Bipolar manic-depressive disorders are arguably the most prevalent idiopathic psychotic disorders, with the lifetime prevalence of mania now at 1.6% and the combined risks of bipolar type I syndrome (with mania) and type II syndrome (with hypomania) evidently above 2% (
1,
2). Bipolar II syndrome includes particularly severe, rapidly recurring, and treatment-resistant forms of depressive illness (
3–
8). Depression accounts for a high proportion of distress, comorbidity, and disability in all bipolar disorders and is strongly associated with suicidal behavior (
9,
10). Despite the clinical importance of bipolar depression, research on its treatment is surprisingly limited (
11–
15), and it has been routinely excluded from contemporary research on the therapeutics of depressive disorders (
16–
18). Research on lithium treatment has provided the most extensive information but has often included broadly defined manic-depressive disorders, without clear distinction of bipolar and unipolar forms or without direct comparison of mania and depression or of the bipolar subtypes under matching conditions (
16–
18).
Data from 10 studies cited elsewhere (
9,
18), involving over 700 patients given lithium maintenance treatment for periods averaging 1.5 years, provide comparisons of base rates and therapeutic effects for both depression and mania in bipolar I disorder and mainly for depression in bipolar II disorder. Of the type I patients in eight of these trials, before lithium or during placebo treatment, 59.7% (SD=24.6%) relapsed into mania and 40.8% (SD=14.5%) into depression, but during lithium maintenance only 23.6% (SD=20.9%) relapsed into mania and 22.6% (SD=13.3%) into depression. Without lithium, the risk for mania was thus 1.46 times greater than the risk for depression. With lithium, recurrences of mania fell by 2.53-fold, but depression decreased by only 1.81-fold. These findings suggest a somewhat superior reduction of mania with lithium, although nearly identical proportions of patients (23% and 24%) relapsed into mania and depression
during lithium treatment. A study of 29 bipolar I patients during a year of treatment (
5) also found a greater decrease in time spent in mania (from 20.0% to 8.1%; 2.47-fold) compared to the more prevalent depression (from 48.5% to 28.6%; 1.70-fold). Another study of 61 bipolar I patients (
19) found a similar pretreatment incidence of depression and mania but even greater benefits of lithium for depression by comparing risk rates (episodes per year): mania decreased from 0.50 to 0.20 (2.50-fold), and depression from 0.59 to 0.12 (4.92-fold). These several findings in bipolar I patients are thus inconsistent and not conclusive concerning the relative therapeutic impact of lithium on depression versus mania, although they suggest somewhat greater proportional decreases of mania but similar levels of depressive and manic illness during lithium treatment.
Among the few controlled studies evaluating bipolar II patients, three (
3,
4,
20) found only a moderate (1.60-fold) average decrease in relapses (mainly depressive), from 60.3% (SD=9.1%) of patients treated with a placebo to 37.7% (SD=32.6%) treated with lithium maintenance for a year. More encouraging results were found in at least five trials that provided recurrence rates, mainly of depression, for a total of 169 bipolar II patients maintained with lithium versus placebo (
3,
4,
20,
21) or during lithium maintenance versus before (
22) in observation periods averaging 13.6 months (SD=7.3). Morbidity averaged 1.01 (SD=0.566) affective episodes per patient-year without lithium versus 0.263 (SD=0.203) during lithium maintenance treatment, indicating a large (3.84-fold) reduction. Although this research is limited, the results suggest that lithium has substantial beneficial effects against recurrences in bipolar II disorder, and that these may even be superior to those against bipolar depression in the bipolar I syndrome.
Conclusions from studies of lithium in bipolar I and bipolar II disorders remain tentative, since direct comparisons of morbidity in the diagnostic subtypes were rare, and since depression and mania were not always examined separately. Moreover, methods of measuring morbidity have varied, with episode rates often considered rather than the proportion of time ill. Recent American Psychiatric Association treatment guidelines (
23) and an APA-sponsored survey (
24) concluded that clinical experts consider lithium to be a drug of choice in the long-term maintenance therapy of both depressive and manic phases of bipolar I and bipolar II syndromes. However, research evidence supporting the relative value of lithium in the syndrome subtypes, as well as for bipolar depression versus mania or hypomania, remains limited and largely inconclusive (
9,
11,
15,
18,
23–
26). These considerations encourage further clarification of the relative benefits of lithium in the diagnostic subtypes and phases of bipolar illness, with direct comparisons under similar conditions and with substantial numbers of bipolar I and bipolar II patients.
Accordingly, we studied 317 patients with bipolar I or bipolar II disorders who were followed prospectively during long-term lithium maintenance, with detailed information on their course of illness before and during treatment. Specific hypotheses for this study, arising from the findings just reviewed, were that 1) lithium treatment is associated with a greater reduction in mania or hypomania in both type I and type II bipolar disorders, 2) the amounts of time spent in mania/hypomania and in depression during lithium treatment are similar, and 3) in general, not only is bipolar II disorder not a milder form of bipolar illness, but benefits of lithium maintenance treatment are superior in that syndrome.
METHOD
Adult patient-subjects were evaluated while undergoing clinical maintenance treatment with lithium carbonate and follow-up at the university-affiliated Lucio Bini mood disorders research center in Cagliari, Sardinia. Confidentiality was assured, and patients provided written informed consent for such anonymous use of their clinical records, with approval of the study by the institutional review board of McLean Hospital, Belmont, Mass., and corresponding officials of the University of Cagliari medical center. The 317 subjects (65.6% of whom were women) included 188 patients with type I and 129 patients with type II bipolar disorder based on rediagnosis by DSM-IV criteria, which were also used to define affective episodes (
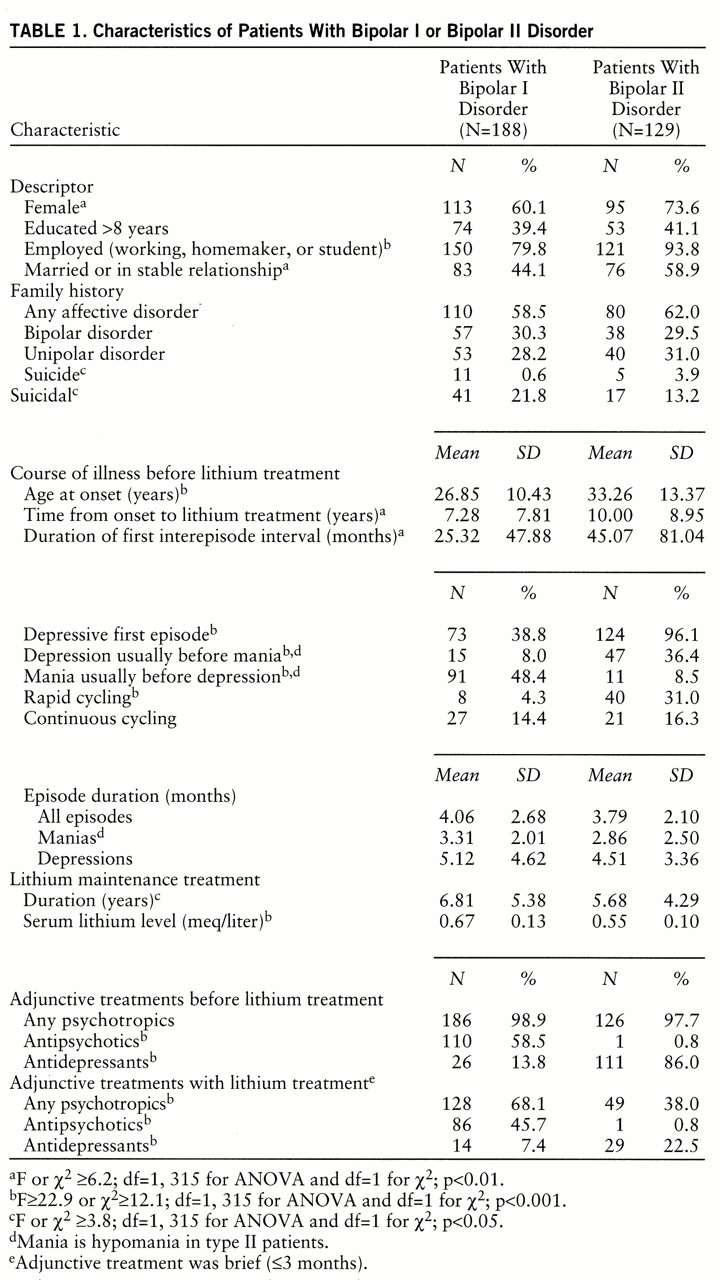
table 1). Excluded were patients who had been exposed to antidepressant or antipsychotic drugs other than for brief treatment of breakthrough symptoms (≤12 weeks) and those receiving long-term anticonvulsant treatment or abusing drugs or alcohol.
Clinical assessments by research psychiatrists at the clinical center (L.T. and G.F.) in follow-up visits (four to 12 per year) were recorded on research data forms and life charts to document treatments (type, doses, and duration of use of psychotropic and other agents) and the course of affective illness (
27–
29). Demographic data included sex, birth date, level of education, employment, and marital status. Clinical data included diagnostic type, family history of affective disorders in first-degree relatives, age at onset, polarity of the first episode, number and duration of depressive episodes before a first manic (bipolar I) or hypomanic (bipolar II) episode, length of first interepisode interval, number and duration of all episodes of mania or depression, majority sequence of episode polarities (either mania before depression or the opposite) (
11,
30), time from illness onset to starting maintenance treatment, hospitalizations, suicide attempts, doses and the average of approximately semiannually ascertained serum concentrations of lithium, and use of adjunctive treatments (tables
1 and
2).
This information yielded morbidity rates as manic or depressive episodes or hospitalizations per year and percentage of time in DSM-IV-defined mania (hypomania in type II cases) or depression before and during lithium maintenance treatment. Statistical analysis used paired t tests or analysis of variance (ANOVA) for unpaired continuous data; categorical data were compared by contingency tables (chi-square). Kaplan-Meier survival analysis (
31) was used to plot time to recurrence and compute time-to-50%-recurrence risk with variance as standard error; correlations were tested by linear regression (r) or nonparametric regression (r
s)—all as reported previously (
27,
28). Significance was set at p<0.05 in two-tailed tests at defined degrees of freedom. Multivariate linear regression analyses were used to assess factors associated with response to lithium maintenance treatment, as defined by the difference in percentage of time ill before lithium treatment minus the percentage during lithium treatment, and modeling total affective morbidity, mania, and depression separately.
Demographic, clinical, and treatment variables were first considered in bivariate analyses for association with the overall treatment effect, and those suggesting an association (p<0.10) were included in multivariate analyses; distributions of these proposed variables were first tested for distribution normality and to verify that normalizing data transformations were not needed. Partial residual and influence plots did not identify outlier observations that might unduly influence reported models. Deciles-of-risk and partial-residual-plot methods (
32) validated the goodness of fit of multivariate models. In the reported models, explanatory variables with regression coefficients (beta) statistically different (p<0.05) from 0 were considered valid explanatory factors associated with treatment responses, and they are reported with their 95% confidence intervals and associated t and p values.
DISCUSSION
This clinical study had limitations in that it was not double-blind or placebo-controlled, nor were short-term adjunctive treatments strictly excluded during observation of lithium as the maintenance monotherapy. However, the observations represent clinically realistic conditions in which the long-term effectiveness of maintenance treatment with lithium could be evaluated, and the inclusion of persons who required brief supplemental treatments avoided an excessively biased selection of highly lithium-responsive patients. Moreover, the design of the study was comparative, such that effects of treatment in the diagnostic subtypes and in both phases of bipolar illness were evaluated under comparable conditions. It would be unrealistic and unethical to attempt blind and random assignment of patients to more than 5 years of placebo treatment in such life-threatening and highly morbid conditions, and introduction of a placebo itself may complicate treatment studies by adding an iatrogenic contribution to the risk of early relapse because of the evident pharmacodynamic stress associated with discontinuation of treatment (
27,
28,
33–
35). Moreover, recruitment into controlled studies now risks overinclusion of treatment-resistant subjects (
17,
36–
38).
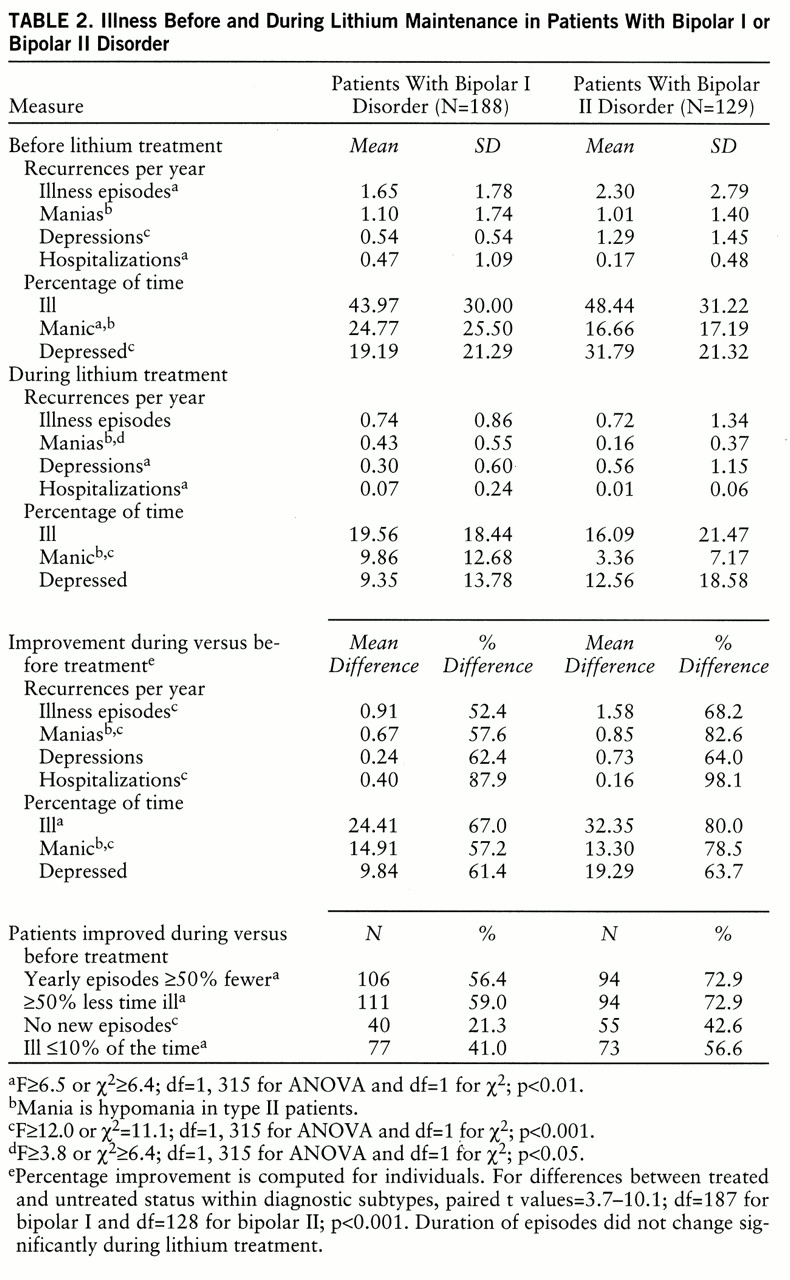
Various measures of morbidity and course of illness before sustained lithium maintenance in the present study accord well with previous reports, including those involving placebo treatment under double-blind conditions. For example, studies reviewed above (
3,
4,
20–
22) indicated an average recurrence risk of 1.05 (SD=0.64) episodes per patient-year in 67 bipolar II patients treated with placebo and 0.26 episodes (SD=0.20) during lithium treatment of 169 bipolar II patients. The present findings indicate similar or even slightly greater risks of recurrence: 1.29 versus 0.56 depressive episodes per patient-year in 129 bipolar II subjects before versus during lithium treatment (
table 2), suggesting that the present methods did not underestimate morbidity.
This study yields several findings of clinical and research interest. First, although some uncertainty about the significance of a distinction between bipolar subtypes remains, they have been found to differ in several clinical factors, with apparent long-term diagnostic stability (
2,
6,
39–
41), and the bipolar II syndrome appears to be distinct from recurring nonbipolar depression (
2,
7,
15,
39–
41). The present findings also strongly support a clinical distinction between the bipolar I and bipolar II subtypes, with several statistically robust and clinically important differences between them (tables
1 and
2).
In the present results, cases of bipolar II disorder included a higher proportion of women, later age at onset, greater likelihood that the patient was married and employed, and a longer time before the start of lithium maintenance. Bipolar II patients also had first-degree relatives with a greater risk of suicide but were only slightly less likely than bipolar I patients to be suicidal themselves. The course of bipolar illness also differed markedly between subtypes: bipolar II patients more often presented with a depressive episode first, had more depressive-before-manic episodes, and predominantly followed a depression-before-mania course sequence (
11,
30). Bipolar II patients were also much more likely to show rapid cycling in association with a higher average annual attack frequency; they also had many more depressive episodes per year and spent more time in depression than bipolar I patients before lithium treatment. Although bipolar II subjects were less often hospitalized than bipolar I subjects before lithium treatment started, this difference may reflect response to dangerous or antisocial behaviors associated with bipolar I mania. However, bipolar II syndrome is probably not appreciably less life-threatening than bipolar I disorder, since suicidal behavior is strongly associated with depression in bipolar illnesses, and rates of life-threatening acts were shown to be similar among both bipolar types in a Sardinian population (
9) and were only somewhat less frequent in the present bipolar II study group (
table 1). In general, in accord with our hypothesis 3, it is evidently neither valid nor clinically prudent to assume that bipolar II syndrome is merely a mild form of bipolar illness.
In the previous studies of manic and depressive phases in bipolar syndromes reviewed above, there was evidence of beneficial effects of lithium for both mania and depression in type I patients and for mainly depressive episodes in bipolar II patients (
3,
4,
10,
15,
17,
19–
22). Such controlled lithium trials, typically lasting for 1–2 years, had suggested substantial improvement of depression as well as mania in bipolar I disorder and of depression in bipolar II syndrome. Typically, there was a somewhat greater proportional decrease of mania than of depression in bipolar I patients, but the findings suggested a similar morbid risk or percentage of time spent in both manic and depressive phases of bipolar I illness
during lithium maintenance. The present findings are strikingly congruent with those earlier findings, they extend observations to nearly 10 years of follow-up, and they strongly support our hypotheses 1 and 2. That is, the reduction in episodes per year or percentage of time ill was somewhat greater in mania than in depression among bipolar I patients, but the absolute risk and proportion of time ill in mania and depression during lithium maintenance treatment were indistinguishable (
table 2).
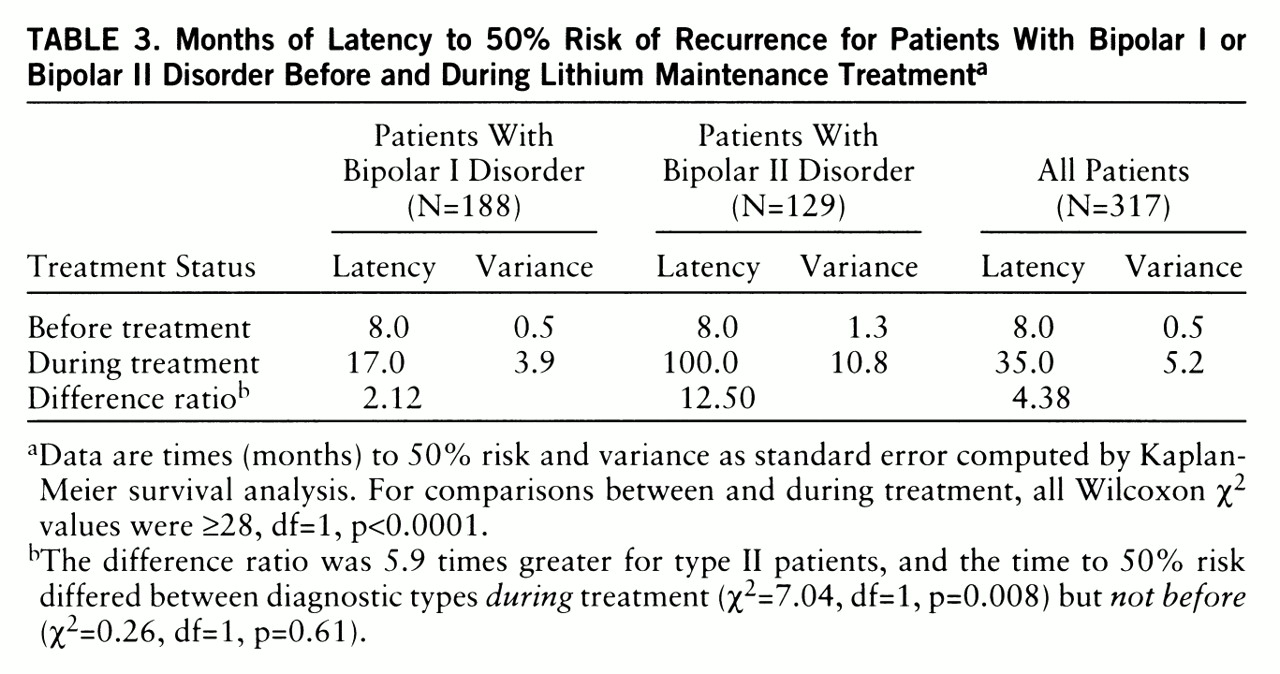
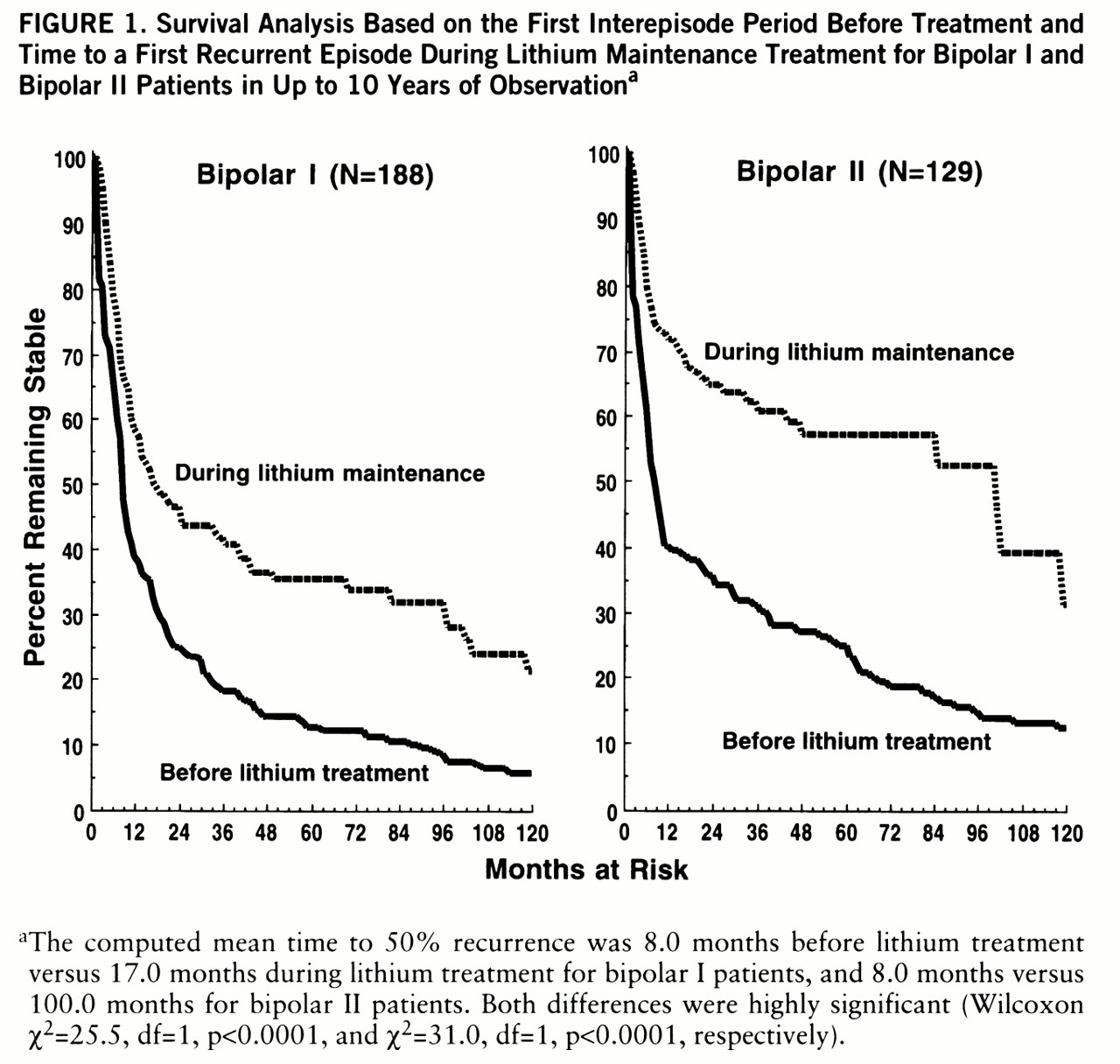
There were significant differences in responses to lithium in the bipolar subtypes, with strong indications of greater responsiveness to lithium in the type II syndrome. These differences include a longer period of euthymia between episodes (
figure 1) and a markedly greater proportional reduction in episodes or percentage of time ill in bipolar II illness, as well as in other comparative measures of the sparing of morbidity (
table 2). Reductions in the frequency of depressive episodes and in the total percentage of time ill in bipolar II subjects also exceeded these benefits in bipolar I subjects (
table 2). However, depressive morbidity—as both episode frequency and time in depression—in the type II syndrome was markedly higher before lithium treatment, and it also tended to remain somewhat greater in these cases during lithium maintenance (
table 2). These findings underscore the urgent need for improved treatment of bipolar depression and its consideration in experimental therapeutic investigations of depressive disorders.
The average serum concentrations of lithium reported (0.55–0.67 meq/liter) (
table 1) may seem low by recent American dosing recommendations, which have encouraged use of lithium routinely at serum levels above 0.75 meq/liter (
15,
17,
34,
42,
43). The dosing in the present study may, to some extent, reflect selection of patients who were compliant with long-term lithium maintenance and exclusion of potential poor-prognosis patients with comorbid substance abuse or with schizoaffective disorders, who appear in other studies. Nevertheless, the lithium levels we used are consistent with contemporary international practice and with research findings on prospectively determined relationships between lithium blood level and response in bipolar disorders (
16,
21,
44). A provocative possibility is that there may be a trade-off between marginally increased morbid risks associated with flexible and moderate dosing with lithium versus long-term gains due to increased adherence to recommended maintenance treatment.
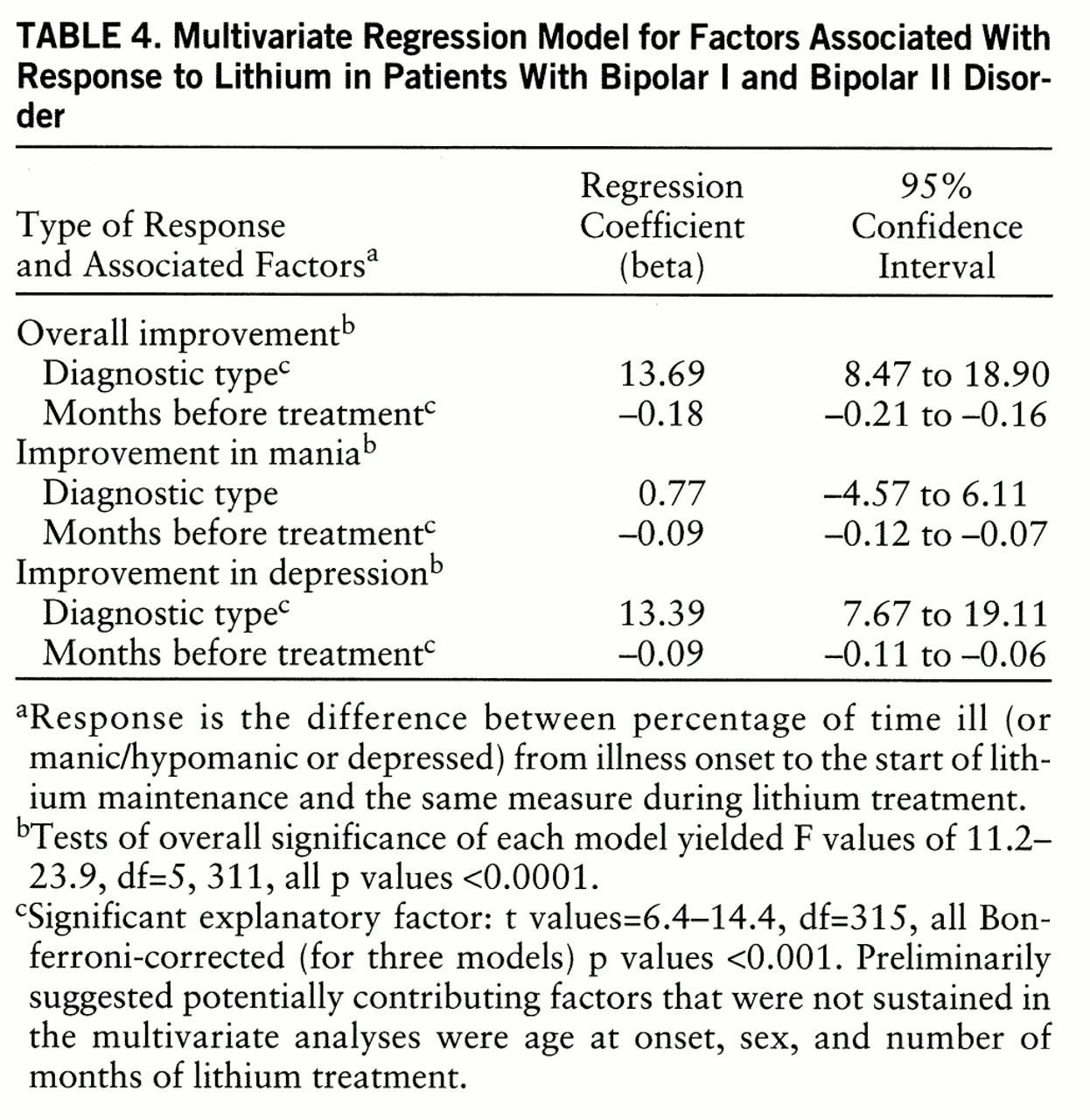
In general, the present comparisons of bipolar diagnostic types indicate that the benefits of lithium maintenance were superior in type II cases. Recurrences of both depression and mania (or bipolar II hypomania) and the amount of time in each state were markedly reduced with lithium treatment in both diagnostic subtypes, although episode duration was not altered appreciably (
table 1). However, the current findings do not represent treatment effectiveness in all candidates for lithium therapy: many patients with bipolar or schizoaffective disorders—particularly those now available for study at research centers—do not do well with lithium monotherapy, and many others refuse to consider it or fail to remain compliant with recommended doses (
17,
38). High rates of apparent treatment failure have been documented in several recent surveys, typically based on clinically complex samples in urban teaching centers (
38,
45–
50). However, these have usually focused on the presence of recurrences rather than on reduction of morbidity and mortality, and their results are not consistently worse than those in the present study. For example, our overall failure rate was 36.2% after 1 year of lithium maintenance, which is in the midrange of other comparable recent U.S. studies with rates of 17%–48% (
43,
49,
50). The present findings are consistent with other such studies in indicating that complete prevention of attacks of mania or depression in bipolar disorders is unlikely with any available treatment (
15–
17,
36). However, they also document the rather remarkable effectiveness of primary lithium maintenance treatment, with occasional short-term supplementation, in limiting long-term morbidity due to recurrences of life-threatening depression as well as potentially dangerous mania or hypomania in both type I and type II bipolar disorders. Finally, the present results add strong evidence to the view that longer delay in initiating sustained lithium maintenance treatment is associated with lesser reductions in morbidity during eventual treatment (
table 4) and so encourage early intervention (
18,
23).