Transcranial magnetic stimulation is being studied as a novel method of stimulating brain neurons in conscious humans
(1). Uncontrolled
(2) and controlled
(3, 4) studies have reported antidepressant effects for transcranial magnetic stimulation, especially left prefrontal rapid transcranial magnetic stimulation. In normal subjects, transcranial magnetic stimulation has also been reported to cause mood changes specific to brain side in two separate controlled studies
(5, 6). Paradoxically, the studies of normal subjects found increased sadness with left prefrontal stimulation and increased happiness with right prefrontal stimulation.
ECT is effective in mania as well as depression
(7). Since transcranial magnetic stimulation may have ECT-like properties
(8), we decided to study transcranial magnetic stimulation in mania. Because the studies in depressed and normal subjects suggested a laterality of transcranial magnetic stimulation effects, we decided to compare left with right prefrontal transcranial magnetic stimulation in patients with mania who were also receiving unrestricted drug treatment.
METHOD
A patient admitted to the Beersheva Mental Health Center in Israel could enter the study if he or she met DSM-IV criteria for mania by consensus of two psychiatrists after clinical interview. No changes in clinical pharmacotherapy were made because of study participation. Patients with a history of epilepsy, neurosurgery, brain trauma, cardiac pacemaker implant, or drug abuse were excluded. The study was approved by our Helsinki Committee, and all patients gave written informed consent.
Patients were hospitalized for a mean of 8.6 days (range=1–38) before entering the study. Eighteen patients were enrolled (of 62 patients with mania admitted to our hospital over the period of the study). Two of the 18 patients dropped out, one after four transcranial magnetic stimulation treatments because of severe worsening of mania and a positive urine for nonprescribed drugs, and the other before any transcranial magnetic stimulation treatment because of change in diagnosis. Of the 16 patients who completed the study, 12 had nonpsychotic mania and four had psychotic mania. Seven were men (two in the right transcranial magnetic stimulation group) and nine were women (five in the right transcranial magnetic stimulation group).The patients’ mean age was 33 years (range=20–52); the mean age of the patients given right transcranial magnetic stimulation was 35, and that of the patients given left transcranial magnetic stimulation was 32.
Among the nine patients receiving left prefrontal transcranial magnetic stimulation, concomitant drug therapy consisted of lithium for six patients, carbamazepine for one patient, valproate for one patient, and no mood stabilizer for one patient. Eight of these patients also received neuroleptics (mean dose=340 mg/day in chlorpromazine equivalents, range=150–600).
Among the seven patients receiving right prefrontal transcranial magnetic stimulation, five were receiving lithium, two were receiving carbamazepine, and one was receiving no mood stabilizer. Four of these patients also received neuroleptics (mean=240 mg/day in chlorpromazine equivalents, range=75–600).
The first six patients were randomly assigned to right or left stimulation by one of us (R.H.B.) and then rated by an observer (N.G.) who was not blind to the site of stimulation because no hypothesis had yet been formed. As it became apparent that right stimulation seemed more therapeutic, a blind rater (Y.Y.) began to do all clinical ratings. Since there was no difference in the magnitude of the left versus right difference between the first six patients rated by the nonblind observer and the following 10 patients rated by the blind observer, the results were analyzed both combined and also separately for the 10 patients rated blindly.
Patients were assessed at four time points: 24 hours before the first transcranial magnetic stimulation (baseline), 3 and 7 days after the first treatment, and at the end of the study (day 14). Day 14 was usually 4 days after the final transcranial magnetic stimulation. The following assessment instruments were used: the Clinical Global Impression (CGI); Mania Scale
(9); and Brief Psychiatric Rating Scale (BPRS).
A Cadwell high-speed magnetic stimulator with a 9-cm diameter circular coil was used. Each patient was assessed for motor magnetic threshold
(1) before the first treatment, and 80% of the individual patient motor threshold was then administered on all treatment days. Mean patient motor threshold was 67% for the left treatment group (range=50%–80%) and 72% for the right treatment group (range=55%–85%).
Patients were given 10 daily consecutive sessions of 20 trains per session. Frequency was 20 Hz for 2 seconds per train; intertrain interval was 1 minute. Each of the participants was given the stimuli over the right prefrontal cortex or the left prefrontal cortex, randomly assigned by one of us (R.H.B.).
RESULTS
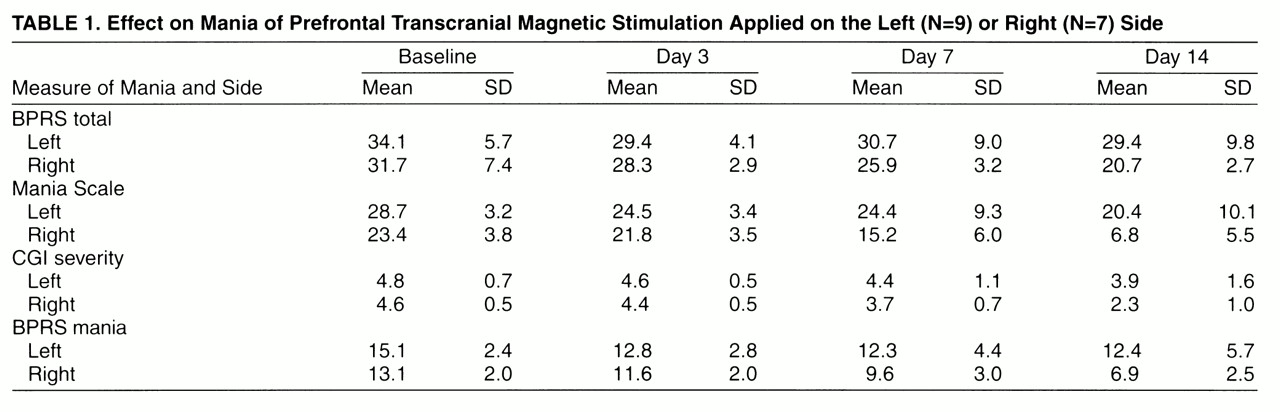
Table 1 shows the scores on the BPRS, Mania Scale, CGI, and BPRS mania factor of patients treated with prefrontal transcranial magnetic stimulation on the left or right side. For total BPRS, two-way repeated measures analysis of variance (ANOVA) with covariance for baseline showed a significant effect of time (F=3.9, df=2, 28, p=0.03) and a significant interaction of time and side of transcranial magnetic stimulation (F=3.4, df=1.2, 17.2, p<0.08, Greenhouse-Geiser-corrected). Post hoc Sheffé test showed a significant effect of side of transcranial magnetic stimulation on day 14 (p=0.01).
For the Mania Scale, two-way repeated measures ANOVA with covariance for baseline showed a highly significant effect of time (F=16.0, df=2, 28, p<0.0001) and a significant interaction of time and side of transcranial magnetic stimulation (F=5.2, df=1.4, 19.2, p=0.04, Greenhouse-Geisser-corrected). Post hoc Sheffé test showed a significant effect of side of transcranial magnetic stimulation at day 7 (p=0.03) and day 14 (p<0.001).
For the BPRS mania factor, which includes the items excitement, grandiosity, hostility, tension, and uncooperativeness, two-way repeated measures ANOVA with covariance for baseline showed a significant effect of time (p=0.02) and a significant interaction of side of transcranial magnetic stimulation and time (F=3.4, df=1.7, 23.2, p=0.05, Greenhouse-Geisser-corrected). Post hoc Sheffé test showed a significant effect of side of transcranial magnetic stimulation at day 14 (p<0.01).
For the CGI, two-way repeated measures ANOVA with covariance for baseline showed a highly significant effect of time (F=14.6, df=2, 28, p<0.0001) and a significant interaction of time and side of transcranial magnetic stimulation (F=3.9, df=1.5, 28, p=0.06, Greenhouse-Geisser corrected). Post hoc Sheffé test showed a significant effect of side of transcranial magnetic stimulation at day 14 (p=0. 03).
DISCUSSION
These results suggest that transcranial magnetic stimulation of the right prefrontal cortex has therapeutic effects in mania. This is the opposite lobe reported to have antidepressant effects
(3, 4). Interestingly, right unilateral ECT was not found to be effective in mania in a small group of patients
(7). The effects of transcranial magnetic stimulation in psychiatry may be complex; for example, certain stimulation patterns enhance neuronal activity and cause, for instance, a motor movement, whereas other stimulation patterns can disrupt neuronal outflow and cause, for instance, speech arrest
(1). Thus, further studies of frequency of the magnetic stimulus, its intensity, and its location will be necessary before the contrast with ECT is proven.
Although psychopathology ratings were consistently somewhat lower at baseline in the group given right transcranial magnetic stimulation than in the group given left stimulation (
table 1), covariance with baseline should adequately control for this factor, which in any case usually associates higher baseline ratings with greater treatment response in mania. No clinically significant side effects of transcranial magnetic stimulation were observed in this small study with either right or left transcranial magnetic stimulation. The present study was terminated at 16 patients because of the clinical impression that patients in the left prefrontal transcranial magnetic stimulation group were responding more poorly than would be expected given their adequate pharmacotherapy; i.e., left prefrontal transcranial magnetic stimulation may worsen mania. Therefore, we plan an immediate follow-up study of right prefrontal active transcranial magnetic stimulation compared with right prefrontal sham transcranial magnetic stimulation in mania.