Preliminary Analyses
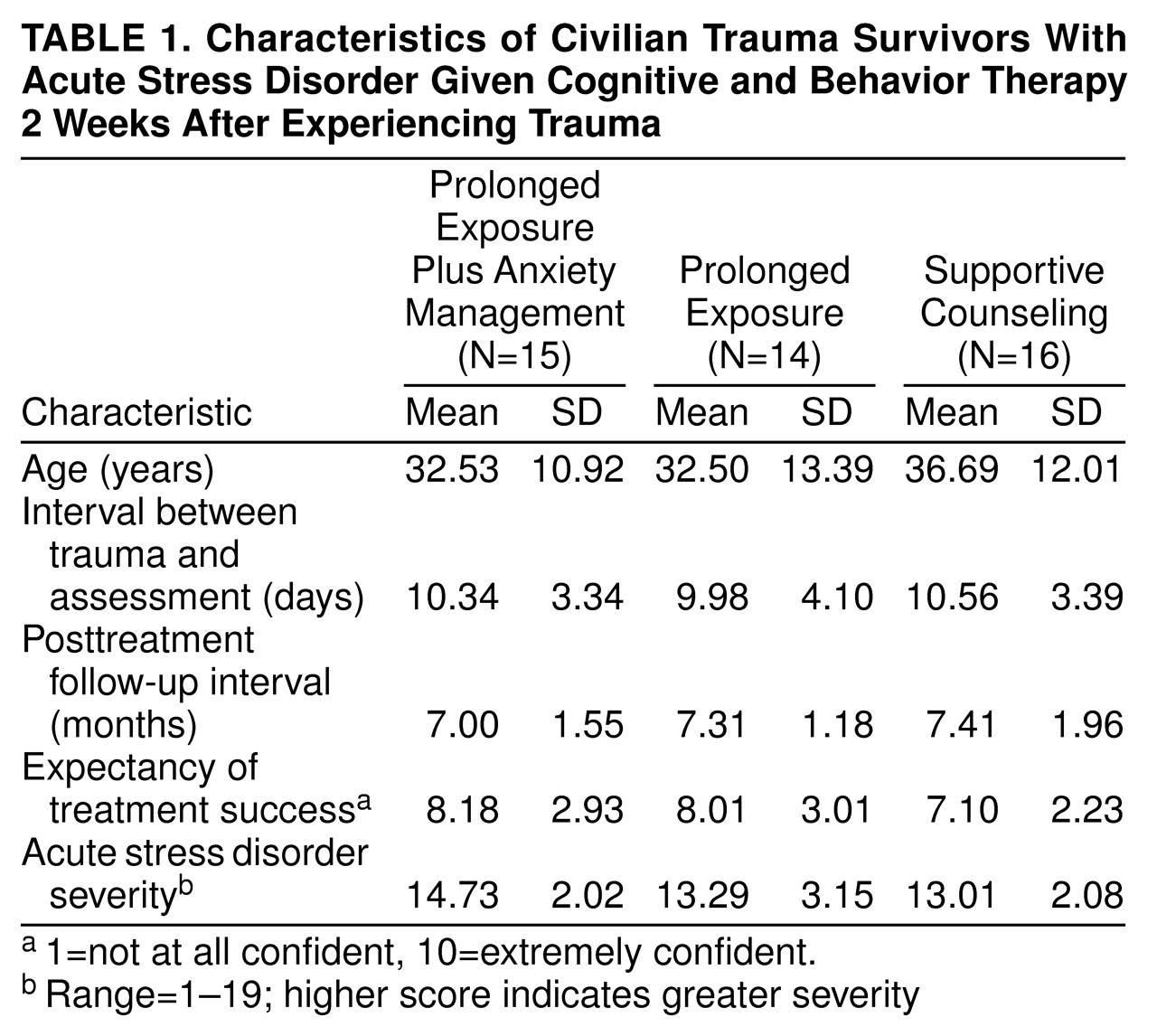
The seven patients who displayed two acute dissociative symptoms of stress disorder did not differ from patients who displayed the required three dissociative symptoms on any pretreatment measures, including the Impact of Event Scale, the State-Trait Anxiety Inventory, and the Beck Depression Inventory. That is, these patients displayed comparable levels of acute psychopathology as those who met the full criteria. The 11 patients who dropped out of treatment differed from those who completed treatment in terms of the severity of their acute stress disorder (F=2.48, df=2, 54, p<0.05) and their State-Trait Anxiety Inventory scores for state anxiety (F=3.55, df=2, 64, p<0.01). That is, those who dropped out of treatment reported more severe acute stress disorder and higher scores for state anxiety than those who completed therapy. Of the 45 patients who completed treatment, four (two in prolonged exposure plus anxiety management, one in prolonged exposure, and one in supportive counseling) were not included in the follow-up assessment because two could not be contacted and two were instructed by legal counsel not to participate.
Diagnostic Status
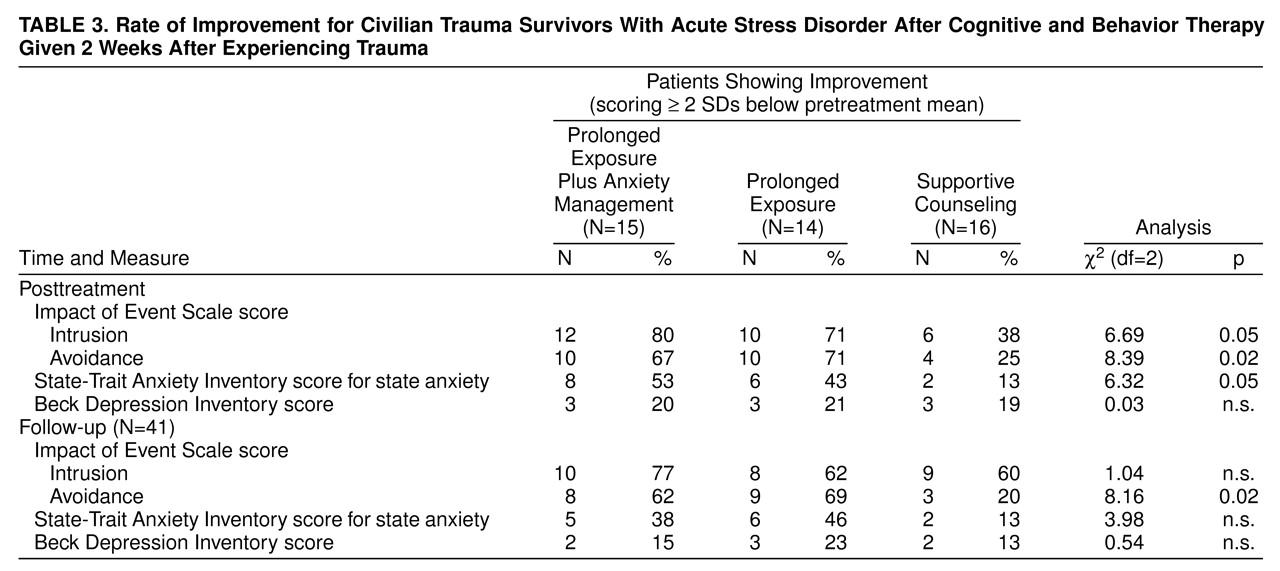
McNemar’s chi-square tests indicated that at posttreatment, fewer patients in the prolonged exposure plus anxiety management group (20%, N=3 of 15) and the prolonged exposure group (14%, N=2 of 14) met the criteria for PTSD than in the supportive counseling group (56%, N=9 of 16) (χ
2=7.43, N=45, df=2, p<0.05, with Yates’s correction
[21]). Paired chi-square comparisons indicated that more patients in the supportive counseling group met the criteria for PTSD than in the prolonged exposure plus anxiety management group (χ
2=4.27, N=31, df=1, p<0.05, with Yates’s correction) and in the prolonged exposure group (χ
2=5.54, N=30, df=1, p<0.02, with Yates’s correction). Similarly, at the 6-month follow-up, fewer patients in the prolonged exposure plus anxiety management (23%, N=3 of 13) and prolonged exposure (15%, N=2 of 13) groups met the criteria for PTSD than in the supportive counseling group (67%, N=10 of 15) (χ
2=9.39, N=41, df=2, p<0.01, with Yates’s correction). Paired chi-square comparisons indicated that more patients in the supportive counseling group met the criteria for PTSD than in the prolonged exposure plus anxiety management group (χ
2=5.36, N=28, df=1, p<0.05, with Yates’s correction) and in the prolonged exposure group (χ
2=7.59, N=28, df=1, p<0.01, with Yates’s correction).
Posttraumatic Stress Severity
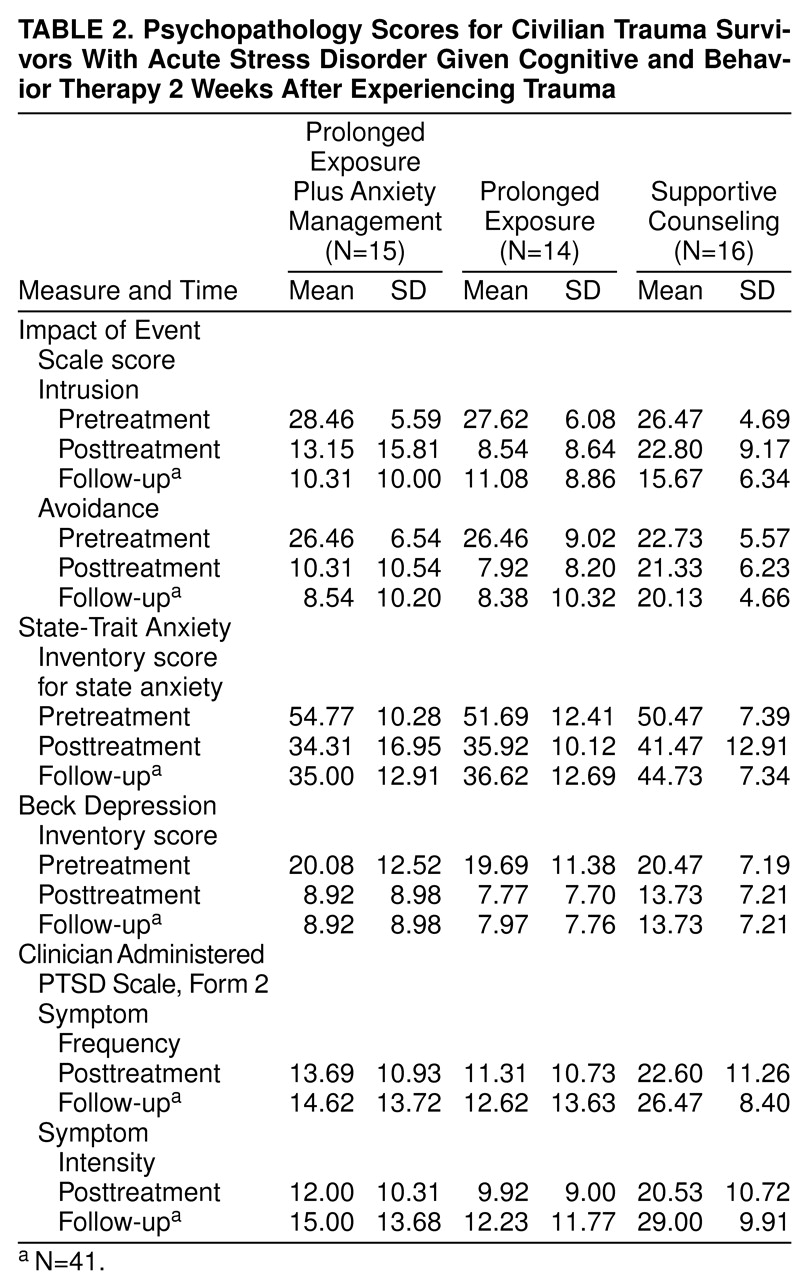
A series of three-(group) by-three (assessment), repeated-measures ANOVAs were conducted on Impact of Event Scale, State-Trait Anxiety Inventory, and Beck Depression Inventory scores (
table 2). Post hoc Tukey comparisons were conducted with an adjusted alpha rate of 0.01 to provide an overall significance level of 0.05. A three-by-three, repeated-measures ANOVA on Impact of Event Scale scores for instruction indicated a significant main effect for time (F=56.05, df=2, 37, p<0.001) and a significant group-by-time interaction effect (F=5.03, df=4, 76, p<0.001). Post hoc Tukey comparisons indicated that patients reported higher Impact of Event Scale scores for intrusion at time 1 than at times 2 and 3. When we used post hoc t tests, patients in supportive counseling reported higher Impact of Event Scale scores for intrusion at posttreatment than did patients with prolonged exposure (t=4.08, df=28, p<0.001).
A three-by-three, repeated-measures ANOVA on Impact of Event Scale avoidance scores indicated a significant main effect for time (F=26.78, df=2, 37, p<0.001) and a significant group-by-time interaction effect (F=2.98, df=4, 76, p<0.05). Post hoc comparisons indicated that patients reported higher Impact of Event Scale avoidance scores at time 1 than at times 2 and 3. Further, supportive counseling patients displayed higher Impact of Event Scale scores for avoidance at the 6-month follow-up than both the patients with prolonged exposure plus anxiety management (t=3.91, df=26, p<0.01) and the patients with prolonged exposure (t=11.75, df=26, p<0.001).
A three-by-three, repeated-measures ANOVA on State-Trait Anxiety Inventory scores for state anxiety indicated a significant main effect for time (F=29.45, df=2, 37, p<0.001) and a significant group-by-time interaction effect (F=2.58, df=4, 76, p<0.05). Post hoc comparisons indicated that patients reported higher State-Trait Anxiety Inventory scores for state anxiety at time 1 than at times 2 and 3. The supportive counseling patients displayed only marginally higher State-Trait Anxiety Inventory scores for state anxiety at the 6-month follow-up than both the patients with prolonged exposure plus anxiety management (t=2.50, df=26, p<0.02) and the patients with prolonged exposure (t=2.08, df=26, p<0.05).
A three-by-three, repeated-measures ANOVA on Beck Depression Inventory scores indicated a significant main effect for time (F=19.95, df=2, 37, p<0.001). Post hoc comparisons indicated that patients reported higher Beck Depression Inventory scores at time 1 than at times 2 and 3.
Separate three-by-two, repeated-measures ANOVAs were also conducted on Clinician Administered PTSD Scale, Form 2, scores for intensity and frequency; the Clinician Administered PTSD Scale, Form 2, scores were obtained only after treatment and at follow-up. A three-by-two, repeated-measures ANOVA of Clinician Administered PTSD Scale, Form 2, scores for intensity indicated significant main effects for time (F=8.26, df=1, 38, p<0.01) and group (F=8.07, df=2, 38, p<0.001). Patients reported lower scores for intensity after treatment than at follow-up. The supportive counseling patients reported higher scores for intensity than did the patients with prolonged exposure (t=4.09, df=26, p<0.001) and the patients with prolonged exposure plus anxiety management (t=3.13, df=26, p<0.01). A three-by-two, repeated-measures ANOVA of Clinician Administered PTSD Scale, Form 2, scores for frequency indicated a significant main effect for group (F=4.18, df=2, 38, p<0.05). Post hoc comparisons indicated that supportive counseling patients reported higher scores for frequency than did the patients with prolonged exposure (t=3.48, df=26, p<0.01) and the patients with prolonged exposure plus anxiety management (t=3.13, df=26, p<0.01).