Behavioral problems are not only a frequent finding among patients with Alzheimer's disease (AD),
1 but may also pose a serious burden to relatives and caregivers. Although depression is the most prevalent emotional disorder in AD, irritability and aggressive outbursts are also frequent and may seriously impair quality of life for patients and their families.
2Deutsch et al.
3 examined the relationship between psychosis and episodes of physical aggression in 181 AD patients attending a research clinic. They found aggressive episodes in 30% of the patients and also reported a significant association between delusions and episodes of physical aggression. A similar prevalence of aggressive episodes was reported by Burns et al.
4 (32%) in 31 patients with AD and by Mendez et al.
5 (25%) in a retrospective chart-review study of 217 outpatients with AD. Aarsland et al.
6 explored the relationship between aggressive behavior and other neuropsychiatric symptoms in 75 patients with AD. They reported that 25 patients (33%) had verbal outbursts and 13 patients (17%) had physical aggressiveness, but they could not find significant differences in age, education, gender, level of depression, or severity of dementia between aggressive and nonaggressive AD patients.
However, most of these studies have important methodological limitations, such as a retrospective design, lack of standardized instruments to measure aggressive behaviors, and no structured psychiatric interviews. Moreover, other potential correlates of aggressive behavior, such as premorbid personality traits, concomitant medical disease, and physical impairments, have not been previously examined.
For the present study, we assessed a consecutive series of 196 patients with probable AD for the presence of aggressive behaviors. All patients were examined with a standardized psychiatric interview that included both the Overt Aggression Scale and the Irritability Scale, as well as specific assessments for depression, anxiety, apathy, emotional lability, and personality disorders and traits.
METHODS
Patients
We examined a consecutive series of 196 patients who attended the neurology clinic of our Institute between February 1991 and February 1995 because of progressive cognitive decline. Our institute is not a tertiary care center, but provides neurological care to a wide area of Buenos Aires city. Thus, most of our sample is of urban origin. The inclusion criteria were the following: 1) NINCDS-ADRDA criteria
7 for probable AD, 2) normal laboratory test results, 3) no history of closed head injuries with loss of consciousness, strokes, or other neurologic disorders with central nervous system involvement, 4) no focal lesions on the CT or MRI scan, and 5) a Hachinski Ischemic score of 4 or less.
Psychiatric Examination
After giving informed consent, patients were assessed by a psychiatrist with the following instruments:
Overt Aggression Scale (OAS).8 The OAS measures specific aspects of aggressive behavior on the basis of observable criteria. Aggressive behaviors are divided into four categories: verbal aggression and physical aggression against objects, against self, and against others. Within each category, descriptive statements and numerical scores are provided to define and rate four levels of severity. Following the procedure of Burns et al.,
4 we asked informants about the presence and type of aggressive outbursts during the preceding 4 weeks.
On the basis of the OAS scores, patients were divided into a group without aggression (score of 0 on every item of the OAS), a group with verbal aggression (score of 1 or more points on the verbal aggressiveness section and 0 on the remaining items), and a group with physical aggression (score of 1 or more points on at least one of the nonverbal sections).
Structured Clinical Interview for DSM-III-R (SCID).9 The SCID, a semistructured diagnostic interview for making the major Axis I DSM-III-R diagnoses, was carried out with the patient and at least one first-degree relative. DSM-III-R Axis I diagnoses were made on the basis of SCID responses.
Structured Clinical Interview for DSM-III-R–Personality Disorders (SCID-II).9 The SCID-II is a 100-item questionnaire designed to evaluate DSM-III-R personality disorders. It was filled out by the patient with the help of at least one first-degree relative. They were asked to answer the questions on the basis of the patient's behavior before the onset of the cognitive impairment. Several days later the patient and the relative were interviewed a second time and were questioned about those answers rated positive. On the basis of these answers, a diagnosis of personality disorder was made by using DSM-III-R criteria.
Hamilton Rating Scale for Depression.10 This is a 17-item interviewer-rated scale that measures psychological and autonomic symptoms of depression.
Hamilton Anxiety Scale.11 This is an 11-item interviewer-rated scale that measures the severity of generalized or persistent anxiety.
Anosognosia Questionnaire–Dementia.12 This instrument consists of 30 questions divided into two sections. The first section assesses anosognosia for intellectual functioning, and the second section examines anosognosia for changes in interests and personality.
Bech Mania Scale.13 This scale assesses the severity of manic symptoms, such as euphoria, hyperactivity, flight of ideas, hypersexuality, and decreased need of sleep.
Pathological Laughing and Crying Scale.14 This instrument is an interviewer-rated scale that quantifies aspects of pathological affect.
Apathy and Irritability Scales.15 These scales include 14 items that are scored by the patient's relative or caretaker.
Dementia Psychosis Scale.16 This is an 18-item scale that quantifies the severity and types of delusions in demented patients at the time of the psychiatric evaluation.
Functional Independence Measure.17 This instrument assesses self-care, sphincter control, mobility, locomotion, communication, and social cognition on a low-level scale.
Additionally, relatives or caretakers were systematically asked about the patients' past and present medical illnesses, medications administered to the patient, and approximate date of onset of cognitive decline.
Neurological Examination
Patients were examined with the Unified Parkinson's Disease Rating Scale (UPDRS),
18 a semistructured scale that assesses the presence of extrapyramidal signs. The motor section of the UPDRS was scored by a neurologist blind to the remaining clinical findings.
Neuropsychological Examination
Patients were examined with the following instruments:
Mini-Mental State Examination (MMSE).19 The MMSE is an 11-item examination that has been found to be reliable and valid in assessing a limited range of cognitive functions.
Raven's Progressive Matrices (RPM).20 This test assesses reasoning in the visual modality.
Wisconsin Card Sorting Test.21 This test measures the ability to develop new concepts and shift sets. It also requires the subject to suppress a previously correct response and produce a new one.
Controlled Oral Word Association Test.22 This test examines access to semantic information with time constraint.
Trail Making Test.23 This test examines visual, conceptual, and visuomotor tracking.
Digit Span.24 This test examines auditory attention.
Buschke Selective Reminding Test.25 This test measures verbal learning and memory during a multiple-trial list-learning task.
Benton Visual Retention Test.26 This test assesses visual perception and visual memory.
Token Test.27 This test examines verbal comprehension of sentences of increasing complexity.
Boston Naming Test.28 This test examines the ability to name pictured objects.
Apraxia Subtest of the Western Aphasia Battery.29 This test examines the presence of ideomotor apraxia.
Block Design.30 This test examines the presence of constructional apraxia.
Similarities.30 This test provides a measure of abstract reasoning.
Statistical Analysis
Statistical analysis was carried out by using means and standard deviations, multivariate analysis of variance (ANOVA), and post hoc planned comparisons. Frequency distributions were compared by using χ2 tests with a Yates correction for cell sizes less than 5. All P-values are two-tailed.
RESULTS
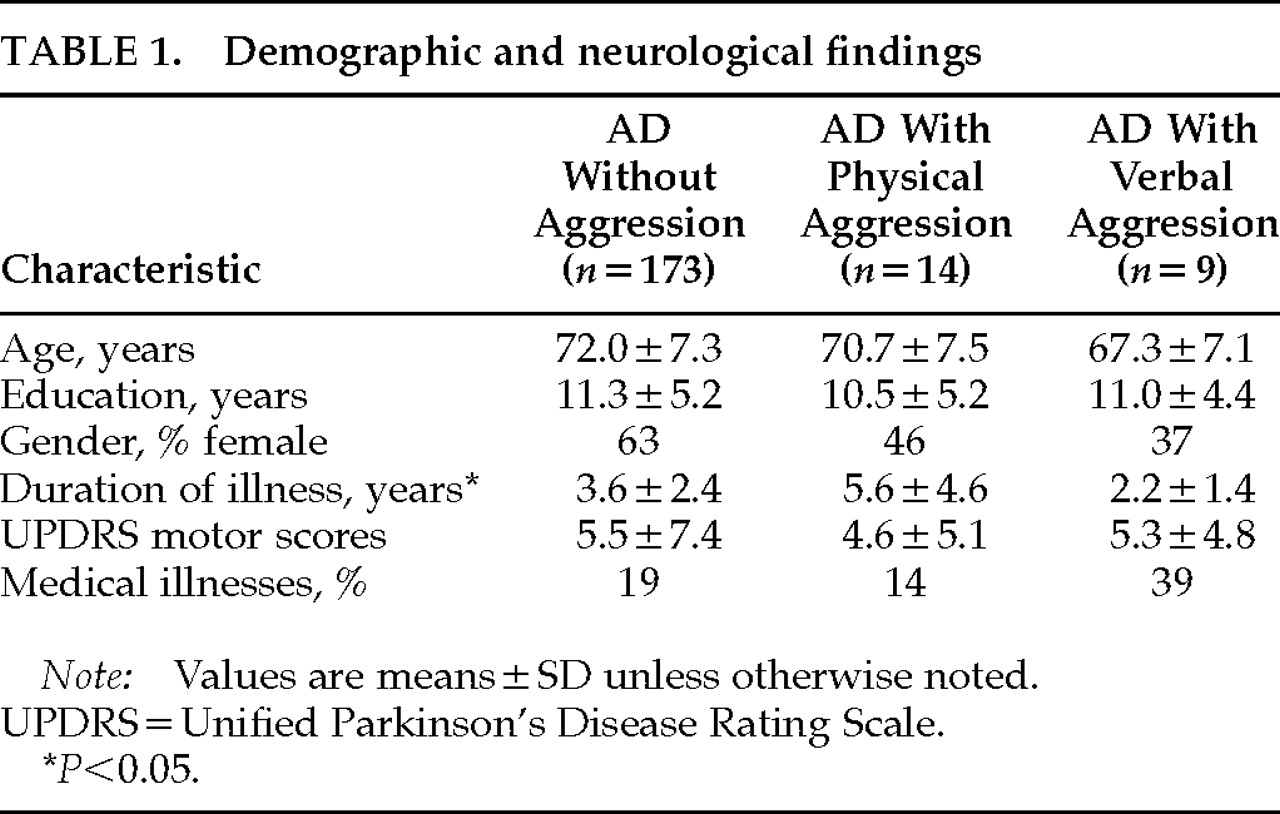
Demographic, Neurological, and Clinical Findings (Table 1)
On the OAS, 173 patients (88%) did not show aggressive episodes, 9 patients (5%) showed verbal aggression only, and 14 patients (7%) showed physical aggression, including 11 patients (79%) with and 3 patients (21%) without concomitant verbal aggression. No significant between-group differences were found in age, education, or gender distribution. There was a significant difference in duration of illness (F=5.46, df=2,194, P<0.01): patients with physical aggression had a significantly longer duration of illness than patients with either verbal aggression (P<0.01) or no aggression (P<0.01).
A one-way ANOVA for UPDRS scores showed no significant between-group differences. The most frequent clinical disorders in our group of AD patients were hypertension, cardiac arrhythmias, arthrosis, and diabetes, and the prevalence of these disorders was similar in all three groups.
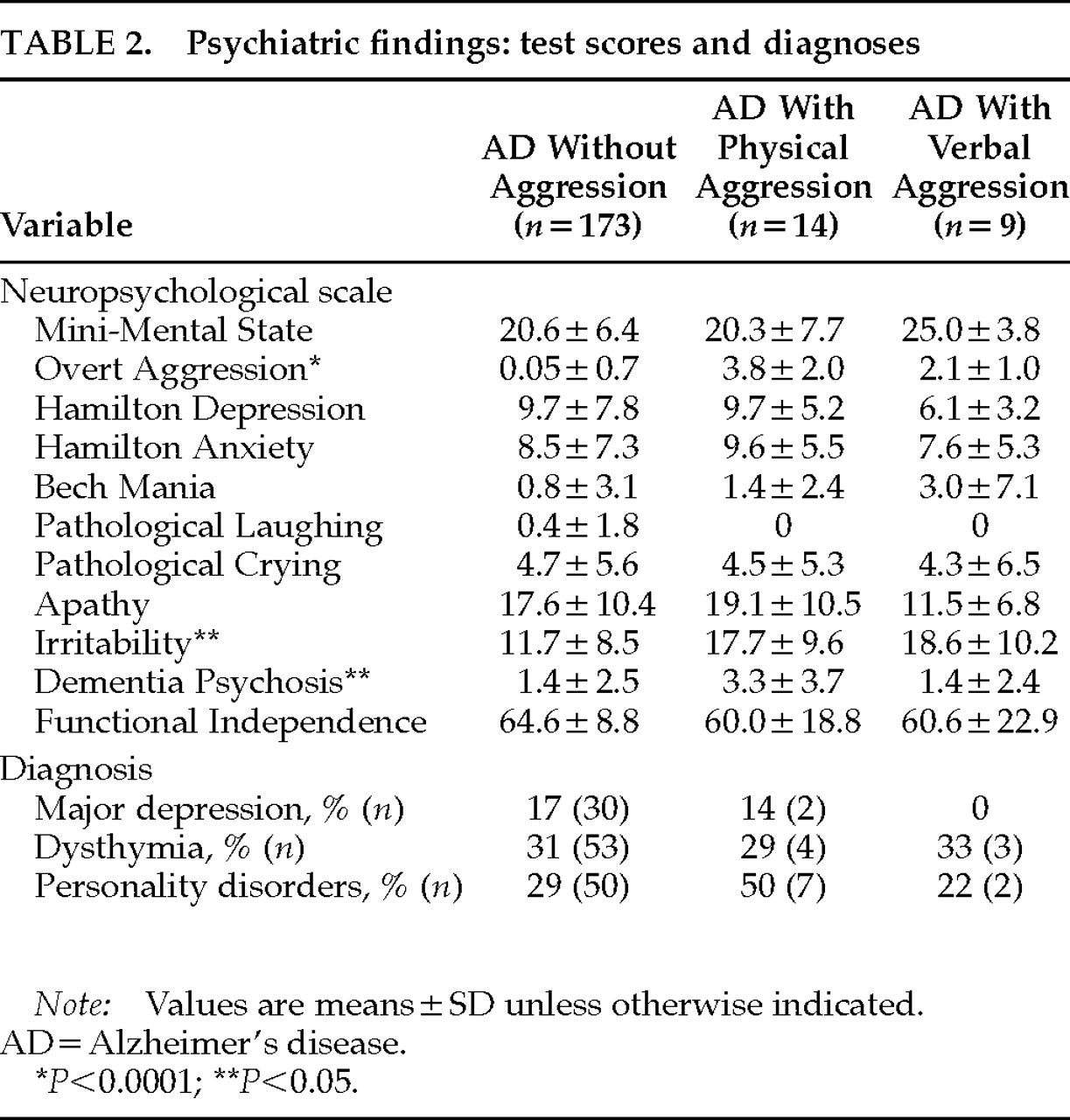
Psychiatric Findings (Table 2)
As expected, there was a significant between-group difference in OAS scores (F=3.92, df=2,197, P<0.0001): patients with physical aggression had significantly higher scores than patients with verbal (P<0.0001) or no aggression (P<0.01), whereas patients with verbal aggression showed significantly higher OAS scores than patients without aggression (P<0.01).
There also were significant between-group differences on the Dementia Psychosis Scale (F=3.61, df=2,192, P<0.005): patients with physical aggression had significantly higher Dementia Psychosis Scale scores than patients without aggression (P=0.001). No significant differences were found between patients with and those without verbal aggression.
Finally, there were significant between-group differences on the Irritability Scale (F=17.3, df=2,196, P<0.05): patients with either physical or verbal aggression had significantly higher irritability scores than patients with no aggression (P<0.01 and P<0.05, respectively).
Prevalence of major depression, dysthymia, and premorbid personality disorders did not differ significantly between groups. Moreover, there were no significant between-group differences on depression, anxiety, emotional lability, anosognosia, apathy, or MMSE scores (
Table 2).
Antidepressant drugs were used by 24 patients (14%) from the nonaggressive group, 1 patient (11%) from the verbal aggression group, and 1 patient (7%) from the physical aggression group. Antipsychotic medication was used by 4 patients (2%) from the nonaggressive group and 1 patient (7%) from the physical aggression group. Anxiolytic medication was used by 28 patients (16%) from the nonaggressive group, 3 patients (33%) from the verbal aggression group, and 5 patients (36%) from the physical aggression group. There was a significantly higher use of anxiolytic and antipsychotic medication for AD patients with aggression as compared to AD patients without aggression (χ2=4.68, df=1, P<0.05).
When we divided AD patients into those with OAS scores equal to 0 or 1 (n=177) and those with OAS scores greater than or equal to 2 (n=19), patients with higher OAS scores had significantly higher scores on scales of delusions (t=2.35, P>0.05), irritability (t=3.03, P>0.05), and activities of daily living (t=2.39 P>0.05).
Neuropsychological Findings
Each patient with verbal or physical aggression was matched for age (±5 years) and MMSE scores (±3 points) with 2 patients without aggression. A multivariate ANOVA for the neuropsychological variables showed no significant main effect (Wilks's lambda=0.31, not significant; data not shown). When groups were matched for mean premorbid years of education completed (AD without aggression, n=44, 11.3±1.6 years; AD with physical aggression, n=44, 11.7±5.5 years; AD with verbal aggression, n=9, 10.2±6.4 years), no significant differences were observed (Wilks's lambda=0.68, not significant).
DISCUSSION
This study examined the prevalence and correlates of aggression in a consecutive series of 196 patients with AD, and there were several important findings: 1) 12% of patients showed aggressive episodes—5% with verbal aggression and 7% with physical aggression—during the 4 weeks preceding the psychiatric evaluation; 2) physical aggression was significantly associated with more frequent delusions and more severe irritability; 3) patients with verbal aggression had a significantly shorter duration of illness than AD patients without aggression; and 4) there were no significant differences on the severity of cognitive impairment and other psychiatric disorders such as depression, apathy, anxiety, emotional lability, and anosognosia between AD patients with and those without aggression.
Our study had several limitations. First, we based the diagnosis of physical or verbal aggression on the OAS scores and not on specific criteria. Future studies should develop and validate standardized criteria for the diagnosis of aggression in AD. Second, this being a cross-sectional study, longitudinal changes in the prevalence of aggression in AD should be examined in follow-up studies.
In our sample of 196 AD patients, we found episodes of physical aggression in 7% and verbal aggression in 5%. Although this prevalence is lower than frequencies reported in other studies, our larger sample size, more stringent criteria for the diagnosis of aggressive behavior, recruitment of patients from a neurology clinic rather than a psychiatric clinic, use of a specific instrument to measure aggression, and restriction of assessment of aggressive behaviors to the period of 4 weeks preceding the psychiatric evaluation may account for this discrepancy. Although the presence of aggressive behavior may be assessed retrospectively for the whole period of cognitive impairment, the absence of adequate informants may not allow a fair assessment for many patients.
We also examined clinical correlates of aggressive behavior in AD. We found that AD patients with verbal or physical aggression had significantly more severe irritability than AD patients without aggression. Although this would seem to be an expectable finding, Burns et al.
4 could not find a significant association between irritability and aggressive behavior. This discrepancy may result from different methods used to measure irritability: whereas Burns et al.
4 rated irritability on a 5-point scale, we used a comprehensive scale with proven validity and reliability. We also found that AD patients with physical (but not verbal) aggression had significantly more frequent delusions (as assessed with a scale specifically used to measure psychosis in dementia) than AD patients without aggressive behavior, which replicates the findings of Deutsch et al.
3 Thus, among AD patients, aggressive outbursts may occur in the context of delusions and irritable mood.
ACKNOWLEDGMENTS
The authors thank Paul Fedoroff, M.D., for his helpful suggestions. This study was partially supported by grants from the Raúl Carrea Institute of Neurological Research, the Fundación Perez Companc, and the Consejo Nacional de Investigaciones Científicas y Técnicas.