Research on the course of alcohol use disorders has shown gender differences that investigators have labeled the "telescoping" effect (
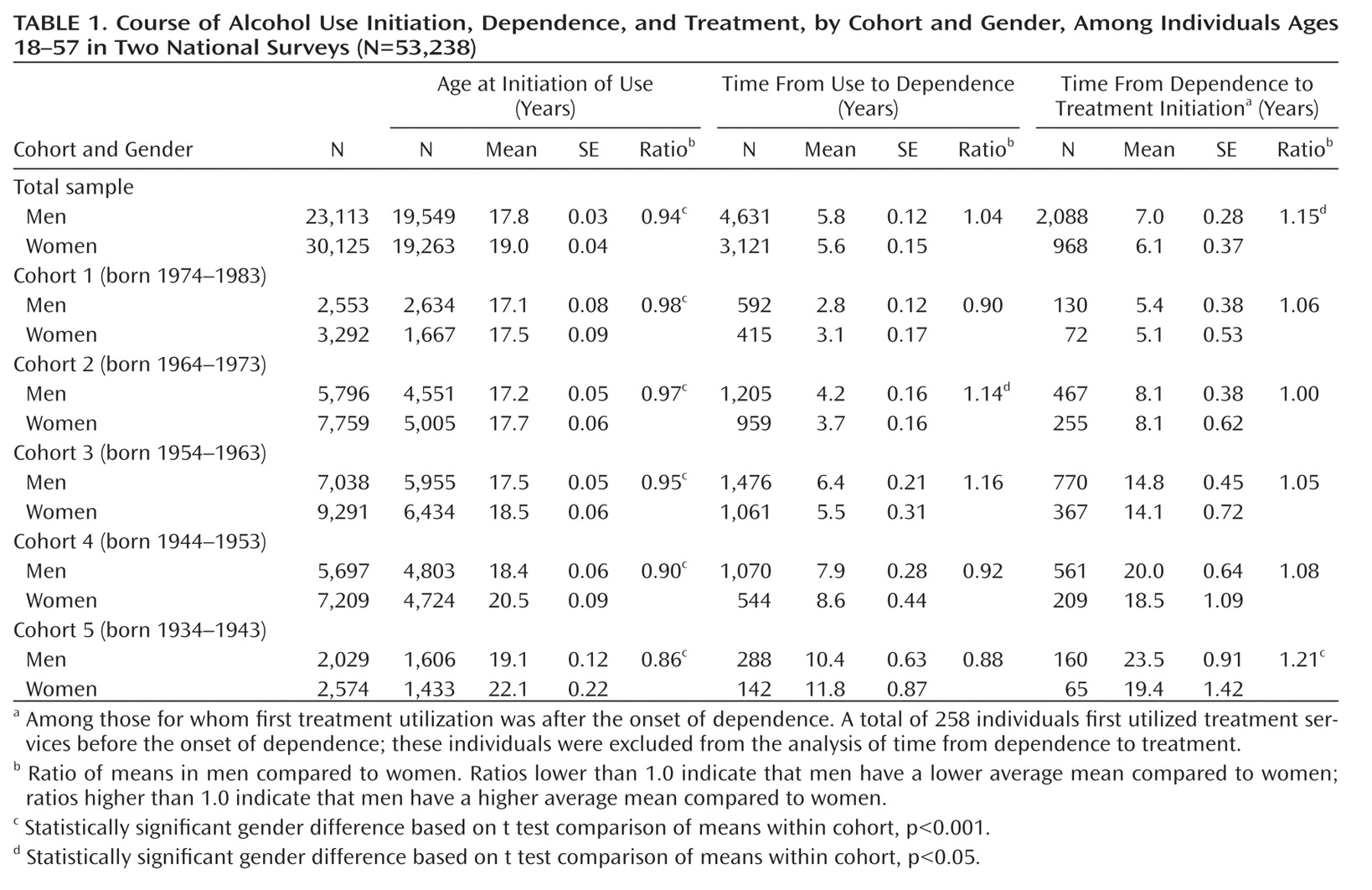
1). Telescoping has been reported in several components of the alcohol dependence course, beginning with initiation of alcohol use and continuing with subsequent landmark alcohol-related events, such as onset of dependence and initiation of treatment among those with dependence. In clinical samples, women have been found to initiate drinking later than men (
2). After drinking initiation, however, women progressed faster to alcohol dependence, and among those who became dependent, women progressed faster to treatment (
3–
6). The course of alcohol disorders is thus considered to be compressed, or telescoped, in women compared to men. Telescoping research has focused on individuals in treatment for alcohol disorders. Whether telescoping occurs in the larger population remains unknown.
Several time trends suggest that the telescoping phenomenon needs reexamination. First, many studies indicate that among more recent birth cohorts, regardless of gender, alcohol use disorders have become more common and start at an earlier age (
2,
7–
9). Furthermore, gender differences have diminished in several alcohol-related phenomena, including the prevalence of early drinking (
7,
8), heavy drinking (
9–
11), and alcohol use disorders (
12–
15). Traditionally, men have higher rates of all these phenomena (
16). However, in younger cohorts, prevalences are increasing among women while remaining stable or even decreasing slightly among men (
12). These changes over time suggest that even if telescoping of the course of alcohol use disorders existed in the general population, it may no longer occur in more recent birth cohorts. However, changes between birth cohorts in the main components of telescoping have never been tested directly. If evidence shows that the timing of major components of telescoping is becoming more similar between men and women in more recent birth cohorts, it could challenge commonly held clinical conceptions about gender differences in alcohol use disorders and signal the need to increase clinical awareness of the importance of screening, assessment, and interventions for alcohol use disorders in younger women.
To provide recent and representative information on telescoping in alcohol use disorders, we combined information from two U.S. national surveys conducted with identical measures 10 years apart. We had three aims in this study. The first was to determine whether a telescoping effect is present in the general population—that is, a later age at drinking initiation in women than men but shorter times from use to dependence and from dependence to treatment. The second aim was to test the hypothesis that gender differences in the overall rate of alcohol use, dependence, and treatment utilization are diminished in more recent cohorts. Our third aim was to test the hypothesis that in more recent cohorts, gender differences are diminished in age at drinking initiation, time from drinking initiation to dependence, and time from dependence to treatment initiation.
Method
Sources of Data
Data were drawn from two cross-sectional surveys: the National Longitudinal Alcohol Epidemiologic Survey (NLAES, 1991–1992) (
17) and the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC, 2001–2002) (
16). Both surveys were sponsored by the National Institute on Alcohol Abuse and Alcoholism, with fieldwork conducted by the U.S. Census Bureau. Interviews, which included households and group quarters, were conducted face-to-face by experienced lay interviewers. Both surveys featured a complex multistage design, which has been described in detail elsewhere (
17). The overall response rate was 81% for the NESARC and 90% for the NLAES. There was no overlap in the individuals included in the two surveys.
Similarities in design and measurement in the NESARC and the NLAES allowed pooling of the data to maximize the information available for each birth cohort. Consistent with other studies of cohort effects in these data (
13,
18), individuals older than age 57 were not included to minimize the possibility of alcohol-associated mortality effects. Confounding of cohort composition due to in-migration was minimized by limiting the sample to those born in the United States. The total combined sample was 53,238.
Cohorts were categorized in 10-year groupings: cohort 1, born 1974–1983 (N=5,845); cohort 2, born 1964–1973 (N=13,555); cohort 3, born 1954–1963 (N=16,329); cohort 4, born 1944–1953 (N=12,906); and cohort 5, born 1934–1943 (N=4,603). Groups were defined to be consistent with other cohort analyses of these data (
12,
13,
18); sensitivity analyses using 5-year age groups did not yield appreciably different results.
Two time points are available for cohorts 2, 3, and 4: those who were 18–27 years old in the NLAES were 28–37 at the time of the NESARC (cohort 2); those who were 28–37 years old in the NLAES were 38–47 at the time of the NESARC (cohort 3); and those who were 38–47 years old in the NLAES were 48–57 years old in the NESARC (cohort 4). We have one time point measurement for the youngest and oldest cohorts (cohort 1 was 18–27 years old in the NESARC, and cohort 5 was 48–57 years old in the NLAES). For cohorts with two time points, data were pooled; survey year was adjusted in all models.
Measures
Individuals were considered alcohol users if they had ever consumed >12 drinks, consistent with the NLAES definition of alcohol users. Interviews were conducted using the Alcohol Use Disorders and Associated Disabilities Interview Schedule–IV (AUDADIS-IV) (
19–
21). The AUDADIS-IV is a structured interview developed to advance measurement of substance use and mental disorders in large-scale surveys. Diagnoses were established explicitly following DSM-IV, including three or more of seven criteria clustering in a 1-year period. The good to excellent reliability and validity of alcohol diagnoses have been documented (
20). Three outcome measures were tested: age at drinking initiation, time from drinking initiation to onset of dependence, and time from dependence onset to treatment initiation.
Statistical Analysis
Statistical analysis was conducted by first pooling data from the NLAES and the NESARC and combining complex sampling weights from both surveys using statistical procedures that simultaneously adjust for clustering by sampling stratum and primary sampling unit across data sets. The SUDAAN software package (Research Triangle Institute, Research Triangle Park, N.C., 2004) was used to adjust for the complex sample designs. The analytic plan proceeded in three steps.
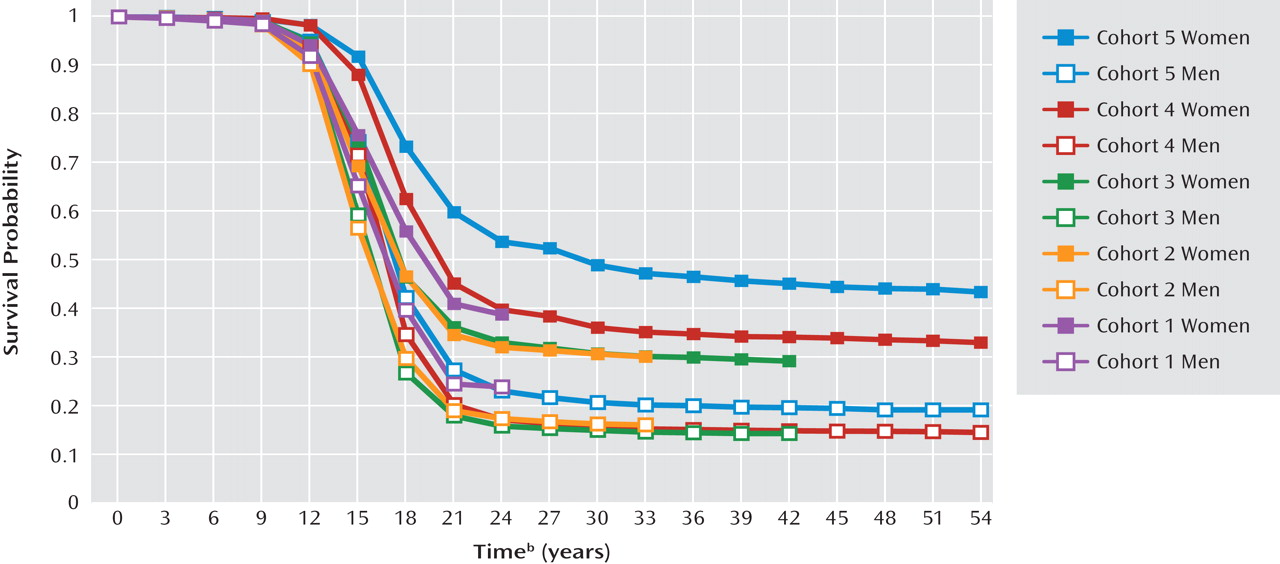
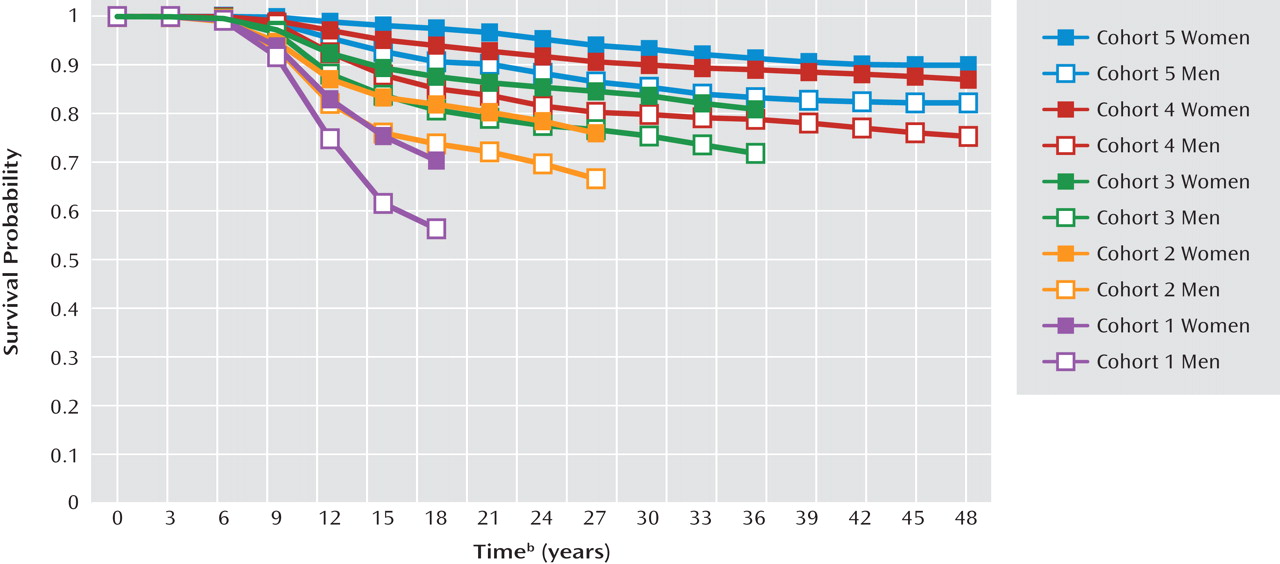
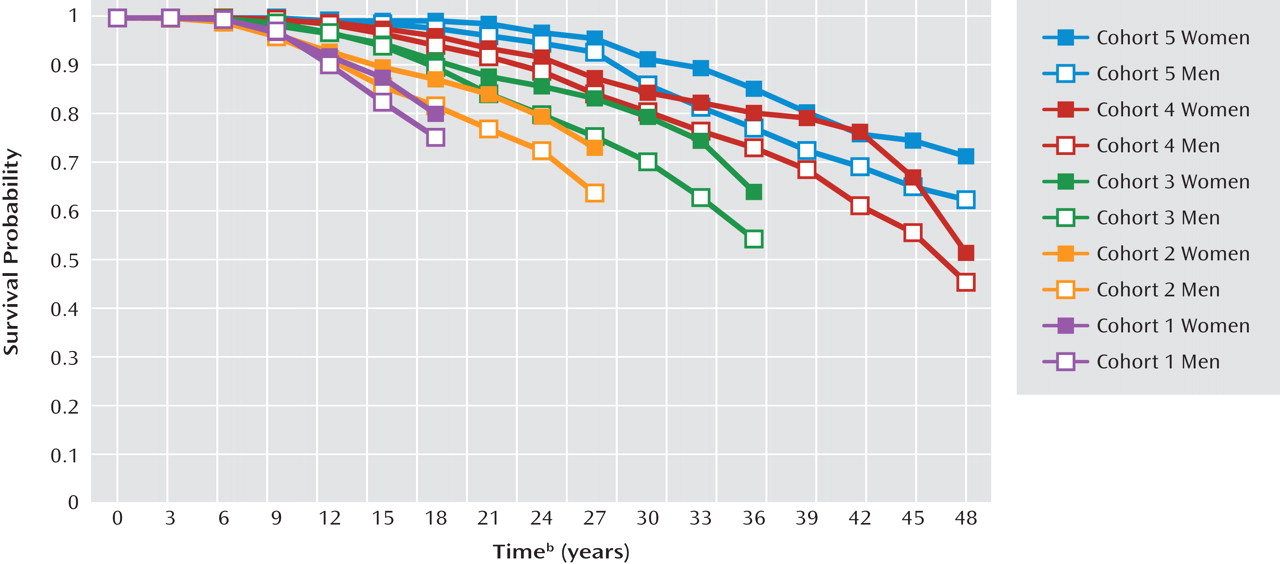
To investigate whether a telescoping effect exists in the general population, we first conducted a bivariate analysis of the three telescoping components by examining mean values stratified by cohort and gender; differences between men and women within cohorts were tested with t tests. These results can be misleading because mean age and duration increase by cohort (older individuals have had more time in which to have the disorder). Thus, our second step was to use standard life table analysis of the three telescoping components for bivariate analysis. Survival probabilities describe the probability of an outcome at any time t among individuals without the outcome at time t–1. When age at initiation of alcohol use was considered as an outcome, individuals were assumed to be at risk beginning at age 5, the minimum age allowed in the survey for reporting alcohol consumption. When time from use to dependence and time from dependence to treatment were considered as the outcome, individuals were assumed to be at risk from the age at initiation of alcohol use and the age at onset of dependence, respectively. Differences in survival curves were tested with the log-rank test for equality across strata.
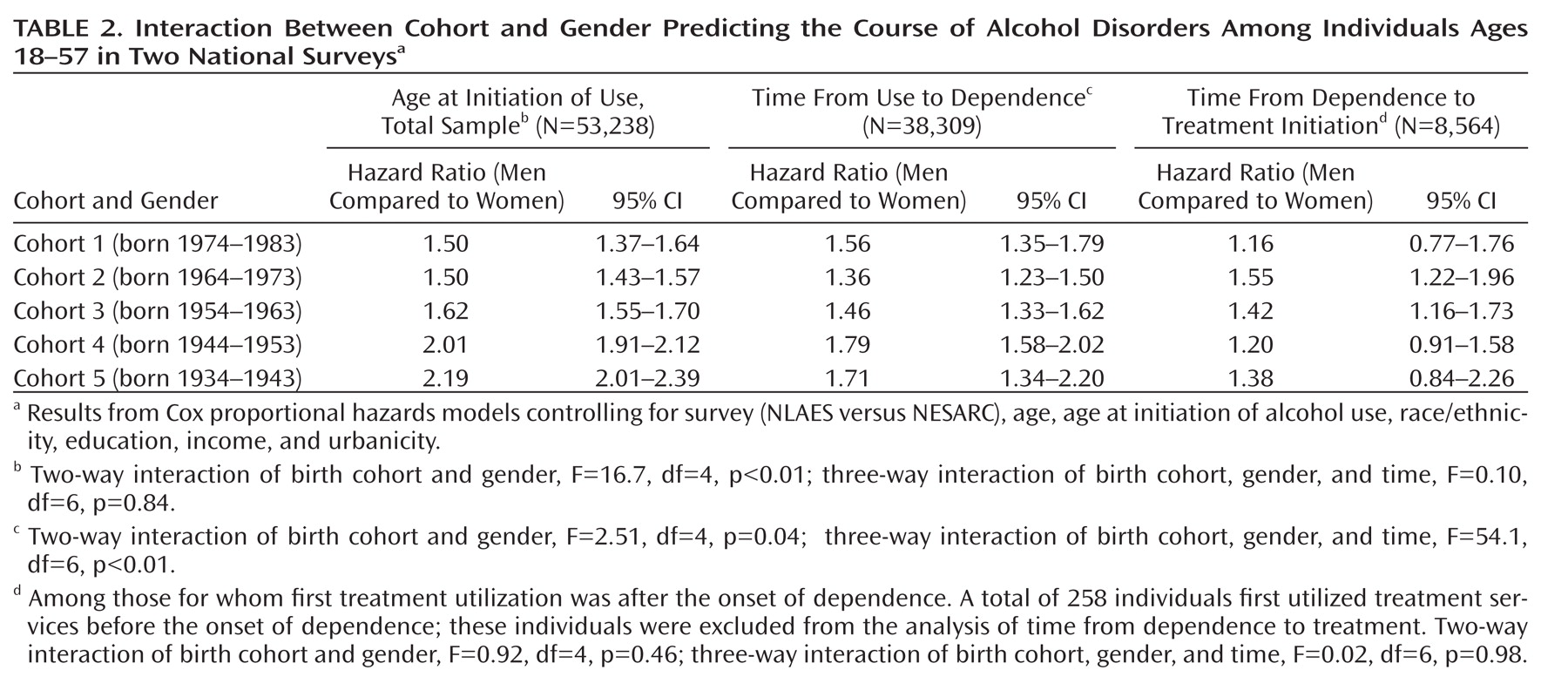
To investigate whether gender differences in overall hazard are diminishing by cohort, we used Cox proportional hazards models to examine evidence for cohort-by-gender interactions in the hazards of the three telescoping components: alcohol use (person-time, the number of years between age 5 and the age when alcohol use was initiated), dependence (person-time, the number of years between initiation of alcohol use and age at onset of dependence), and time to treatment initiation (person-time, the number of years between age at onset of dependence and first engagement with treatment). We first present gender-specific overall hazard ratios within each birth cohort. Cohort-by-gender interactions test whether the overall hazard of the outcome has converged in more recent cohorts.
To assess whether gender differences in the timing of events have diminished in more recent cohorts, we used a Cox proportional hazards model to examine evidence for cohort-by-gender-by-time to event interactions.
Individuals who did not develop the outcomes of interest were censored at current age. Control variables in all models included survey, race/ethnicity, income, education, and urbanicity. Age was evaluated as a potential confounder but not retained in final models because it was not significantly associated with the outcomes. Age at initiation of alcohol use was included in all models for which alcohol use was not the outcome, as it is related to both alcohol dependence and treatment utilization. Birth cohort was modeled as a five-level categorical variable to allow for nonlinear variation.
Discussion
In this study we sought to examine evidence for gender differences in the course of alcohol dependence—the telescoping effect—in the general population and evidence for cohort effects on gender differences. We highlight three major findings from these analyses.
First, we found that the full telescoping effect does not appear in the general population. Based on analyses of survival curves as well as mean time to event, we found that women had a later age at initiation of alcohol use (consistent with telescoping) but had neither a shorter time to dependence once alcohol use was initiated nor a shorter time to first treatment after onset of alcohol dependence. In fact, men had a shorter time to dependence in every birth cohort. We examined evidence for these outcomes in five different birth cohorts spanning 40 years and found little evidence of a telescoping effect in any of these cohorts. These results stand in contrast to studies of clinical populations (
1–
6) and suggest that the telescoping effect disappears when all individuals at risk are considered.
Second, variation by birth cohort in the course of alcohol dependence is evident in these data. Survival analysis showed that later cohorts were more likely to initiate alcohol use (with the exception of the youngest cohort). Decreases in alcohol use initiation from cohort 2 to cohort 1 are consistent with per capita alcohol consumption data in the United States more generally (
22), although factors that mediate the decrease (e.g., an increase in the minimum drinking age) remain unclear. Furthermore, the rate of transition to dependence given initiation of alcohol use is increasing in each successive cohort. These findings extend recent work indicating cohort effects in the prevalence of alcohol dependence (
12–
15), documenting cohort effects in the timing of landmark events, including time to alcohol use initiation and time to alcohol dependence. Third, we found that cohort effects operate differently between genders in the overall hazard of alcohol use and dependence: increases in rates of alcohol use initiation and alcohol dependence between earlier and later birth cohorts were more pronounced in women than in men. While men remain more likely to initiate alcohol use and to develop alcohol dependence compared to women, the gender difference appears to be diminishing in more recent cohorts. Furthermore, survival curves and the direction of gender-specific hazard ratios by cohort suggest that the gender difference in time from use to dependence is actually increasing in more recent cohorts. Men had a shorter time from first drink to dependence compared to both women in more recent cohorts and men in earlier cohorts. This finding is in direct conflict with the telescoping hypothesis, which suggests that women have a faster progression from first drink to dependence.
Gender convergence in the overall hazard of alcohol dependence in recent birth cohorts is consistent with the possibility that earlier gender differences in alcohol problems stemmed from protective social factors (e.g., drinking norms sanctioning female drinking) that have diminished as overall gender norms have shifted (
1,
4,
5,
15). While we know of no formal tests of this possibility, research provides evidence consistent with a role for changing norms. For example, studies have documented increases in the acceptability of women drinking and getting drunk (
23) and increased exposure to alcohol advertising among adolescent women (
24). Furthermore, the World Health Organization World Mental Health Surveys (
15) indicate that diminished gender differences in alcohol disorders are most pronounced in countries where traditional gender roles (e.g., women in the workforce) have concurrently changed. Research formally testing mediators of the cohort-by-gender effect is necessary to advance our understanding of the role of changing social factors in the development of alcohol consumption and alcohol disorders. While cohort effects on gender differences in the overall hazard appear to be converging in more recent birth cohorts, the gender difference in time from first use to onset of dependence is becoming wider, with the average time from first use to dependence faster in men than in women, especially in younger cohorts. Further research assessing potential mediators of both time to dependence and overall hazard of dependence is warranted.
We found limited evidence for a cohort effect on time from dependence to treatment and no evidence of a gender-by-cohort or gender-by-cohort-by-time interaction on this outcome. It is likely that forces other than gender norms are important in the delivery of mental health services (such as access through health insurance), which could account for the discrepant findings on this outcome. However, continued monitoring of gender differences in treatment initiation is necessary to observe long-term effects of both the earlier age at initiation of use and the shorter time from use to dependence in more recent cohorts of women. Monitoring is especially important in light of evidence indicating that women with alcohol use disorders have more medical problems compared to men (including higher overall mortality [
25], cancer of the liver and breast [
26,
27], myocardial infarction [
28], and neurological damage [
29,
30]).
Our study had several limitations. First, the older participants in these surveys were reporting on the timing of landmark events that may have occurred several years before the survey interview. Retrospective reporting of alcohol history is imperfect (
31,
32). However, our research aims could not be addressed without using such data, because existing longitudinal studies have neither the long-term follow-up nor the potential variation across many birth cohorts to observe these effects. In a sensitivity analysis designed to detect potential recall bias, we tested whether the prevalence of alcohol dependence that began at age 25 or later differed between members of any given birth cohort by whether they were interviewed in the NLAES or in the NESARC, when the birth cohort was 10 years older. A lower prevalence of dependence beginning at age 25 or older in members of a given cohort interviewed in the NESARC would suggest the presence of recall bias. In fact, no such differences in prevalence were found, which suggests a limited impact of recall bias on these analyses. Second, while this analysis included over 50,000 individuals, with at least 4,600 in each cohort, treatment utilization is relatively rare in the general population, with 24.6% of alcohol-dependent individuals in these data ever utilizing any type of alcohol treatment (consistent with national estimates [
16]). Thus, while these data provide the most comprehensive resource for general population estimates, our study did not have sufficient power to detect small effects regarding cohort differences in treatment. Third, while the NLAES and the NESARC are comparable in sampling frame, study design, and measurement, unmeasured confounding factors between surveys could have introduced bias into the results. To address this possibility, we controlled for the survey in all analyses. Additionally, in post hoc analyses, we examined outcomes by birth cohort and gender in each survey. All findings were similar in direction and magnitude to those presented here, which suggests that minor study design differences did not confound our results.
A greater clinical focus on screening and treatment for alcohol use disorders among young women is warranted given this and other accumulating evidence (
12,
13,
15) on the changing course of alcohol use disorders in women. As women increasingly engage in alcohol use earlier in life and exhibit drinking patterns and disorders at ages similar to men, screening for alcohol use disorders among younger women who present for primary care or treatment for non-alcohol-related psychiatric disorders appears to be warranted as an increasingly important component of overall evaluation. In addition, our evidence suggesting that the time from first use to dependence is shorter in men than in women, especially in later birth cohorts, emphasizes the importance of continued alcohol use disorders assessment and intervention in men and the need for additional investigation of this apparent acceleration of the course of alcohol dependence in younger men. Evidence-based guidelines from the National Institute on Alcohol Abuse and Alcoholism for brief alcohol assessment and intervention provide useful information on such screening for clinicians who do not specialize in the treatment of alcohol use disorders (
33).