The few studies that have examined the effect of comorbid personality disorders on the clinical outcome of ECT had important methodological limitations. Among 13 studies reviewed by DeBattista and Mueller in 2001
(15), six were published prior to the advent of DSM-III
(16–
21). All six reports found that indicators of personality disturbance were negative predictors of ECT response, but the lack of standardized diagnostic and symptom assessments renders interpretation difficult. Two of the seven studies published after the introduction of DSM-III did not find an association between personality disorder and ECT outcome
(5,
9), although lack of statistical power because of the small number of subjects may have contributed to the negative findings. In contrast, three studies showed comorbid personality disorder to be associated with inferior outcomes after ECT, either in terms of more severe depressive symptoms, higher rates or rehospitalization, or poorer social functioning, based on assessment of these variables immediately after the completion of ECT or at 6-month to 1-year follow-up
(8,
22,
23). One of these studies found that patients with a cluster B personality disorder were especially likely to have poor outcome
(23). Two additional reports focused on borderline personality disorder. One found that borderline personality disorder dimensional scores predicted a poorer outcome immediately after ECT in 16 patients with major depression
(24). The second report consisted of a chart review of five patients with major depression and concluded that patients with comorbid borderline personality disorder evidenced only a slight response to ECT followed by a rapid relapse
(25). In summary, there is preliminary evidence that depressed patients with a personality disorder, especially borderline personality disorder, have a poorer outcome when treated with ECT.
We compared the acute outcome of ECT in patients with major depression who did or did not have a comorbid personality disorder. The study subjects were participants in a large prospective study involving standardized ECT administration and clinical assessments. We hypothesized that patients with personality disorders other than borderline personality disorder would respond more poorly than those with no personality disorder and that borderline personality disorder patients would show the least positive outcome.
Method
The study subjects consisted of 139 depressed patients who participated in a multisite study examining short-term ECT outcome and the efficacy of continuation pharmacotherapy in preventing relapse
(26). Only patients at the Western Psychiatric Institute and Clinic were included in the study group for this report. Patients provided written informed consent after all of the study procedures had been fully explained. Study methods have been described previously
(26–
29).
Patients referred for ECT were invited to participate if they met the Research Diagnostic Criteria
(30) for an episode of primary, unipolar depression and the DSM-III-R criteria for a major depressive episode on the basis of semistructured interviews with a supplemented Schedule for Affective Disorders and Schizophrenia
(31). Patients also had to receive a score of at least 20 on the 24-item Hamilton Depression Rating Scale
(32). Exclusion criteria were a history of schizophrenia, schizoaffective disorder, or other functional psychosis; a history of neurological injury or disorder (including dementing disorders); a history of substance abuse other than use of nicotine within the past year; and a course of ECT within the past 6 months. Of the 139 participants, 44 patients (31.7%) had psychotic features, 17 patients (12.2%) had comorbid dysthymia, and two patients (1.4%) had comorbid panic disorder.
DSM-III-R personality disorder symptoms were assessed with the Personality Disorder Examination
(33) or the Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II)
(34). Assessments were administered by trained, experienced raters. The first 68 patients were administered the Personality Disorder Examination before receiving ECT, and the remaining 71 patients were given the SCID-II after completion of ECT. On both instruments, personality disorder criteria are scored on a 3-point scale (0=absent, 1=probable, 2=definite). Subthreshold diagnoses were assigned if patients met one criterion less than required for a full diagnosis of a personality disorder; only the criteria that were definitely present (i.e., scored 2) were counted.
Given that two different interviews were used for the diagnosis of personality disorders and that the Personality Disorder Examination was administered before ECT and the SCID-II after completion of ECT, analyses were conducted to examine whether the different methods yielded different rates of personality disorders and personality disorder symptoms. We compared the interviews in the number of diagnoses of cluster A personality disorders (paranoid, schizoid, schizotypal), borderline personality disorder and other personality disorders in cluster B (antisocial, histrionic, narcissistic), and cluster C personality disorders (avoidant, dependent, obsessive-compulsive, passive-aggressive, and the provisional self-defeating personality disorder). Both threshold and subthreshold personality disorder diagnoses were considered. Chi-square tests comparing the interviews in rates of personality disorder diagnoses did not yield significant differences (cluster A personality disorders: Personality Disorder Examination=11.8%, SCID-II=11.3%, p=0.93; borderline personality disorder: Personality Disorder Examination=14.7%, SCID-II=14.1%, p=0.92; other cluster B personality disorders: Personality Disorder Examination=25.0%, SCID-II=26.8%, p=0.81; cluster C personality disorders: Personality Disorder Examination=41.2%, SCID-II=42.3%, p=0.90).
Second, we compared the dimensional scores for each of the personality disorders yielded by the Personality Disorder Examination and SCID-II. Dimensional scores were obtained by totaling the individual item scores for each personality disorder. The Personality Disorder Examination and SCID-II yielded remarkably similar dimensional scores across the majority of personality disorders, and visual inspection of histograms showed that the distribution of dimensional scores was very similar for the two interviews. However, t tests comparing the Personality Disorder Examination and SCID-II scores yielded a few significant differences: the Personality Disorder Examination produced higher dependent personality disorder scores (mean=4.41, SD=3.88, versus mean=2.89, SD=2.75) (p=0.009) and antisocial personality disorder scores (mean=0.66, SD=1.58, versus mean=0.06, SD=0.48) (p=0.003), whereas the SCID-II yielded higher self-defeating personality disorder scores (mean=2.73, SD=3.38, versus mean=1.75, SD=2.24) (p<0.05). To control for these differences, we standardized each of the dimensional personality disorder scores for both the Personality Disorder Examination and SCID-II, separately, and used these z scores in subsequent analyses.
In terms of the prevalence of threshold and subthreshold personality disorders, 20 patients (14.4%) met the criteria for borderline personality disorder, 42 patients (30.2%) met the criteria for a personality disorder other than borderline personality disorder, and 77 patients (55.4%) did not meet the criteria for any personality disorder. The prevalence of individual personality disorders other than borderline personality disorder was as follows: avoidant, 17.3% (N=24); dependent, 7.9% (N=11); obsessive-compulsive, 7.9% (N=11); histrionic, 7.9% (N=11); personality disorder not otherwise specified, 7.2% (N=10); self-defeating, 6.5% (N=9); paranoid, 5.8% (N=8); schizoid, 3.6% (N=5); narcissistic, 3.6% (N=5); schizotypal, 2.2% (N=3); passive-aggressive, 2.2% (N=3); and antisocial, 0.7% (N=1).
Patients were administered the 24-item Hamilton depression scale
(32) at three time points: before starting ECT, within 3 days of completing the acute course of ECT, and within 4–8 days of completing ECT. To ensure adequate interrater reliability, all raters participated in regular training sessions. The interviews were videotaped and rerated by an off-site rater who was blind to the patients’ diagnoses. Intraclass correlation coefficients for the on-site and off-site Hamilton depression scale ratings exceeded 0.95. Before treatment, resistance to antidepressant medication was classified with the Antidepressant Treatment History Form
(27,
28). The measure takes into account the duration, oral dose, blood levels, compliance rate, and clinical outcome for each medication trial patients received during the index episode. Patients’ physical status was assessed with a modified version of the Cumulative Illness Rating Scale for Geriatrics
(35). Medical burden was rated for each of 14 organ systems on a 5-point scale ranging from 0 (no problem) to 4 (extremely severe problems).
All psychotropic medications (with the exception of up to 3 mg/day of lorazepam) were tapered before ECT. Patients received either right unilateral ECT with the d’Elia placement or bilateral ECT with the bifrontotemporal placement. The titration procedure was used at the first treatment to quantify seizure threshold
(36). Treatment was started with suprathreshold right unilateral ECT unless the patient had not responded to this modality in the past or the patient’s depression was severe enough that the patient’s psychiatrist requested bilateral ECT. For right unilateral treatment, stimulus intensity was increased to a minimum of 150% above the empirically determined seizure threshold. Treatment was switched to bilateral ECT if the patient did not show significant improvement after at least five suprathreshold right unilateral treatments. For bilateral ECT, stimulus intensity was also set at 150% above the threshold.
There was no preset maximum number of treatments for either modality. All patients were encouraged to continue ECT until they had full remission (i.e., had experienced complete or almost complete resolution of their depressive symptoms) or until they had been treated with at least 8–12 bilateral treatments and showed no further improvement during the past 2–3 treatments. Some patients (or their attending psychiatrists) declined to switch treatment from unilateral to bilateral ECT and/or decided to discontinue ECT before receiving the recommended complete course.
Pretreatment characteristics and response to ECT were examined for borderline personality disorder patients, patients with personality disorders other than borderline personality disorder, and patients with no personality disorder. We used chi-square tests for discrete variables and univariate analyses of variance (ANOVAs) for continuous variables to compare the groups in demographic and clinical characteristics and in ECT treatment parameters. Significant effects in the chi-square analyses were followed by additive partitioning, a procedure that permits the partitioning of the contingency table into independent subtables that can then be analyzed separately
(37). For two-by-three contingency tables, this procedure allows the comparison of two subtables. Because our focus was on examining the characteristics of the borderline personality disorder versus the no borderline personality disorder groups, we chose the following comparisons a priori: 1) the group with no personality disorder versus the group with personality disorders other than borderline personality disorder and 2) the groups with no personality disorder and with personality disorders other than borderline personality disorder combined versus the group with borderline personality disorder. Significant ANOVA results were followed by post hoc tests using Tukey’s honestly significant difference procedure.
Group differences in symptomatic improvement after ECT were tested with analyses of covariance (ANCOVAs). The post-ECT Hamilton depression scale score served as the dependent variable and the pre-ECT Hamilton depression scale score as the covariate. Significant ANCOVA results were followed by Helmert contrasts with the following a priori comparisons: 1) the group with no personality disorder versus the group with personality disorders other than borderline personality disorder and 2) the groups with no personality disorder and with personality disorders other than borderline personality disorder combined versus the groups with borderline personality disorder. In addition, consistent with our previous work
(27–
29), we classified patients with post-ECT Hamilton depression scale scores of 10 or less as having achieved remission and compared the remission rates of the three groups using chi-square analyses. Significant results were again followed by additive partitioning by using the following a priori chosen comparisons: 1) the group with no personality disorder versus the group with personality disorders other than borderline personality disorder and 2) the groups with no personality disorder and with personality disorders other than borderline personality disorder combined versus the group with borderline personality disorder. To examine whether the proposed relationship between personality disorders and ECT outcome could be accounted for by group differences in baseline features, we conducted a series of multiple regression analyses using as predictor variables those characteristics that differentiated the three study groups before ECT.
The first set of analyses focused on the effect of categorical personality disorder diagnoses on response to ECT. Further analyses were conducted to examine the predictive effects of standardized dimensional scores obtained from the Personality Disorder Examination and SCID-II. We constructed five dimensional scores based on the criteria for 1) borderline personality disorder, 2) cluster A personality disorders, 3) cluster B personality disorders (including borderline personality disorder), 4) cluster C personality disorders, and 5) all personality disorders, including borderline personality disorder and the provisional self-defeating personality disorder (total personality disorder score). To determine the predictive value of these dimensional scores, multiple regression analyses were conducted, with post-ECT Hamilton depression scale scores as the dependent variable and pre-ECT Hamilton depression scale and dimensional personality disorder scores as predictor variables.
Twenty-four patients (17.3%) did not have a 4–8-day post-ECT Hamilton depression scale assessment. There was no statistical difference in the proportion of missed final assessments across the study groups (χ2=1.33, df=2, p=0.52).
Results
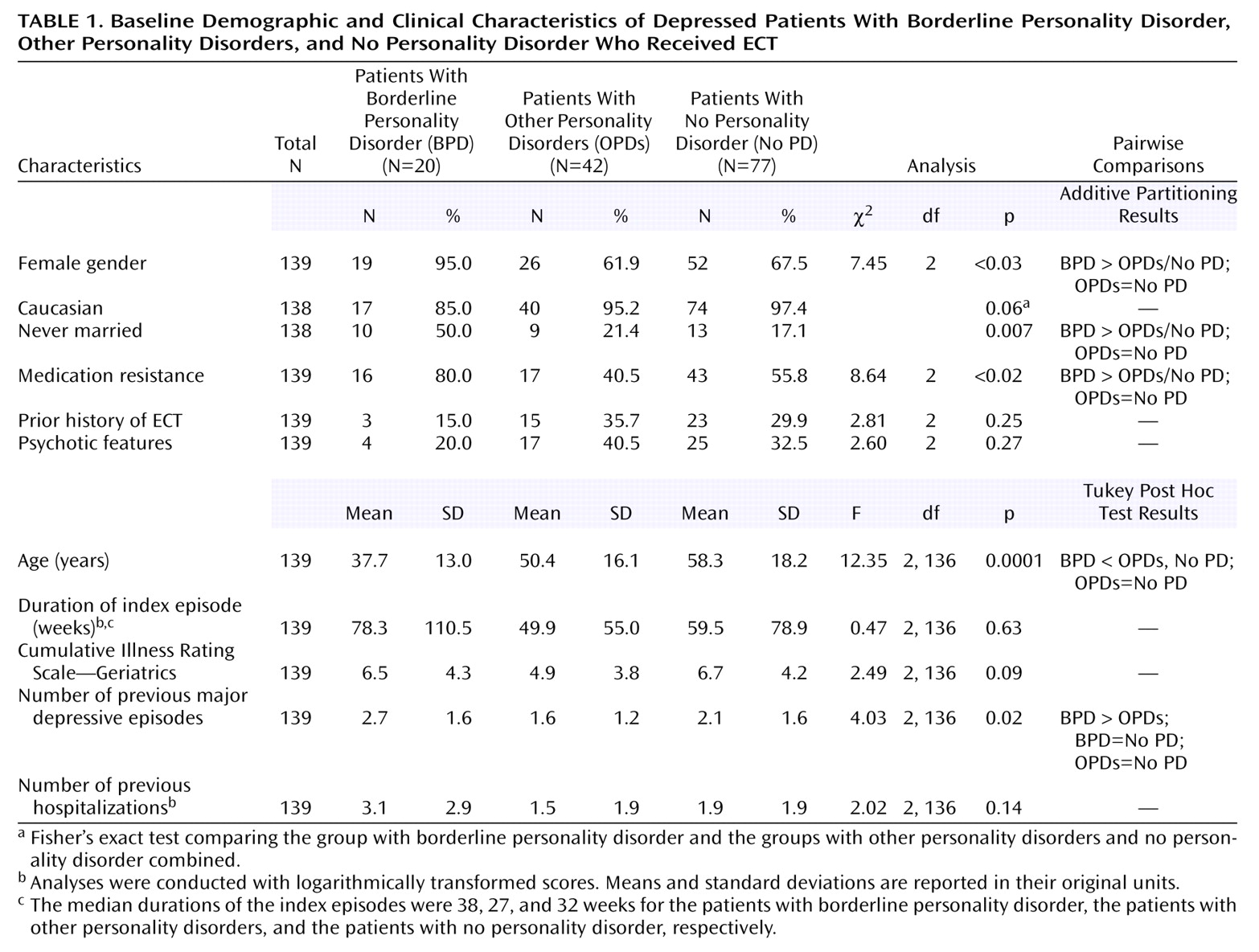
Baseline demographic and clinical characteristics of the three study groups are presented in
Table 1. Compared to all other patients, the borderline personality disorder patients were younger and more likely to be female, to never have been married, and to have medication-resistant depression. Compared to the patients with other personality disorders, the borderline personality disorder patients had more prior major depressive episodes. The patients with other personality disorders did not differ on any variable from the patients with no personality disorder.
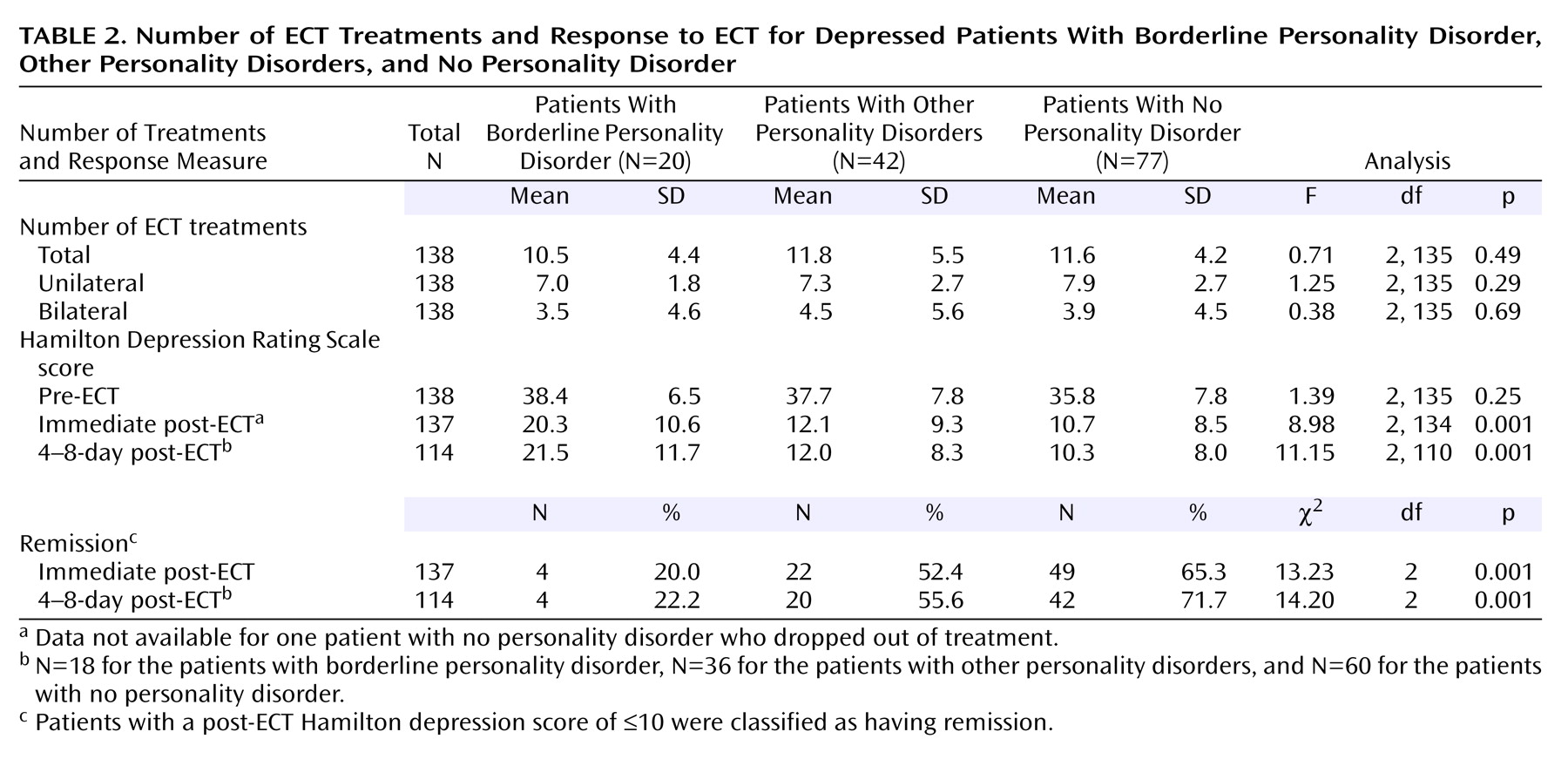
Table 2 presents the number of ECT treatments, pre-ECT Hamilton depression scale scores, and ECT remission rates for the three study groups. The three groups did not differ significantly in the total number of treatments, number of unilateral or bilateral treatments, or pre-ECT Hamilton depression scale scores. However, ANCOVAs with post-ECT Hamilton depression scale scores as the dependent variable and pre-ECT Hamilton depression scale scores as the covariate yielded significant effects for group, for both the immediate post-ECT and 4–8-day post-ECT scores. Post hoc contrasts showed that the borderline personality disorder group had higher post-ECT Hamilton depression scale scores than the two comparison groups combined (p<0.001, Helmert contrasts, for immediate and 4–8-day post-ECT Hamilton depression scale scores). Post-ECT Hamilton depression scale scores for the patients with personality disorders other than borderline personality disorder and for the patients with no personality disorder did not differ (p=0.39 and p=0.36, Helmert contrasts, for immediate and 4–8-day post-ECT Hamilton depression scale scores, respectively). Analyses examining outcome based on remission status resulted in similar findings: the borderline personality disorder patients were more likely to be classified as not having achieved remission than the patients in the two comparison groups combined (χ
2=11.63, df=1, p=0.001, and χ
2=11.16, df=1, p=0.001, for immediate and 4–8-day post-ECT remission status, respectively), whereas the group with other personality disorders and the group with no personality disorder did not differ in remission status (χ
2=1.97, df=1, p=0.18, and χ
2=1.93, df=1, p=0.18, for immediate and 4–8-day post-ECT remission status, respectively).
To examine the effects of the different axis II diagnostic methods, we conducted two ANCOVAs with type of interview (Personality Disorder Examination versus SCID-II) and diagnostic status as the between-subjects factors. The results showed main effects for group (p<0.001) and interview (p<0.001) and a group-by-interview interaction (p=0.06 and p<0.04), indicating that the borderline personality disorder patients whose diagnosis was made with the Personality Disorder Examination had lower post-ECT Hamilton depression scale scores than those whose diagnosis was made with the SCID-II. However, these results were due to the fact that three of the four borderline personality disorder patients with remission were assessed with the Personality Disorder Examination. Thus, the small cell sizes make these findings difficult to interpret. Moreover, given that the main effects for borderline personality disorder remained significant after adjustment for the type of interview and given that no ascertainment effect was found for other personality disorder diagnoses, it is unlikely that our findings are attributable to the effects of the diagnostic methods.
Additional regression analyses were conducted to test whether the relationship between borderline personality disorder and response to ECT was attributable to group differences in baseline features. We first examined the predictive power of medication resistance, age, marital status, and number of previous depressive episodes separately, without controlling for personality disorder status. We then conducted a second set of analyses that included any significant predictor variables as well as personality disorder diagnostic status. The relationship between medication resistance and higher Hamilton depression scale scores 4–8 days after ECT approached significance (R2=0.03, F change=2.87, p=0.09, β=0.16, t=1.69, p=0.09), but the relationship between medication resistance and Hamilton depression scale scores immediately after ECT was not significant (R2=0.02, F change=2.40, p=0.12, β=0.13, t=1.56, p=0.12). Younger age emerged as a predictor of negative response at both assessment points (immediately post-ECT: R2=0.08, F change=11.06, p=0.001, β=0.28, t=3.33, p=0.001; 4–8 days post-ECT: R2=0.08, F change=9.20, p=0.003, β=0.28, t=3.03, p=0.003). Separate analyses that included marital status (married versus separated, divorced, or widowed) and number of depressive episodes did not yield significant effects (marital status: p=0.24 and p=0.48; number of depressive episodes: p=0.66 and p=0.82). Two additional analyses were conducted to examine the predictive power of diagnostic status with adjustment for effects of both medication resistance and age. With diagnostic status entered as the third predictor, only the effects of diagnostic category remained significant (immediate post-ECT Hamilton depression scale scores: R2=0.05, F change=7.21, p=0.008, β=0.24, t=2.69, p=0.008; 4–8-day post-ECT Hamilton depression scale scores: R2=0.08, F change=11.00, p=0.001, β=0.32, t=3.32, p=0.001).
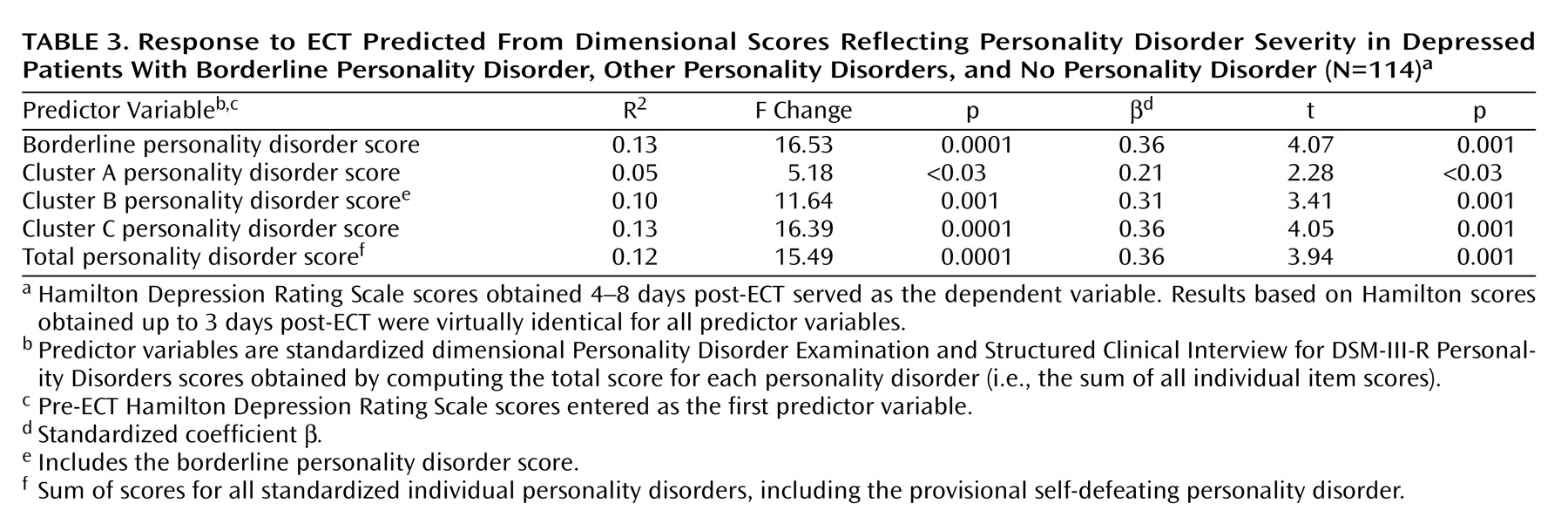
Table 3 presents the results of the regression analyses that used the personality disorder dimensional scores to predict 4–8-day post-ECT Hamilton depression scale scores. Each of the dimensional scores was associated with poorer outcome, accounting for 5%–13% of the variance in post-ECT Hamilton depression scale scores. We did not formally compare the relative predictive power of the various personality disorder scores, but inspection of the test values suggested that the borderline personality disorder dimensional score alone was as potent a predictor of outcome as any of the other dimensional personality disorder scores. Analyses predicting immediate post-ECT outcomes yielded similar results.
Discussion
This report describes a methodologically rigorous effort to test the effect of comorbid personality disorders on the response to acute ECT. Advantages over previous studies include the larger number of subjects, the use of a standardized ECT protocol, the availability of meaningful comparison groups, and the standardized assessment of axis I and II diagnoses and treatment outcome.
Consistent with our hypothesis, the depressed patients with comorbid borderline personality disorder responded more poorly to ECT than the combined group of depressed patients with other personality disorders and depressed patients with no personality disorder. Inspection of Hamilton depression scale scores and remission rates further indicates that these findings are of clinical and not merely statistical significance. Although borderline personality disorder patients’ scores on the 24-item Hamilton depression scale decreased from an average of 38 to 20, they still remained in the moderate to severe range post-ECT. Only 22% of borderline personality disorder patients met the criteria for remission up to 8 days after ECT, compared to 56% and 70% of the patients with other personality disorders and the patients with no personality disorder, respectively. Relapse rates as high as 84% 6 months after ECT without continuation therapy have been reported
(26), suggesting that the prognosis of those borderline personality disorder patients who did respond to ECT is guarded in the absence of additional intervention. Contrary to our predictions, the patients with personality disorders other than borderline personality disorder responded as well to ECT as those with no personality disorder.
We cannot offer a definitive explanation for the present findings, though several hypotheses warrant attention. The borderline personality disorder patients were significantly more likely to be classified as having medication-resistant depression (i.e., to not have responded to at least one antidepressant medication trial before treatment with ECT), and previous findings in a subgroup of the patients included in this study showed medication resistance to be negatively related to acute response to ECT
(28). In a follow-up report, patients age 59 years and younger responded more poorly than patients age 60–74 years, but these results were explained by the younger patients’ greater likelihood of being classified as having medication-resistant depression
(29). In the present study, neither the effects of medication resistance nor younger age remained significant once the presence of borderline personality disorder was added as a predictor variable. Relative to the comparison groups, the borderline personality disorder patients had experienced a larger number of major depressive episodes and were less likely to have ever been married, but neither variable was associated with outcome. The borderline personality disorder patients were also more likely to be female. We were not able to examine the potential effects of gender differences, given the small number of male borderline personality disorder patients, but there are no theoretical or empirical data linking gender to the effects of ECT. Taken together, none of the variables that differentiated the borderline personality disorder group from the two comparison groups explained the borderline personality disorder patients’ poorer acute response to ECT. Granted, given the data analytic strategies used, the nature and size of the study group, and the method for assessing treatment response, we cannot entirely rule out the possibility that the borderline personality disorder patients’ outcome may be caused by variables other than borderline personality disorder (e.g., medication resistance, axis I or II comorbidity). With this ambiguity in mind, the presence of borderline personality disorder still offers the most parsimonious explanation for our findings.
There is some evidence that the borderline personality disorder patients’ differential response may be due to differences in the type of depression associated with borderline personality disorder, compared to that occurring in the context of pure axis I depression or personality disorders other than borderline personality disorder. Delineating the boundaries between borderline personality disorder and depression is important because it has implications for treatment. However, research on this topic has been complicated by the diagnostic overlap between the two disorders: four of the borderline personality disorder criteria in DSM-III, DSM-III-R, and DSM-IV capture symptoms that can easily be taken to reflect axis I depression (i.e., chronic suicidality and repeated suicide attempts, affective instability, intense anger, and chronic emptiness or boredom). Nonetheless, studies indicate that the depression of borderline personality disorder patients differs phenomenologically from that experienced by patients with axis I depression that occurs either alone or in combination with personality disorders other than borderline personality disorder
(38). There is further evidence that borderline personality disorder and depression are characterized by different biological markers and a differential response to pharmacological agents, suggesting that these disorders may also respond differently to somatic treatments other than pharmacotherapy
(38,
39). Taken together, the current data suggest that borderline personality disorder and depression share both similarities and differences in their phenomenology, biology, pathogenesis, and symptom course
(38,
39). It is conceivable that any of the identified difference variables, either alone or in combination, are implicated in borderline personality disorder patients’ relative failure to respond to ECT.
Several limitations of this study need to be acknowledged. In approximately one-half of the study subjects, personality disorder symptoms were diagnosed with the Personality Disorder Examination before ECT, and symptoms in the remaining subjects were diagnosed with the SCID-II after treatment with ECT. However, we found little evidence suggesting that our primary results are attributable to an ascertainment bias. There is some suggestion that patients with personality disorders respond as well as those without a personality disorder immediately after ECT but are more likely to relapse in the year following ECT
(8,
23). Whether patients with personality disorders other than borderline personality disorder assessed over longer-term follow-up are more likely to relapse than patients with no personality disorders cannot be addressed with the present data. Finally, our assessment of treatment outcome was limited to the severity of depression, which did not allow us to examine the potentially differential response of other relevant symptoms (i.e., anger and irritability, general anxiety, interpersonal functioning) across groups.
In summary, our findings suggest that the diagnosis of borderline personality disorder (at either the threshold or subthreshold level) is a predictor of poor acute response to ECT, whereas the presence of personality disorders other than borderline personality disorder (at either the threshold or subthreshold level) does not have an effect on the immediate response to ECT. In practical terms, dimensional scores reflecting the severity of borderline personality disorder symptoms alone were as useful in predicting acute outcome as were dimensional scores capturing the severity of clusters A, B, and C personality disorder symptoms or all personality disorder symptoms taken together. The present results and other data suggest that the majority of depressed patients with comorbid borderline personality disorder are likely to be classified as having depression that is resistant to antidepressant treatment. Because ECT is considered one of the treatments of choice for treatment-resistant depression
(14), many depressed patients with comorbid borderline personality disorder may be considered for treatment with ECT. Thus, our findings suggesting that borderline personality disorder patients may not respond adequately to ECT have potentially significant implications for the selection of candidates for ECT.