Sleep problems are prevalent among psychiatric patients with common mood and anxiety disorders (
1,
2). Problematic sleep is associated with more severe medical and psychological conditions (
3) and greater health service utilization and associated costs in these populations (
4). However, the prevalence and implications of sleep problems for patients with serious mental illness are not as well known. An improved understanding of the prevalence, correlates, and implications of sleep disturbances for health care utilization in this patient population could provide useful guidance for design of services and targeted treatments.
In this study, we examined the prevalence and severity of psychiatrist-rated sleep problems in a large sample of psychiatric patients who were enrolled in Medicaid. We also explored associations between these problems and clinical factors, as well as the association of sleep problems with psychiatric hospitalizations and emergency department use. We hypothesized that patients with sleep problems would be more likely to have psychiatric hospitalizations and psychiatric emergency department visits than those without sleep problems and that use of these services would be more prevalent among patients with more severe sleep problems.
Methods
The sample consisted of 1,560 Medicaid patients of a randomly selected group of psychiatrists who were identified via the American Medical Association's Physician Masterfile of all physicians in the United States. Data were collected by mail from September to December 2006. Psychiatrists were excluded if they did not treat Medicaid patients in their last typical work week, were psychiatry residents, had undeliverable addresses, or had limited contact with patients. A total of 2,671 psychiatrists (62% of those approached) responded, of whom 857 (32%) met eligibility requirements. Each psychiatrist was asked to complete a questionnaire concerning the next two Medicaid patients that they saw during their last typical work week, after one of 21 randomly assigned start days and times. Psychiatrists were offered $75 compensation for completing the questionnaire. Data were available for 1,625 Medicaid patients reported on by the eligible psychiatrists. We excluded from this sample patients whose psychiatrists either reported not knowing whether they had sleep problems (N=11) or failed to provide sleep data (N=54), resulting in a final sample of 1,560 patients. The study procedures were approved by the institutional review board of the American Psychiatric Institute for Research and Education. More details on the design of the study are provided elsewhere (
5).
Psychiatrists were asked to provide information on the patients' demographic characteristics,
DSM-IV-TR diagnoses, prescribed medications, and the current severity of a number of psychiatric symptoms, including sleep problems. Response options were “none,” “mild,” “moderate,” “severe,” and “don't know.” [A sample of the instrument is available as a supplement to this report at
ps.psychiatryonline.org.]
The patients' health service utilization was measured by a series of items, including queries about psychiatric hospitalization and emergency department use. Psychiatrists recorded the number of days a patient was hospitalized and the number of emergency department visits that were a result of a patient's psychiatric illness since January 1, 2006. For this study, we examined the association of sleep problems with psychiatric hospitalizations of at least one day and with any use of emergency services.
Analyses were conducted in three stages. We first examined the prevalence and severity of sleep problems in our sample. Next, we explored the demographic and clinical correlates of sleep problems among the patients. For these analyses, a sleep score ranging from 0 (no sleep problem) to 3 (severe sleep problems) was computed on the basis of the psychiatrist ratings. We compared patients with different sleep scores in terms of demographic and clinical characteristics. Finally, we assessed the association of sleep problems with psychiatric hospitalization (any versus none) and emergency service use (any versus none) in binary logistic regression models, controlling for demographic and clinical characteristics. Estimates were weighted by the clinician's Medicaid caseload, as well as the number of psychiatrists treating Medicaid patients in each state.
Results
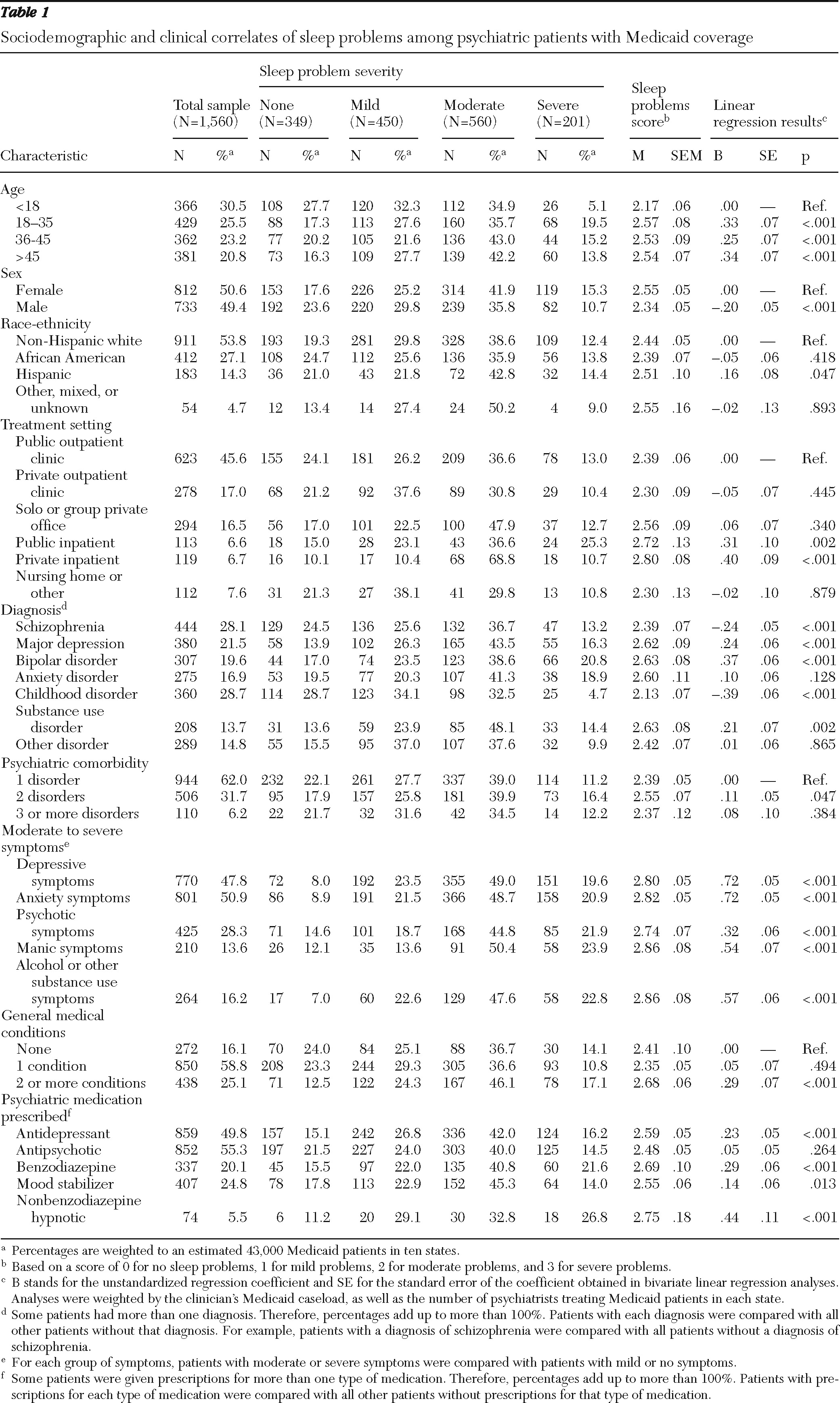
Patients' demographic and clinical characteristics are presented in
Table 1. A majority (56%) were under 36 years of age. Approximately half were male and half were white. Psychiatrists treated nearly half of these patients (46%) in public outpatient clinics; approximately one-third were treated in private outpatient clinics (17%) or solo or group private office settings (17%). Almost 30% of these patients had a diagnosis of schizophrenia, over 20% had a diagnosis of major depression, and close to 20% had bipolar disorder. Approximately 38% of patients had more than one psychiatric diagnosis, and almost 84% had at least one comorbid medical condition. The psychiatric symptoms rated most often by psychiatrists as “moderate” or “severe” were anxiety (51%), depressive symptoms (48%), and psychotic symptoms (28%). A total of 55% of patients received prescriptions for antipsychotics, 50% for antidepressants, 25% for mood stabilizers, 20% for benzodiazepines, and 6% for nonbenzodiazepine hypnotics.
Overall, 78% (N=1,211) of patients were rated by their psychiatrists as having some sleep problems. Approximately 29% (N=450) were rated as having mild, 36% (N=560) moderate, and 13% (N=201) severe sleep problems. The sleep problems were associated with a number of patient demographic and clinical characteristics as well as treatment setting characteristics. More severe sleep problems were found among patients 18 years old or older compared with younger patients; females compared with males; Hispanic patients compared with non-Hispanic whites; patients treated in inpatient settings compared with other settings; patients with mood and substance use disorders compared with patients without these disorders; patients with two psychiatric comorbid conditions compared with those with no comorbid conditions; patients with moderate to severe mood, anxiety, psychotic or substance use symptoms compared with those with no or mild symptoms; patients with more than one comorbid medical condition compared with no comorbid medical conditions; and patients with prescriptions for antidepressants, benzodiazepines, mood stabilizers, and nonbenzodiazepine hypnotics compared with those without prescriptions for these medications. Patients with schizophrenia and childhood disorders had less severe sleep problems compared with patients without these diagnoses (
Table 1).
In this sample 492 (28%) patients had at least one psychiatric hospitalization, and 560 (34%) patients visited an emergency department at least once in the period since January 1, 2006. In multivariate analyses, patients with sleep problems had greater odds of psychiatric hospitalization compared with those with no sleep problems (adjusted odds ratio [AOR]=1.51, 95% confidence interval [CI]=1.04–2.19 for mild versus no problems; AOR=1.98, CI=1.35–2.90 for moderate versus no problems, and AOR=1.68, CI=1.06–2.68 for severe versus no problems). [Supplemental Table 1 provides details on psychiatric hospitalization and is available at ps.psychiatryonline.org.] In addition, patients with sleep problems had greater odds of emergency service use compared with those with no sleep problems (AOR=1.29, CI=.91–1.83 for mild versus no problems; AOR=1.79, CI=1.26–2.55 for moderate versus no problems; and AOR=2.37, CI=1.52–3.70 for severe versus no problems). [Supplemental Table 2 provides details on use of emergency services; see
ps.psychiatryonline.org.]
Discussion
In this study, we examined the prevalence and correlates of sleep problems in a sample of psychiatric patients with Medicaid insurance and the association of sleep problems with psychiatric hospitalizations and emergency department use. The study had two main findings. First, four out of every five patients in this sample had some sleep problems, according to ratings by their psychiatrists. Furthermore, approximately half of patients were described as having either moderate or severe problems, suggesting that sleep problems were highly prevalent in this population.
To put these findings in perspective, epidemiological studies of sleep problems in the general population have indicated a self-reported prevalence of approximately 10% to 33%, depending on the definitions used for the sleep problems, with older adults having the highest prevalence (
6). Epidemiological studies of sleep problems in primary care settings report a prevalence of approximately 50% (
7). Our estimates of sleep problems are similar to previous reports for patients with depression, generalized anxiety disorder, panic disorder, and posttraumatic stress disorder, 70%–90% of whom present with sleep problems (
2). Even among patients with diagnoses of schizophrenia or childhood disorders in our sample—two diagnoses with fewer sleep problems—over 70% were rated as having some degree of sleep problems, and large proportions had moderate to severe problems (
Table 1).
The high prevalence of sleep problems in this patient population calls for better monitoring and management of these problems in various treatment settings. The use of standardized measures in routine practice settings may improve clinicians' ability to screen for and diagnose sleep disturbances and monitor treatment responses of patients treated for these complaints. A number of validated instruments are available for this purpose, including the Pittsburgh Sleep Quality Index (
8) and the Insomnia Severity Index (
9). These instruments are easily administered and can be used for patients with different psychiatric diagnoses.
Physicians most commonly rely on medications to address sleep problems of their patients (
10). Medication treatments can be effectively combined with various nonpharmacological interventions for insomnia (
7,
11,
12). These nonpharmacological interventions are based on generalizable behavioral principles and have been effectively used with patients who have sleep disorders that are associated with physical and more common psychiatric conditions. However, there is little research on the application of these interventions with patients with more severe mental disorders. Future research is required to assess the feasibility and effectiveness of these interventions in this patient population and especially the added benefits of combinations of these treatments with the common pharmacological interventions. Research also needs to explore strategies to most efficiently disseminate these nonpharmacological interventions in routine treatment settings.
The second noteworthy finding of this study is the significant association of sleep problems with psychiatric hospitalization and emergency department use for psychiatric reasons. Although this study did not examine the factors that could mediate this relationship, past research has found an association between sleep problems and suicidal ideation and behaviors (
13), which, in turn, are among the most common reasons for emergency department use and psychiatric hospitalization (
14,
15). This and other potential mechanisms linking sleep problems with emergency service use and psychiatric hospitalization need to be assessed in future studies using a longitudinal design.
The results of this study should be considered in the context of its limitations, including the cross-sectional design; the use of a global measure of sleep problems, which did not distinguish between different types of sleep problems; and reliance on psychiatrists' reports rather than objective measures of sleep. Furthermore, the sample was limited to Medicaid patients with serious mental disorders, who typically have fewer financial resources and may be especially prone to sleep problems and their adverse consequences.
Acknowledgments and disclosures
Dr. Spira's work was supported by a Mentored Research Scientist Development Award (1K01AG033195) from the National Institute on Aging. Dr. Mojtabai's work was in part supported by the Center of Mental Health Initiatives at the Department of Mental Health, Johns Hopkins School of Public Health.
The original study and support for Mr. Rae and Dr. West were funded by a grant from the American Psychiatric Foundation (APF). Although a consortium of industry supporters, including AstraZeneca, Bristol-Myers Squibb, Eli Lilly and Company, Forest, Janssen, Pfizer, Sanofi-Aventis and Wyeth, provided financial support to APF for this research, researchers had complete discretion and control over the design and conduct of this study and the analyses of the resulting database. Input or comments on the manuscript were neither solicited nor obtained from benefactors before the manuscript was submitted for consideration.