Youths with an autism spectrum disorder (autistic disorder, Asperger's disorder, or pervasive developmental disorder not otherwise specified) are at high risk of comorbid mental health problems (
1,
2). As much as 70% of these youths have at least one comorbid mental disorder that may warrant mental health treatment (
2). In addition, mental health services are often provided to address behavioral problems and aggression (
3), which are features commonly associated with an autism-related diagnosis. Little is known, however, about the rate of mental health service use among these youths. Regional findings suggest that youths may underutilize mental health services (
4), but studies have not reported on national rates.
Schools play a central role in both providing and coordinating mental health services for all adolescents (
5,
6). A prior study of service use among adolescents across multiple sectors found that schools provided 70%–80% of the mental health services received and were the only source of care for most youths (
6). As growing numbers of youths with an autism-related disorder are identified and served through special education (
7), it is important to understand the role of the school in providing mental health services to them. We examined the prevalence and correlates of mental health service use overall, and then we examined the correlates of receiving a mental health service from school in the subgroup that had used a mental health service. In accordance with Andersen's behavioral model (
8), we grouped variables into predisposing factors that make an individual more likely to seek care, enabling resources that facilitate access, and need variables. This study was conducted to fill a gap in our knowledge by providing nationally representative information on mental health service use patterns in a population at high risk of mental health problems.
Methods
We used data from the first wave of the National Longitudinal Transition Study-2 (NLTS2), a nationally representative study of adolescents in special education. The NLTS2 used a two-stage sampling procedure and weighted the estimates to generalize to all students aged 13–16 in special education in 2000. Further details of the study sample design and weighting have been previously reported (
9).
Data were collected in 2001 through telephone interviews conducted in English or Spanish with parents or guardians of youths aged 13–17. Parents who were not reached by telephone were mailed a shortened self-administered questionnaire. Parents or guardians of 920 youths in the special education autism enrollment category responded, a rate of 84%. Use of these data is governed by a data use agreement with the U.S. Department of Education and was approved by the Washington University Institutional Review Board. All unweighted sample sizes were rounded to the nearest ten as required by the data use agreement.
Youths in the sample were selected on the basis of classification into the special education reporting category of autism, which does not require a
DSM-IV diagnosis of autism; hence we cannot report information about the specific type of autism-related disorder (such as Asperger's syndrome, autistic disorder, or pervasive developmental disorder not otherwise specified). Epidemiological surveillance data have shown that 99% of children served under the autism education designation also meet
DSM-IV criteria for an autism-related disorder (
10). However, some youths who met diagnostic criteria for an autism-related disorder may have been served under another eligibility category and would therefore not be included in this analysis.
Mental health service use was assessed by asking, “During the past 12 months, has [youth] received any psychological or mental health services or counseling?” Respondents who answered affirmatively were asked a follow-up question to determine whether the services had been through the school. The data did not allow us to determine whether youths receiving services in school were also receiving services outside of school. We included gender, race, ethnicity, and parental education as predisposing variables because these variables often serve as proxies for beliefs about mental health treatments. Language impairment was also considered a predisposing characteristic because lack of speaking ability may limit the perceived appropriateness of mental health services. An indicator of severe language impairment was created for youths who have a lot of trouble speaking clearly or who do not speak at all.
Enabling resources included income, health insurance status, case management, having a diagnostic medical evaluation in the past year, and parent and youth involvement in individualized education planning (IEP) meetings. Responses to a sequence of questions about insurance status were recoded into private insurance versus government or other insurance for analysis. Two dichotomous indicators asked about parent and youth attendance at the most recent IEP meeting.
Measures of need included parent-reported comorbid attention-deficit hyperactivity disorder (ADHD), social skills, and experiences with bullying. We included ADHD because it is a common comorbidity among youths with an autism-related disorder (
2). Unfortunately, the survey did not directly ask parents about other types of comorbidities. Social skills were measured with 11 items drawn from the Social Skills Rating System Parent Form (
11), with higher scale scores indicating greater skill. Bullying victimization was measured by collapsing three questions about whether the youth had been bullied, teased, or physically attacked at school into one response. Another question asked whether the youth had bullied others.
One logistic regression model examined use of mental health services among all youths with an autism-related disorder. A second logistic regression model examined the use of school-based mental health services by the subset of youths who had received any mental health services. Twenty multiply imputed data sets were created with sequential regression in IVEware to handle missing data (
12). All estimates are population estimates. Stata 11 was used to weight analyses and adjust variances to account for the sampling design and imputation.
Results
Most youths were male (85%), and the mean±SD age of the sample was 15.0±1.2. In addition, 65% of the sample was white, 22% African American, and 13% other or mixed race. Eleven percent of the sample self-identified as Hispanic. Overall, 46% of respondents reported that their child had received a mental health service in the past 12 months. Of those who had received any service, 49% had received it through the school or school district.
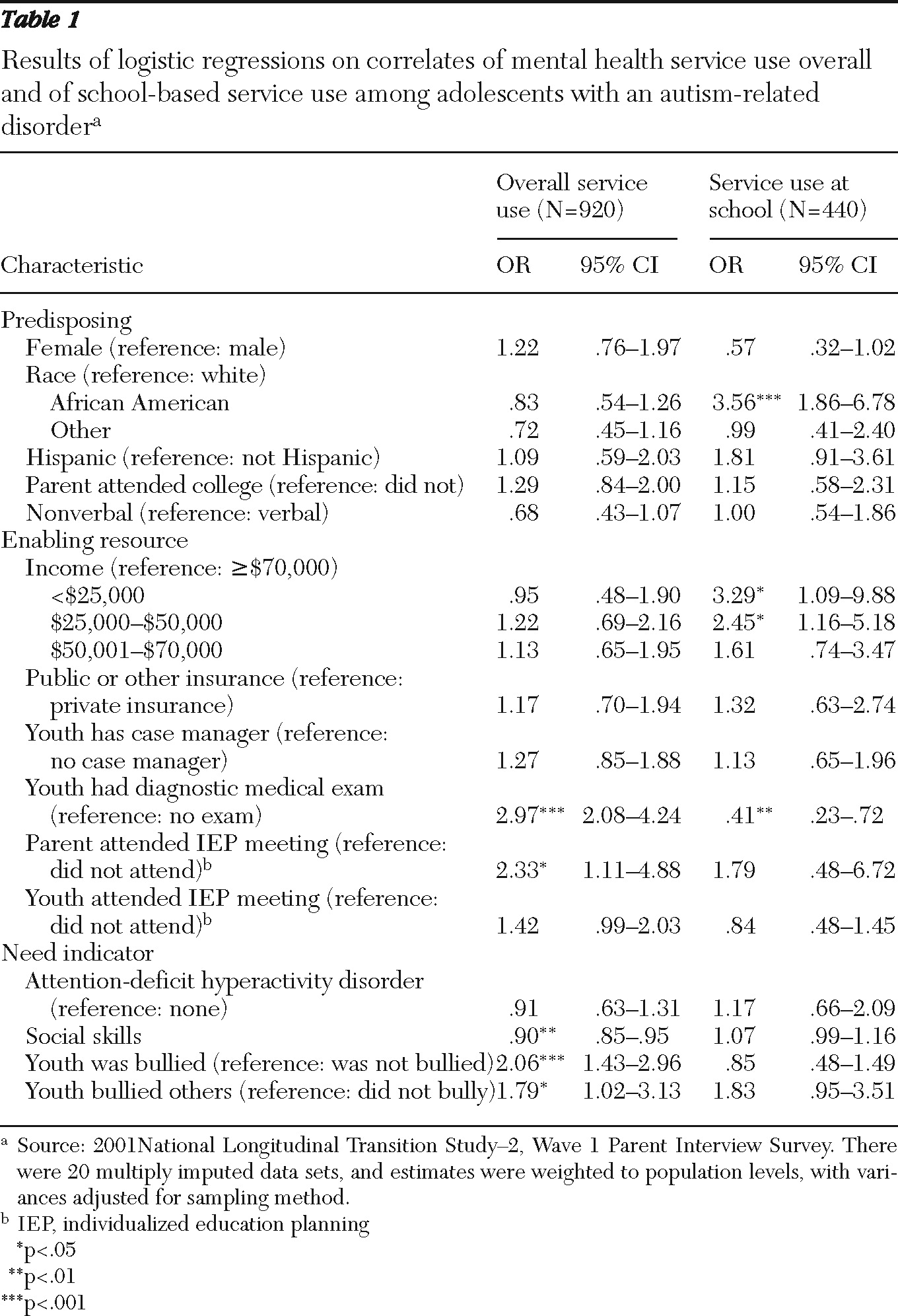
The sample's use of mental health counseling overall did not vary significantly by predisposing characteristics. African Americans had greater odds of receiving services at school. Several enabling resources were significant. Parent involvement in the IEP process was associated with use of mental health services overall but not with utilization of school-based services. Adolescents who had received a diagnostic medical exam in the past year were more likely than those who did not to receive services but were less likely to receive those services at school. Youths from households with incomes below $50,000 were more likely to receive services at school compared with youths from households with incomes over $70,000. Need characteristics of having lower social skills, experiencing bullying, and bullying others were associated with receiving services but were not associated with getting the services at school.
Discussion
Our study indicated that nearly half of youths with an autism-related disorder had accessed a mental health service in the previous year. Although no other national rates have been reported for youths with an autism-related disorder, these rates were higher than the 2001 National Survey of Children with Special Health Care Needs, where 25% of participants reported a need for mental health services and 82% of those accessed services (
13). Our study could not shed light on the exact reason the youths used services and the nature of the mental health services they received. More work is needed to better understand the types of treatments delivered to youths with an autism-related disorder in both school and community settings. Although applied behavior analysis is an evidence-based practice often recommended for this population, less is known about effective methods for treating comorbid mental health conditions of youths with an autism-related disorder. Adaptation of other evidence-based practices may be needed to address the full range of needs for which these youths seek treatment.
Our examination of the correlates of mental health service use overall found no differences by predisposing characteristic, including race or ethnicity; however, African-American youths were more likely to receive the services at school. Previous studies of adolescent mental health service use have found racial disparities in rates of outpatient mental health service use but no differences in the use of school-based mental health services (
14,
15). The fact that African-American youths who received services in our study were more likely to receive them at school supports these previous findings about the importance of the school in providing services to groups that are less likely to access community-based services.
A similar difference emerged in regard to enabling resources. Although there were no differences in overall service use by household income, youths from lower-income families were more likely to receive the services at school. Insurance status, however, was not associated with service use in either model. Having a diagnostic medical exam was positively associated with receiving mental health services overall, but youths who received services at school were less likely to have had a diagnostic medical exam. Our findings underscore the role of the school in providing mental health services to particular groups. Further research is needed to determine whether the type or quality of the services differs between settings.
Conclusions
Our study is the first to report on mental health service use in a nationally representative sample of youths with an autism-related disorder. We found relatively high rates of service use in this population compared with the overall group of youths with special health care needs, a finding that highlights the importance of considering the unique needs of youths with an autism-related disorder in the development of mental health interventions. Our findings also point to the important role of schools in providing access to mental health services, especially for underserved groups. Continued mental health support should be considered in transition planning to ensure that this population of youths does not lose needed services when exiting high school.
Acknowledgments and disclosures
This research was supported with funding from the National Institute of Mental Health (R01-MH086489-01 and T32-MH19960) and the Organization for Autism Research.
The authors report no competing interests.