Acute residential alternatives are not halfway houses that support patients after a hospital stay but, rather, homes in neighborhoods that are staffed and organized to accept and treat acutely decompensated patients in lieu of voluntary admission to a psychiatric ward of a general hospital or state psychiatric facility. Residential alternatives have been described for more than 25 years but have not been widely used (
1,
2). Current efforts to control medical costs, however, have moved into center stage the search for effective non-hospital-based options for psychiatric (and other) patients requiring acute care (
3).
In a randomized study narrowly focused on young adults newly diagnosed with schizophrenia and treated with no or minimal antipsychotic medications, Mosher et al. demonstrated that care in a homelike acute residential facility (Soteria) generated patient outcomes comparable or superior to those of treatment in the inpatient unit of a mental health center (
4–
6). Although clinical reports describe the adaptation of the Soteria model to more typical patients with longstanding and recurrent mental illness (
6–
14), a rigorous assessment of this model has yet to be reported. Accordingly, we conducted a randomized clinical trial to assess the clinical effectiveness of treatment in an acute residential alternative compared to general hospital psychiatric ward care for voluntary patients with severe and persistent mental illness.
METHOD
Subjects
Adult patients under the care of the Montgomery County, Md., Department of Health and Human Services were eligible for participation in this study. As the sole local public mental health authority, the Montgomery County Department of Health and Human Services manages a comprehensive network of services that supports approximately 1,600 adults with serious and persistent mental disorders at any given time. Annually, about 12% of these patients experience an illness exacerbation requiring one or more hospitalizations.
Patients who met the following criteria were referred for randomization: 1) were judged by their treating clinician to be in need of hospital-level care, 2) were judged not to require acute general medical care or detoxification, 3) had Medicaid or Medicare funding, and 4) were willing to accept voluntary placement. Voluntary patients experiencing acute psychosis, depression, suicidality, homicidality, or concomitant substance abuse were not excluded from randomization.
Treatment Sites
McAuliffe House is a eight-bed crisis alternative located in a ranch-style house in a residential neighborhood in Rockville, Md. The program is staffed by two bachelor's-level counselors 24 hours per day under the direction of a master of social work-level program director. During the residential treatment episode, medical responsibility for each patient's care is maintained by the patient's outpatient psychiatrist, who prescribes or changes psychotropic medications and orders outpatient laboratory assessments and other medical evaluations as indicated. Each newly admitted patient is also evaluated by a consulting psychiatrist, who, in addition to providing a written second opinion, meets with program staff weekly to assist in treatment planning, monitor progress, and provide staff supervision. The McAuliffe program model was based on Soteria and Crossing Place and has been described in detail (
4–
13). Beyond a supportive environment, supervised medication self-administration, and the availability of one-to-one staff monitoring, formal treatment is not provided in the alternative. Rather, continued participation in ongoing community-based treatment, rehabilitation, school, work, or other activities is supported to an extent allowed by patients' symptoms. If needed, program staff provide transportation to these appointments or activities. Emergency backup for the residential alternative is provided by a mobile treatment team if evaluation for involuntary hospitalization becomes necessary. The efficacy of the model is thought to derive from a normalizing homelike environment that minimizes stigma, loss of esteem, and assumption of the sick role while allowing patients to maintain continuity with outpatient treatment providers and community supports (
14–
18).
The control treatment site was Montgomery General Hospital, Olney, Md., a 229-bed general hospital, accredited by the Joint Commission on Accreditation of Healthcare Organizations, that since 1971 has operated a 31-bed inpatient psychiatric treatment unit supported by a day hospital and outpatient clinic. Hospital care includes medical assessment, individual psychotherapy, group therapy, and pharmacologic management.
Assignment Procedures
Admission procedures, approved by the institutional review board, were as follows: First, at the time of crisis assessment, a Montgomery County Department of Health and Human Services clinician and the patient agreed on the need for inpatient treatment. Second, after determining patient eligibility, the clinician contacted the department's 24-hour crisis center, which randomly assigned the patient to one or the other treatment condition according to a computer-generated pattern. Referring clinicians were not members of the research team and thus were blind to the randomization sequence. Third, following admission, the patient was approached to provide written informed consent to participate in subsequent study assessments.
Although the research team monitored adherence to the random assignment procedure, because all admissions were voluntary, both referring clinicians and randomized patients were free to decline admission after learning the assignment. In the intention-to-treat group, 27 (14%) of 185 randomized subjects declined admission after receiving assignment. While these patients were denied admission to the treatment option to which they were not assigned, they were free, with their clinicians' assistance, to seek admission to one of the other inpatient programs in the area. An additional 11 patients withdrew consent for assessment interviews, and 11 either did not arrive at their assigned placement or left within 24 hours. Seventeen patients were not entered for administrative or other reasons (e.g., benefits were found to be inactive after randomization, site was full). Overall, unsuccessful entry was more common among those assigned to the hospital (N=42) than those assigned to the alternative (N=24) (χ2=7.63, df=1, p<0.01). Because this trend was noted early in the study, the ratio of random assignments was set at 10:7 to favor hospital placement. Nonetheless, the final group included 69 alternative and 50 hospital participants.
Outcome Assessment
Clinical program effectiveness was assessed by evaluating changes in patient symptom severity, patient satisfaction with treatment episode, and percentage of patients successfully discharged to the community. Psychosocial functioning, service utilization, and life satisfaction in the 6 months before and after the treatment episode were evaluated as secondary measures of clinical effectiveness. Randomized patients were assessed by a member of the research team at three points: 1) within 48 hours of admission (mean=28, SD=13), 2) within 48 hours of discharge (mean=20, SD=26), and 3) 6 months after admission (mean=222 days, SD=85).
Symptom severity was rated at each time by using the Positive and Negative Syndrome Scale (
19). Patient satisfaction with episode treatment was measured at discharge with a 10-item satisfaction survey based in part on the Quality of Life Scale (
20). Discharge was considered successful if the patient was returned to the community and unsuccessful if the treatment episode ended in transfer to another inpatient facility.
At admission, data concerning premorbid functioning and illness onset, severity, and history, as well as psychosocial functioning and service utilization over the prior 6 months, were collected by using an interview schedule based on our earlier work on the prediction of outcome in serious mental illness (
21,
22). Psychosocial functioning and 6-month service utilization were again assessed at 6-month follow-up. Psychosocial functioning during each 6-month period was assessed in the domains of family, social, and romantic relationships; work performance; living situation; and service utilization. Patient satisfaction ratings in each of these areas were obtained on a scale from 1 (extremely dissatisfied) to 7 (extremely satisfied). Data concerning episodes of homelessness and arrests were collected through patient interview for each 6-month period. Axis I, axis II, and substance abuse diagnoses were established through administration of the Structured Clinical Interview for DSM-III-R (SCID and SCID-II [23, 24]) during the treatment episode.
All assessments were administered by six interviewers who were graduate students in psychology or social work and/or had at least 5 years' experience working with patients with serious mental illness. Interviewers underwent approximately 50 hours of training (including the rating of 22 videotaped interviews) to establish SCID and Positive and Negative Syndrome Scale reliability. Mean reliability achieved by interviewers across major diagnostic categories (psychotic disorders, mood disorders, substance abuse) was 0.74 (kappa). Mean reliability for Positive and Negative Syndrome Scale total psychopathology severity was 0.80 (intraclass correlation). To minimize missing data, interviewers obtained information as needed from family members, treatment staff, and medical records. All available medical records, including state Title XIX data tapes, were reviewed to validate patient-reported acute care days.
Statistical Analysis
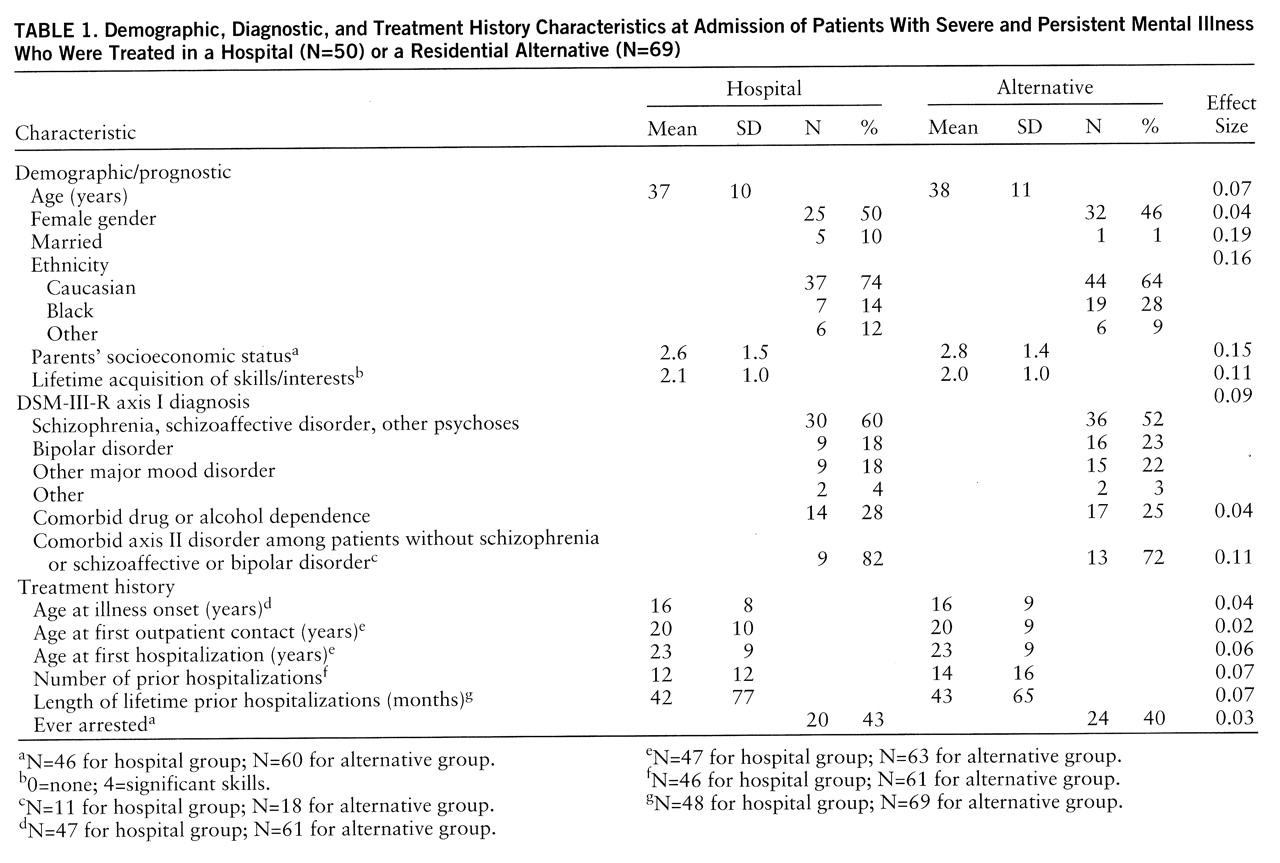
To permit bias testing of missing subgroups, Montgomery County Department of Health and Human Services medical records of all randomized subjects were independently reviewed, and 27 case mix variables were coded. Randomization was further evaluated by comparing patients assigned to each site across an additional 15 core interview-derived demographic, diagnostic, and clinical case mix variables (
table 1). Variables were selected and grouped a priori into conceptual domains (e.g., demographic, diagnostic, and historical variables), and Bonferroni-corrected criterion alpha levels were used to limit the chance of a type I error from multiple comparisons (
25). Patients treated in each setting were then compared across clinical outcome measures. Between-group analyses were conducted by using two-tailed t tests for dimensional and chi-square analyses for categorical dependent variables. Square-root transformations were applied to variables with nonnormal distributions for all statistical analyses. Effect sizes are presented as phi or Cramer's V for chi-square analyses and Cohen's d for t test comparisons (
26). Mixed design repeated measures analyses of variance (ANOVAs) were used to test the significance of changes in symptoms and continuous psychosocial and service utilization variables across assessments and to evaluate time-by-treatment site interactions.
RESULTS
Study Population
Between July 1992 and December 1994 a total of 185 individuals who met entry criteria were randomized; 119 (64%) successfully entered the study. To determine whether the 66 unsuccessful admissions differed from the 119 successful admissions, the subgroups were compared across seven demographic, six treatment history, three diagnostic, four personal history, and seven prognostic/illness severity variables on the basis of information coded from their outpatient charts. The subgroups did not differ significantly on any of these 27 variables, suggesting that the study group adequately represented the total group of patients referred for inpatient treatment.
The average age of the final treated group (N=119) was 37 years (SD=10); 62 (52%) were male, and 38 (32%) were non-Caucasian. Most patients (N=81 [68%]) had never married; 18% (N=21) were divorced. Ninety-five percent of patients met DSM-III-R criteria for schizophrenia (N=33 [28%]), schizoaffective disorder (N=31 [26%]), bipolar disorder (N=25 [21%]), or other major mood disorder (N=24 [20%]). The mean age at illness onset for patients was 16 years (SD=9); mean age at first hospitalization was 23 (SD=9). Study patients had an average of 13 (SD=14) lifetime hospitalizations and a cumulative lifetime average of 43 months (SD=70) of prior psychiatric hospitalization. Core interview-derived case mix variables rated at admission for the hospital and alternative study patients are shown in
table 1. Patient groups did not differ at the p<0.05 level on any variables studied.
Clinical Outcome
Length of stay for alternative-treated patients (mean=18.7 days, SD=13.8) was significantly longer than that for hospital-treated patients (mean=11.7 days, SD=8.2) (t=3.19, df=117, p<0.002, d=0.60). Repeated measures ANOVA that used total Positive and Negative Syndrome Scale score as the dependent variable indicated a statistically significant time effect (F=52.94, df=2,220, p<0.0001) but no significant treatment site effect (F=0.23, df=1,110, p=0.64) or treatment site-by-time interaction (F=1.18, df=2,220, p=0.31). Post hoc t tests showed that psychopathology for both hospitalized patients and patients treated in the residential alternative decreased significantly from admission (hospital mean=89, SD=25; alternative mean=87, SD=24) to discharge (hospital mean=69, SD=16 [t=8.53, df=48, p<<0.001]; alternative mean=72, SD=27 [t=6.29, df=67, p<0.001]), and the decrease was maintained at 6-month follow-up (hospital mean=69, SD=18; alternative mean=73, SD=22). No differences between hospital and the alternative were significant at p<0.05.
Mean total patient satisfaction with acute episode care did not differ between settings (hospital mean=5.1, SD=0.9; alternative mean=5.1, SD=0.8) (t=0.20, df=105, p=0.84). Of 10 areas rated, patient satisfaction differed significantly between settings on only one: alternative-treated patients were significantly more satisfied with facility-provided food (d=0.71). Effect sizes for the differences between groups on the other nine rated areas varied from 0.01 to 0.31.
Overall, 108 (91%) of 119 patients were stabilized during the treatment episode and returned to the community. Treatment failure rate (transfer to another inpatient facility) was nine (13%) of 69 in the alternative and two (4%) of 50 in the hospital (χ2=1.85, df=1, p=0.17). One-third (three of nine) alternative-treated patients requiring transfer accepted voluntary hospitalization; the remainder required involuntary commitment. No serious adverse events occurred among alternative-treated patients requiring transfer to an inpatient unit, beyond police intervention needed for commitment.
Ninety-five percent of patients (N=113 of 119) were located for follow-up interview. One patient (alternative-treated) died from suicide between discharge and follow-up.
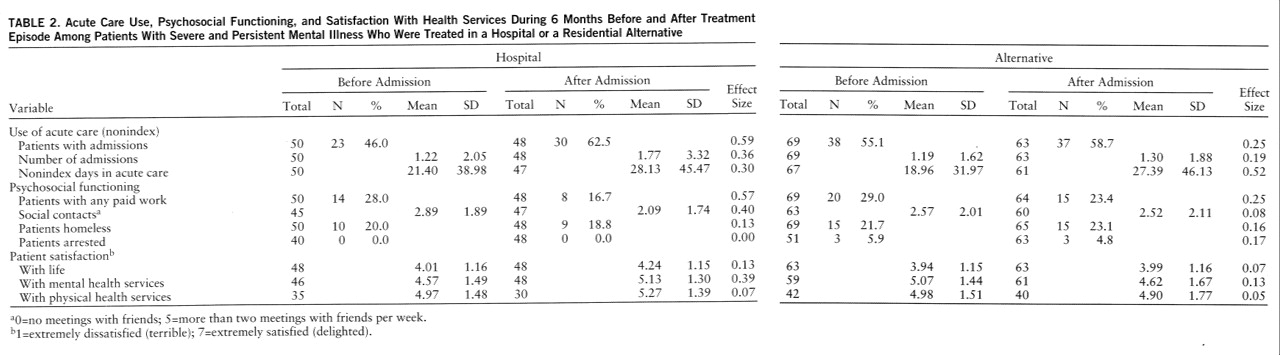
Table 2 shows acute care use, psychosocial functioning, and patient satisfaction over the 6 months before and after index admission. No main effects or interaction between time of assessment and treatment site were significant at Bonferroni-corrected alpha levels. Pairwise comparisons between the two treatment sites yielded effect sizes that varied between 0 and 0.35. Acute care use, psychosocial functioning, and satisfaction with one's life, mental health, and physical health services over the 6 months after admission, therefore, were comparable for patients treated in the hospital and the alternative.
DISCUSSION
Mental illnesses such as schizophrenia, schizoaffective disorder, and bipolar disorder are often recurrent, with exacerbations and remissions superimposed on varying degrees of prolonged disability. Care for patients with these severe disorders accounts for the use of nearly half (43%) of mental health resources, with the largest proportion of expenditures allocated to hospital inpatient care (
27). It is widely recognized that providing needed services to this population within budgetary constraints requires the management of costly inpatient utilization (
28,
29).
In this study, voluntary adult patients with severe and persistent mental illness and a history of multiple prior inpatient care episodes were prospectively assigned at the time of illness exacerbation to an acute psychiatric ward of a general hospital or an acute residential alternative program. Overall, 87% of patients receiving care in the alternative were successfully treated and returned to the community. This relatively low failure rate is consistent with those reported in other studies of alternatives to psychiatric hospitalization (
7,
12,
30–
32). Patient acceptance of the alternative acute care setting was good, as reflected in satisfaction ratings and a higher percentage of successful placements in the intention-to-treat group. Both episode and 6-month clinical outcome measured in the domains of symptom improvement, psychosocial functioning, acute care service utilization, and patient satisfaction were comparable for the hospital- and alternative-treated cohorts.
Using comprehensive cost estimation, Sledge et al. (
33,
34) recently described a model of acute care combining day hospital and residential respite care for voluntary patients that generated outcomes comparable to those of hospital care at a significantly lower operating cost. The crisis care model described here differs from that described by Sledge et al. in our use of an eight- rather than four-bed facility, the use of nonmedically trained crisis staff, and our reliance on ongoing community treatment resources rather than a day hospital to provide medical care and structure during the crisis episode. Charges alone are generally a poor reflection of costs and must be interpreted cautiously (
35,
36). Rates in Maryland are set by a Health Services Cost Review Commission through use of Health Care Financing Administration-like cost report methodology. The Health Services Cost Review Commission fiscal year 1993 per diem rate for the hospital was $384.00; the alternative treatment modality per diem rate was $123.29. Evaluation of total cost, however, is required to assess the costs of additional community services used by patients during a crisis episode (
37–
39).
It is not surprising that neither we nor Sledge et al. found that any acute care intervention had a significant impact on postepisode psychosocial functioning. In the 6 months following acute treatment, most patients resumed functioning at their precrisis episode level. Although extended hospitalizations were once employed to achieve improvements in social and vocational functioning, brief acute care is specifically aimed at crisis resolution. Thus, symptom reduction, return to the community, and patient satisfaction are likely the most important outcomes of acute care to evaluate. Contrariwise, outpatient and community support programs that target improved social and vocational functioning and relapse prevention as goals may be best assessed with measures of psychosocial functioning and rehospitalization.
The results reported here must be considered in light of this study's strengths and limitations. This investigation took place in a functioning mental health system in which both acute hospital and alternative services were in place before the study. The patient group was restricted to Medicaid and Medicare beneficiaries disabled by clearly documented severe and persistent mental illness characterized by repeated inpatient hospitalizations. For these reasons, findings should be broadly applicable to comparable patient populations in public mental health systems in other jurisdictions.
While the naturalistic setting of this study provides a favorable environment to test program model effectiveness, it also results in limitations. The necessity of obtaining patient consent may introduce a selection bias that cannot be measured. In addition to reflecting patient acceptance of this modality, the higher rate of post~randomization admissions to the alternative could reflect the alternative's more central location and faster admission process. Alternatively, the different admission rates may have reflected patients' experience-based preferences for the nonhospital acute care setting or other area inpatient facilities outside the scope of the study. Any biases due to self-selection, however, did not result in significant differences between successfully and unsuccessfully admitted patients on any of 27 demographic and clinical characteristics, and the randomization procedure produced comparable subject groups for the two treatment sites.
The generalizability of these findings to the uninsured or those with private third-party insurance has yet to be demonstrated. Furthermore, results reported here are clearly restricted to voluntarily admitted psychiatric patients not requiring detoxification or acute general medical intervention. In fiscal year 1993, 52 (10%) of 509 admissions among patients enrolled in the Mont~gomery County Department of Health and Human Services catchment area were involuntary.
Medicare and Medicaid are particularly important funding sources for adults with serious mental illnesses and have supported growth in the number of general hospital psychiatric units over the past two decades (
40,
41). During this same period community-based interventions of demonstrated efficacy have been developed (
42–
47), but reliable funding streams to support these technologies have been limited (
2,
47–
49). Current initiatives to limit public health expenditures involve the provision of fewer total dollars, but more local choice in allocating funds to competing services (
50). In this environment the use of new or underused technologies that are as effective as, but potentially less costly than, available treatments should receive priority (
51,
52).
Cost cutting replaces the risk of excessive hospitalization with the risk of undertreatment or of shifting the burden of acute care to families or the criminal justice system. While clearly not a substitute for all psychiatric hospital care (
11,
53), wider use of acute nonhospital residential alternatives may be crucial in maintaining a humane treatment infrastructure for psychiatry's most vulnerable patients in a future that will be characterized by shrinking resources. Our data suggest that a crisis residential alternative can be as effective as general hospital care for a wide range of patients with serious mental illness who do not require either acute detoxification or emergent medical evaluation and are willing to accept voluntary treatment.