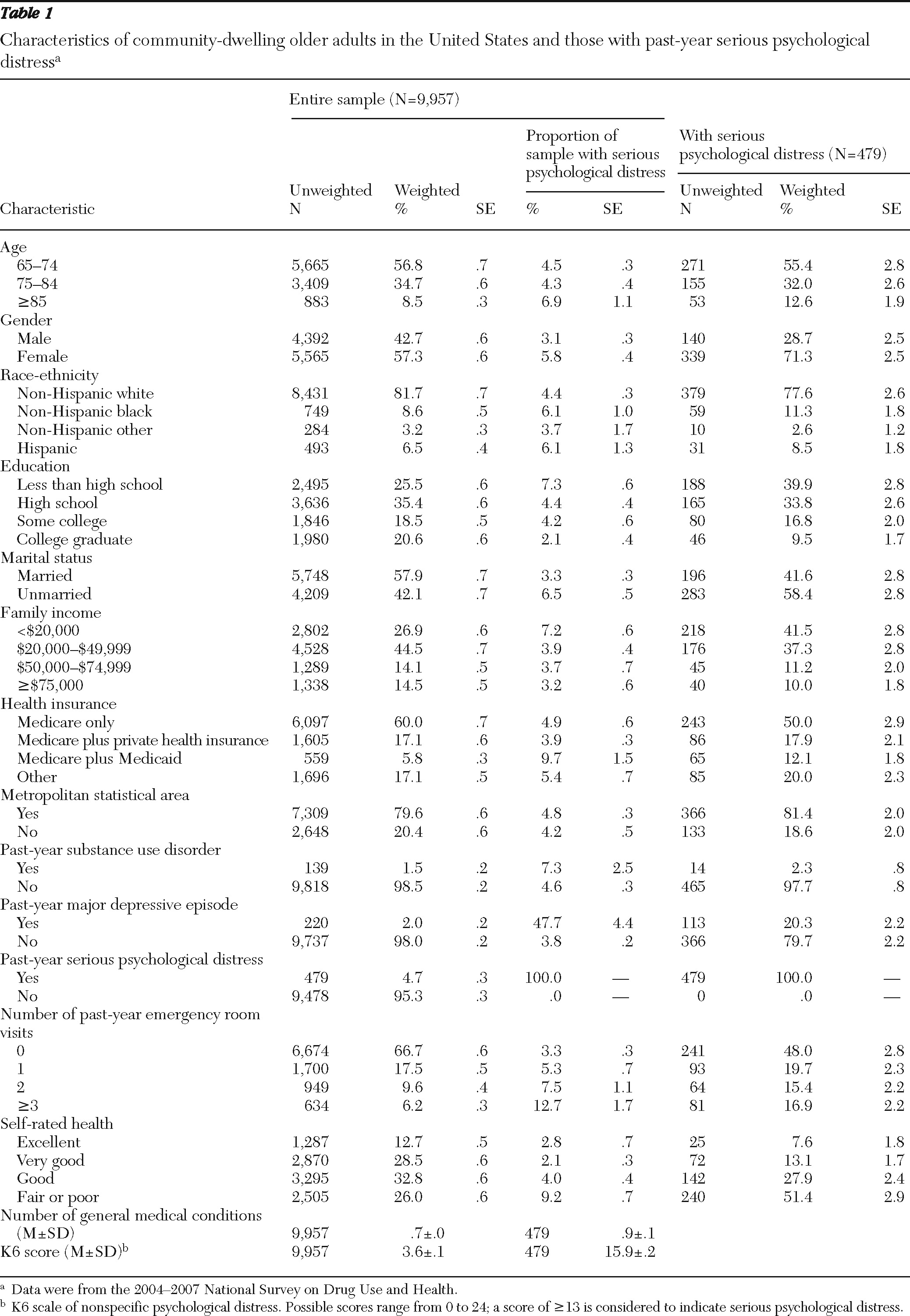
Table 1 presents characteristics and prevalence rates (weighted percentages) of serious psychological distress among the sampled 9,957 older adults. In the past year, 1.5% had a substance use disorder, 2.0% had a major depressive episode, 4.7% had serious psychological distress, 33.3% reported one or more emergency room visits, 26.0% rated their health as fair or poor, and their mean K6 score was 3.6.
Characteristics of adults with serious psychological distress
Table 1 also presents characteristics of the sampled 479 community-dwelling older adults with past-year serious psychological distress. In the past year, 2.3% of them had a substance use disorder, 20.3% had a major depressive episode, 52.0% reported one or more emergency room visits, 51.4% rated their health as fair or poor, and their mean K6 score was 15.9.
Factors associated with serious psychological distress
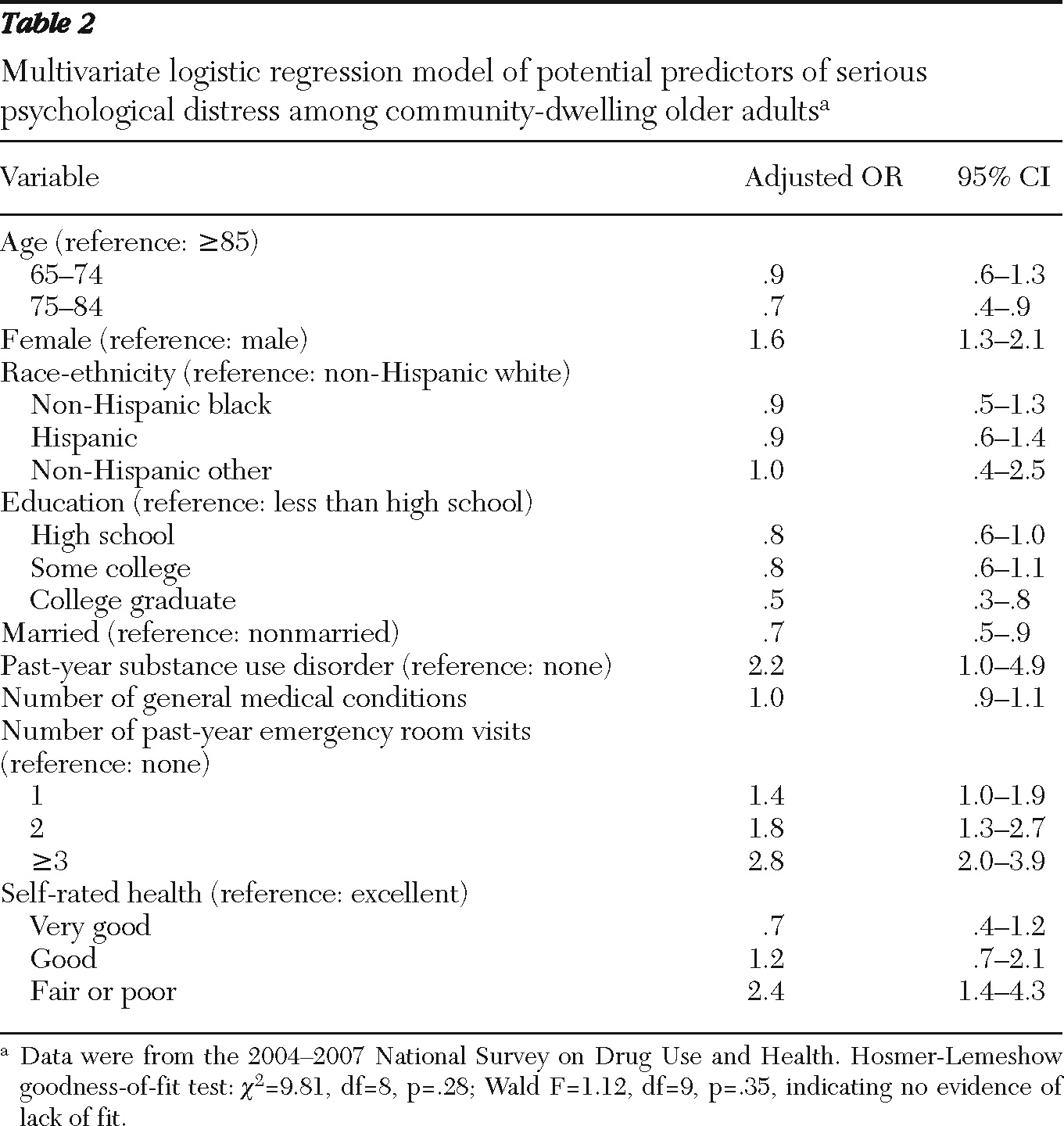
Table 2 presents the results of the final multivariate logistic regression model examining factors associated with past-year serious psychological distress. The Hosmer-Lemeshow test of the model showed no evidence of lack of fit. The multivariate results indicate that adults aged 75–84 were less likely than those aged 85 and older to have serious psychological distress (odds ratio [OR]=.7). Women were more likely than men to have serious psychological distress (OR=1.6). College graduates were less likely to have serious psychological distress than those with less than a high school education (OR=.5). Married adults were less likely than nonmarried adults to have serious psychological distress (OR=.7). Those with one or more emergency room visits in the past year were more likely to have serious psychological distress than those without any visits (range of ORs=1.4–2.8), as were those who rated their health as fair or poor (OR=2.4), compared with those with excellent self-rated health.
Mental health service use
As shown in
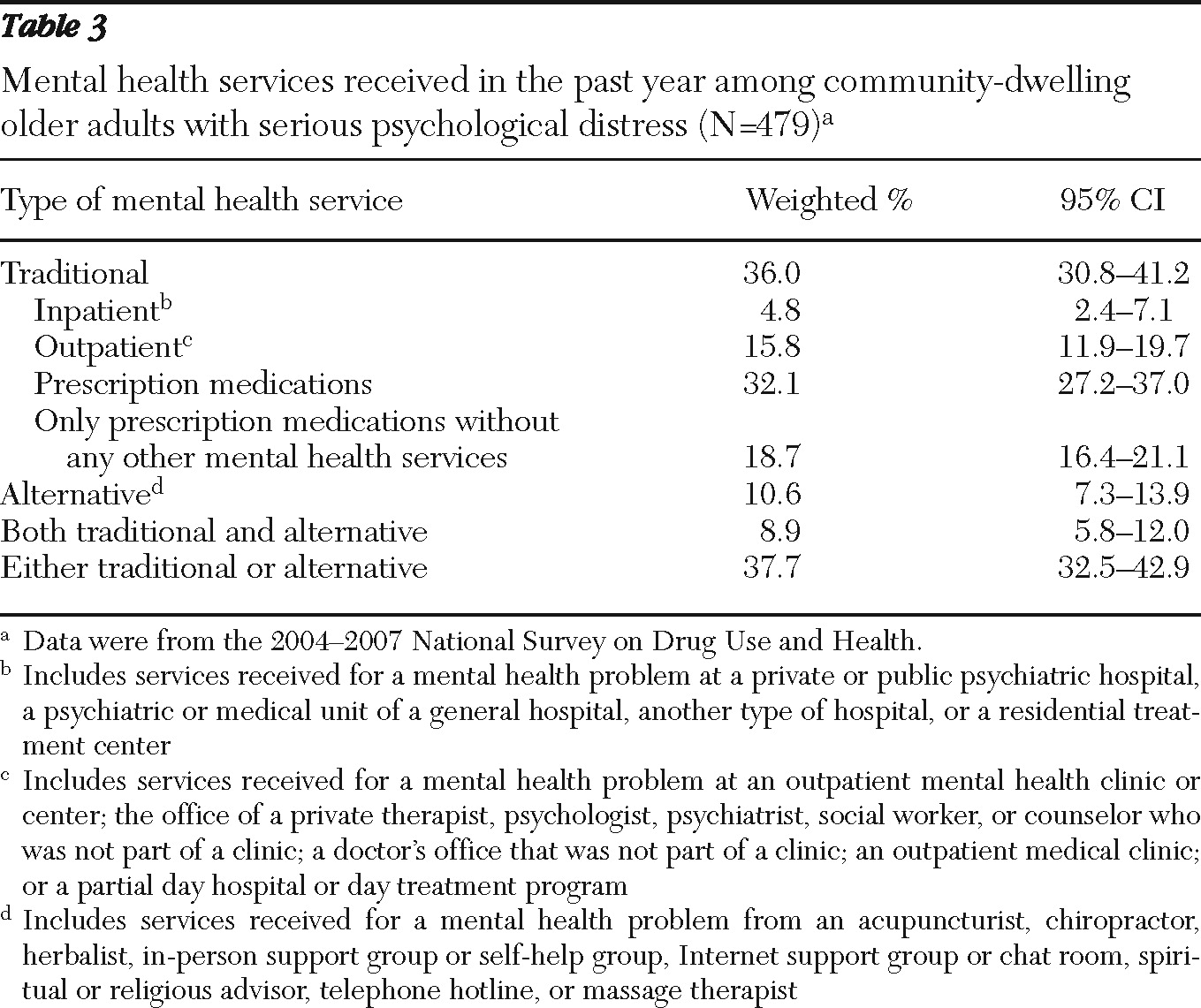
Table 3, among the older adults with past-year serious psychological distress, 36.0% received traditional mental health services, 10.6% received alternative services, and 8.9% received both traditional and alternative services in the past year. In addition, 4.8% of those with serious psychological distress received inpatient mental health services, 15.8% received outpatient services, and 18.7% received only prescription medications without any other mental health services in the past year. Overall, 37.7% received either traditional or alternative mental health services in the past year, which means that a large proportion—62.3% (95% confidence interval [CI]=57.1%–67.5%)—received no mental health services.
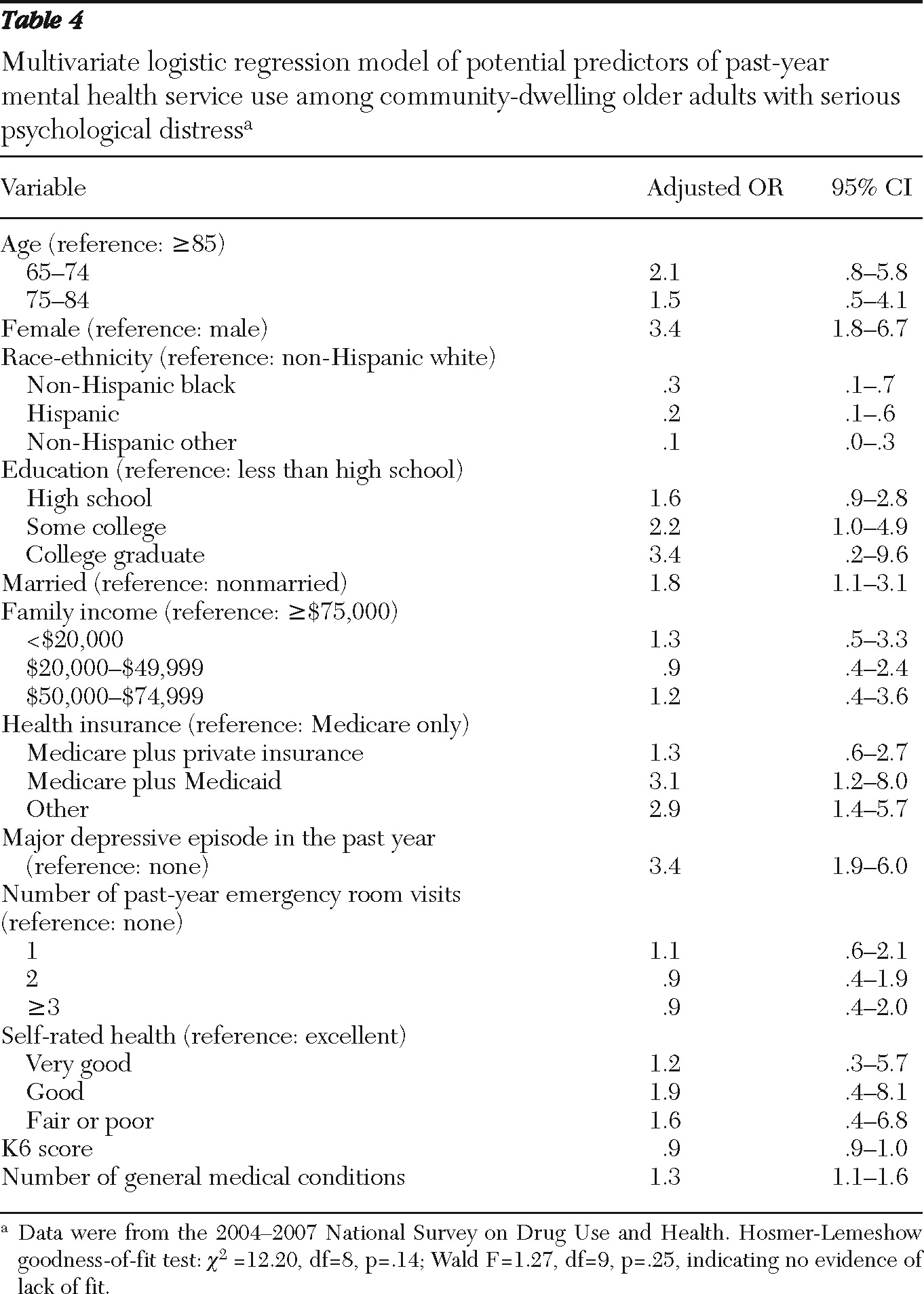
Table 4 presents the results of the final multivariate logistic regression model predicting mental health service use in the past year among older adults with past-year serious psychological distress. The Hosmer-Lemeshow test showed no evidence of lack of fit. After adjustment for covariates, women were more than three times as likely as men to receive mental health services in the past year (OR=3.4). Compared with non-Hispanic whites, non-Hispanic blacks and Hispanics and non-Hispanic others in the “other” category were less likely to receive services (OR=.3, .2, and .1, respectively). College graduates were more than three times as likely as those with less than a high school education to receive services (OR=3.4), and married adults were nearly twice as likely as nonmarried adults to receive services (OR=1.8). Compared with those covered by Medicare only, Medicare and Medicaid dual beneficiaries were more than three times as likely to receive mental health services (OR=3.1). Those with a past-year major depressive episode were more than three times as likely to receive services as those without an episode (OR=3.4). With each incremental increase in the number of past-year general medical conditions, older adults with serious psychological distress were 1.3 times more likely to have received mental health services in the past year (OR=1.3).
Discussion
This study used data from the 2004–2007 NSDUH to examine the prevalence and predictors of serious psychological distress and receipt of mental health service use among community-dwelling older adults in the United States. In this population, 4.7% had serious psychological distress in the past year. Although several new developments may help increase mental health service use among older adults (
21,
22,
31–
37), this study revealed that 62.3% of community-dwelling older adults with past-year serious psychological distress did not receive mental health services in the past year. Among those with past-year serious psychological distress, 4.8% received inpatient mental health services, 15.8% received outpatient mental health services, and 32.1% received prescription medications for their mental health problems in the past year. These results are similar to findings from a previous study based on national data collected in 1997–1998 (
38).
A recent study examining U.S. trends in mental health treatment expenditure from 1986 to 2003 also indicated that more care was being provided through prescription drugs, less in outpatient settings, and much less in inpatient settings (
55). Our findings indicate that this pattern has remained unchanged among older adults with past-year serious psychological distress, according to 2004–2007 NSDUH data. Studies of evidence-based best practices have consistently shown that combining prescription drugs with psychological or psychosocial interventions tends to be associated with better outcomes among older adults with mental health problems (
21,
23). However, these studies show that among older adults who used mental health services from 1986 through 2007, many received only pharmacological treatment (38% in this study), possibly reflecting the inadequate supply and training of geriatric mental health clinicians or the financial incentives inherent in many fee schedules for providing medication management rather than psychosocial treatments. Significant changes are needed in the mental health service delivery system for older adults in order to provide optimal therapeutic options and improve the quality of their mental health care.
Even after adjusting for differences in income, other sociodemographic characteristics, and case mix, this study found that older adults with past-year serious psychological distress who were covered by both Medicare and Medicaid were 3.1 times more likely to receive mental health services than their counterparts with Medicare only. This important finding may reflect differences in copayments and prescription drug coverage in 2004–2007. Compared with Medicaid, Medicare requires a much higher copayment for a limited range of psychologically based services (
21,
56). Moreover, before the implementation of the Medicare Part D drug benefit in 2006, Medicare did not provide a prescription drug benefit, whereas Medicaid did (
21,
57–
63).
Since 2008, however, there have been significant changes that have revolutionized payment for mental health care and that may be essential to promoting adequate access to mental health care among older adults. First, the enactment of the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 required that insurance coverage of mental health and substance abuse services be equal to coverage of general medical and surgical care. Second, the Medicare Improvements for Patients and Providers Act of 2008 addressed the inequity of a 50% copayment by beneficiaries for Part B outpatient mental health services, compared with a 20% copayment for general medical care. By 2014, the mental health copayment will decrease to 20%. Third, according to the Kaiser Family Foundation, among the 47 million Medicare beneficiaries in 2010, about 27.6 million (58.7%) were enrolled in Part D as of April 2010 (
64). Many older Americans have had a prescription drug benefit since Medicare Part D became effective in 2006. Fourth, the Patient Protection and Affordable Care Act of 2010 reduces the amount that Medicare Part D enrollees are required to pay for their prescriptions when they reach the coverage gap (“donut hole”), which will be closed by 2020. Also under this act, Medicare beneficiaries will be entitled to an annual wellness visit and personalized prevention plan services starting in 2011, including a comprehensive health risk assessment with no copayment or deductible. Thus it will be critical to screen for mental health problems among older adults during their annual wellness visit, which may improve their access to mental health services. Further studies are needed to assess trends in mental health service utilization among older adults and the quality of their mental health care over time.
A few limitations of this study should be acknowledged. First, the NSDUH is based on self-report data, which are subject to recall and reporting bias. Second, about 8%–9% of selected older adults were unable to participate in the survey because they were judged to be mentally or physically incapable. Thus this study likely underestimated the prevalence of serious psychological distress among community-dwelling older adults in the United States. Third, although the K6 has very good concordance with independent clinical ratings of serious mental illness (
44,
46), it does not mean that every older adult with serious psychological distress meets diagnostic criteria for a mental disorder or requires treatment. Fourth, the 2004–2007 NSDUH did not ask whether some inpatient or outpatient mental health services were medication management visits, which also could represent pharmacologic treatment. Fifth, this study could not examine the impact of Medicare Part D on use of prescription medications for mental health problems because the 2004–2007 NSDUH did not ask whether respondents with Medicare were enrolled in Medicare Part D. Sixth, little is known about the appropriateness and effectiveness of the mental health services received by older adults with serious psychological distress because the NSDUH does not collect such data. Finally, further research is needed to examine whether there are differences in levels of mental health service use between dually eligible Medicaid and Medicare beneficiaries with mental illnesses and their counterparts with Medicare only.
Conclusions
Despite these limitations, the findings contribute to an understanding of the prevalence and predictors of serious psychological distress and receipt of mental health services among community-dwelling older adults. These results suggest the need to more effectively screen and treat mental health problems among older adults.
To better meet the unmet needs for services among older adults with mental illness, significant changes are needed in the mental health service delivery system to promote access to services, improve the quality of mental health services, and increase the number of professional providers with adequate training in geriatrics and mental illness. Since 2008 major policy changes have revolutionized payment for mental health care and may promote access to mental health care among older adults. Further studies are needed to assess trends and factors facilitating mental health service use and quality care among older adults.
Acknowledgments and disclosures
The authors report no competing interests.