Effective weight loss programs are critically needed for people with serious mental illness. The obesity rates among people in this population are at least as high as those among the general population and possibly higher, particularly for women (
1). Moreover physical health concerns associated with obesity are more prevalent among people diagnosed as having serious mental illness than in the general population and result in greater problems. A recent study found that potential life lost among clients of public mental health facilities numbers in the decades, compared with expectations of life span in the general population in the same states (
2). Heart disease, which is highly linked to obesity, was the leading cause of death. Health care costs of obese individuals diagnosed as having a mental illness are higher than for those without a mental illness (
3). In addition, obesity was found to have a more negative impact on health-related quality of life among people with schizophrenia and bipolar disorder than among a general population of individuals seeking weight loss programs (
4).
In fact, traditional weight loss programs may not meet the needs of this population. Many individuals with mental illness require adapted programs that address cognitive deficits and limited social and economic resources. The investigation of weight loss interventions that promote changes in lifestyle for people with serious mental illness is just beginning, but the initial results are promising. However, most studies have been small, short-term investigations at a single site that underrepresented participants from minority groups and focused on either physical activity or dietary changes but not both. Few used randomized controlled trial designs (
11,
5).
To address many of the limitations of previous research, we conducted a randomized controlled trial of the efficacy of a weight loss program among clients with serious mental illness after three and six months. It is the first study to examine whether use of medications associated with varying risks of weight gain affects outcomes of the intervention. Preliminary results are presented here.
Methods
A total of 136 individuals with serious mental illness were enrolled in the study. All of the participants were clients at one of four community mental health programs, three in the Kansas City area and one in Las Vegas. Participants were stratified by risk of weight gain associated with the medications they used. Those taking olanzapine, clozapine, or lithium were considered to be at high risk of weight gain; those taking risperidone, chlorpromazine, quetiapine, or valproate, at moderate risk; and those taking molindone, ziprasidone, fluphenazine, haloperidol, or aripiprazole, at low or no risk. The groups were chosen on the basis of consensus conference guidelines on antipsychotic drugs and obesity (
6).
At each site computer-generated random assignment was used to assign an equal number of individuals from each risk group to the weight loss program, called Recovering Energy Through Nutrition and Exercise for Weight Loss, or RENEW, or to a control group. The RENEW program is a 12-month intervention including a three-month intensive phase, a three-month maintenance phase, and a six-month intermittent support phase. It combines evidence-based weight loss strategies (
7) and psychiatric rehabilitation principles by incorporating social and instrumental support, goal setting, skills and transfer training, and compensatory strategies for cognitive impairments.
In the intensive phase participants attend a weekly three-hour session in which they learn about nutrition, participate in physical activity, set individualized goals, and eat a meal together. Participants are encouraged to reduce their daily calorie intake by 500 calories and engage in physical activity for at least 30 minutes every day. The intervention is delivered by a graduate-trained nurse, occupational therapist, or dietician (who may also be a trained fitness instructor). Participants receive two meal replacements a day; side dishes and breakfast are provided by participants. During the maintenance phase participants meet once a month for three hours and receive weekly phone support but are given no meal replacements. The intervention is not specifically adapted for a high number of African-American participants; however, it is sensitive to cultural differences. For example, participants are encouraged to identify food preferences and are offered ideas for preparing and modifying favorite foods in a healthful way.
Individuals in the control group received treatment as usual. Typical treatment included medication and case management and the opportunity for voluntary participation in day programming. No participants were restricted from attending wellness programming offered by their respective mental health centers. This study was approved by the institutional review boards of the University of Kansas Medical Center and Touro University Nevada. Participants provided written informed consent after receiving a complete description of the study.
Data were collected from 2007 to 2009 at the four sites and analyzed using SPSS 18 software. Repeated-measures analysis of variance examined the differences between the intervention and control groups for weight loss at three and six months. A secondary factorial analysis included the independent variable of risk of weight gain by medication group.
Results
A total of 89 of the 136 participants were still enrolled at six months, 47 in the RENEW group and 42 in the control group. Another 47 individuals had dropped out of the study voluntarily and thus were lost to follow-up. No differences were found between those who completed the study and those who dropped out for age, baseline weight, race, or risk of weight gain based on medication; however, a larger proportion of women than men dropped out (χ2=4.37, df=1, p=.037).
Of the 89 individuals who completed the study, 35 (39%) were male, and the mean±SD age was 44.6±10.9 years. A total of 54 (60%) were white; 30 (34%) were African American, and five (6%) were of other races. At baseline there were no statistically significant differences between the control and the RENEW groups for age, gender, race, or weight.
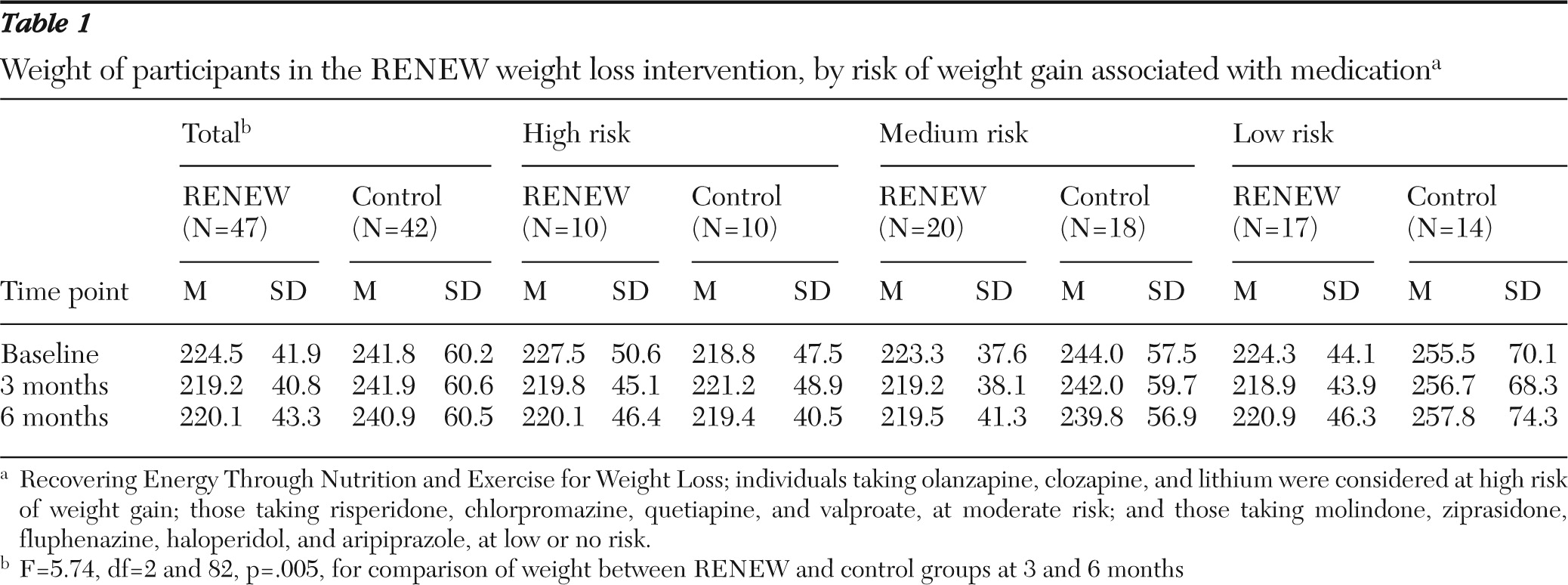
The RENEW group had lost more weight on average than the control group at three months (loss of 5.3 pounds versus a gain of .1 pounds) and six months (loss of 4.4 pounds versus loss of .9 pounds (F=5.74, df=2 and 82, p=.005) (
Table 1). Fifteen (32%) participants in the weight loss intervention had lost more than 10 pounds, compared with only four (10%) individuals in the control group. At three months 13 (28%) individuals in the RENEW group had lost 5% of their body weight, compared with only two (5%) individuals in the control group. Seven (15%) RENEW participants—but only one (2%) control group member—who had lost weight at three months went on to achieve 10% weight loss at six months. The largest weight loss for the RENEW group was 34.5 pounds after three months and 47 pounds after six months. However, some RENEW clients gained weight, as many as 24.6 pounds at three months and 49.8 pounds at six months. Those in the control group had lost as many as 31.5 pounds and gained as many as 24.5 pounds at three months. At six months, the largest gain in the control group was 25 pounds and the largest loss was 44 pounds. There was no significant difference in weight loss based on medication-related risk.
Discussion
The results indicate the RENEW program was successful in achieving modest weight loss for individuals with serious mental illness. Unlike many previous studies, this multisite randomized controlled trial included a significant number of participants from minority groups and promoted changes in both nutrition and physical activity. Its results are similar to those reported by other studies of weight loss interventions, which found a mean loss of 4.3±5.6 pounds (
5). Participants in the RENEW program had maintained their weight loss at six months; other studies indicate that individuals with serious mental illness who have participated in weight loss programs have maintained their weight loss for up to one year (
8,
9). A subgroup of RENEW participants lost 5% to 10% of body weight, an achievement that is associated with important health benefits such as reduced risk of diabetes and high blood pressure (
10).
The variability in weight loss indicates that the RENEW program was not equally effective for all participants. Although more people in the program than in the control group lost weight, some individuals enrolled in RENEW gained weight, and some individuals in the control group lost weight. Initial analyses revealed that gender, race, diagnosis, attendance at RENEW sessions, and risk of gaining weight due to type of medication were not indicators of treatment responsiveness, but small sample size may have contributed to an inability to detect predictors. Future studies should specifically examine predictors of weight loss.
The type of medication used was not related to either baseline weight or weight loss. Although medication-related weight gain should not be disregarded, the findings underscore that obesity is a concern for individuals with serious mental illness regardless of medication status. Perhaps more important, the efficacy of the program did not differ on the basis of risk of weight gain associated with various medications.
A limitation of the study is the loss of a large number of participants to follow-up and the inability to complete an intent-to-treat analysis. However, other studies of weight loss interventions with this population have reported mean retention rates of 70%±17% (
5), in the same range as the 65% retention rate in this study. A higher percentage of female dropouts suggests that women are less likely to continue with the RENEW program. One explanation could be that women tend to be more unrealistic in their weight loss goals (
11) and became discouraged with their progress. Moreover, the intensity of the intervention—which includes the use of meal replacements—may not be replicable for some settings. On the other hand, by using multiple sites and including significant numbers of participants from minority groups, the study increased the generalizability of its findings.
Conclusions
Obesity presents challenging health problems for individuals with serious mental illness that require effective interventions. This study of the RENEW program provides evidence that individuals with serious mental illness can benefit from weight loss programs.
Acknowledgments and disclosures
This project was supported in part by grant R34MH077282 from the National Institute of Mental Health and by Health Management Resources.
The authors report no competing interests.