Posttraumatic stress disorder (PTSD) is a pervasive and devastating anxiety disorder, the lifetime prevalence of which, as assessed in several community-based studies, is estimated at 3%–8%
(1,
2). These high prevalence rates, along with findings from recent studies, clearly indicate that PTSD can follow the experiencing of any major, life-threatening trauma, such as rape, physical assault, natural and industrial disasters, or traffic accidents. On the other hand, it is also well known today that exposure to trauma in itself is not sufficient for subsequent development of PTSD. Only low to moderate proportions of subjects exposed to trauma develop PTSD (e.g., 15.2% of Vietnam veterans
[3], 23.6% of young urban adults
[4], and 39% of traffic accident victims
[5]). Moreover, the traumatic symptoms may at times improve or disappear altogether within a few months after the traumatic event, suggesting a self-limited process similar to spontaneous recovery from a depressive episode
(6). The relative lack of knowledge about the nature of the relationship between PTSD and the traumatic stressor, and about the course of PTSD development, has refocused the attention of clinicians and researchers on the early course of PTSD, around and immediately after the exposure to trauma.
This renewed interest has led to numerous hypotheses about the possible interplay among pretraumatic vulnerabilities, objective and perceived trauma characteristics, and initial stress reactions in their contribution to the development of PTSD
(7,
8). From a diagnostic point of view, this is reflected also by the introduction of acute stress disorder in DSM-IV. The essential diagnostic criterion of acute stress disorder, differentiating it from PTSD, is its temporal limitation to the first 4 weeks following exposure to trauma (criterion G). Otherwise, except for the addition of dissociative symptoms (criterion B), it shares with PTSD symptoms of reexperiencing, avoidance, and hyperarousal. A key question arising from the inclusion of acute stress disorder in DSM-IV concerns the degree to which it predicts later PTSD. To date, however, little prospective research has been conducted in order to assess the relationship between acute stress disorder and PTSD, as well as the validity of 1 month as the critical time in the transition from the former to the latter.
Longitudinal studies, starting immediately after exposure to the trauma and using repeated assessments at multiple points in time, are critically important for the illumination of the developmental course of PTSD. Moreover, this approach may be helpful in choosing between the two major alternative hypotheses regarding the relationship between acute stress reaction and PTSD: The first views PTSD as a failure to extinguish acute stress reaction, which is a normal, straightforward response to abnormal circumstances
(9). The second claims that PTSD is, in fact, an abnormal response to traumatic events, not necessarily extreme in nature, occurring in predisposed individuals
(10).
While not directly addressing the natural course of posttraumatic symptom formation, previously published prospective studies on trauma survivors significantly contributed to identification of risk factors and predictors of PTSD. Low socioeconomic and educational status, prior traumatization, previous axis I morbidity, and personality traits such as neuroticism
(7,
11,
12) were identified as pretraumatic risk factors for PTSD. Perception of a direct threat to life
(5), peritraumatic dissociation
(8), and severity of physical injury
(5,
13,
14), on the other hand, were each found to be significant peritraumatic predictors of PTSD.
Traffic accidents have emerged in recent years as a major cause of psychiatric morbidity in general
(15,
16)and of PTSD in particular
(5,
16,
17). In fact, motor vehicle accidents have been found to be the single leading cause of PTSD in the general population
(18). Studies have shown that while acute stress symptoms exhibited by most traffic accident victims resolve within a few weeks, a significant portion of these subjects (10%–30%) still display PTSD symptoms 6 to 18 months after the accident
(5,
17). Consistent with findings from prospective research on other traumatized populations, perceived threat to life and severity of physical injury were found to be the strongest and most reliable predictors of PTSD in traffic accident victims
(5).
The present study was designed to assess, prospectively, the relationship between acute stress symptoms following exposure to trauma and the later development of PTSD. More specifically, our aims were to replicate previous estimates of PTSD prevalence in injured victims of traffic accidents and, more important, to delineate the developmental course of posttraumatic stress symptoms, as well as to identify the critical point in time in the transition from acute stress reaction to PTSD. In order to achieve these goals, posttraumatic symptoms were repeatedly assessed at five points in time during the first year following trauma. The formal diagnosis of acute stress disorder was not used in this study because it was designed and carried out before the introduction of DSM-IV. However, acute stress disorder key symptoms were assessed. The population of injured traffic accident victims was chosen because of its availability for immediate assessment soon after exposure to trauma.
METHOD
Participants
Participants included 99 traffic accident victims and 21 comparison subjects, who were followed up for 1 year between 1993 and 1996. All participants were recruited from three orthopedic wards (Rambam and Afula Medical Centers) to which they were admitted for medical care of their injuries, or elective surgery in the case of the comparison group. The elective surgery group was selected in order to control for possible hospitalization effects. All participants gave written informed consent after receiving a detailed explanation of the purpose and design of the study. Participants were considered eligible for the study group (traffic accident victims) if they were between the ages of 18 and 65 and had sustained mild to moderate physical injury because of traffic accidents, requiring hospitalization of at least 2 days. Participants were excluded if they had sustained head injury or showed evidence of brain damage, were in a coma or unconscious for more than 10 minutes before or during their emergency room admission, were actively treated for psychiatric disorder at the time of the accident, or were unable to communicate fluently in Hebrew. Screening for gross cognitive deficits was performed by using the Mini-Mental State examination
(19).
The resultant group of traffic accident victims consisted of relatively young (mean age=27.5 years, SD=10.0), predominantly male (66.7%), Jewish (88.8%) individuals, fairly well educated (mean=12.3 years, SD=2.1) and from middle socioeconomic class backgrounds, as measured by their housing conditions (i.e., number of rooms per person) (mean=1.1 rooms, SD=0.7). The elective surgery subjects were slightly, but not significantly, older and more educated than the traffic accident victims. They averaged 32.0 years of age (SD=13.7) and had an average of 13.3 years of formal education (SD=2.3).
Procedure and Measures
Initial evaluation took place within the first week of hospitalization after the accident. Participants were asked to answer questions regarding their personal background (e.g., family status, country of origin, level of education) and to rate their experience of the traumatic event on several key dimensions, such as helplessness, loss of control, and perceived threat to life. In addition, an extensive battery of self-report questionnaires was administered, covering areas such as PTSD and general psychiatric symptoms, pain severity, quality of sleep, work and social adjustment, and life events. This battery was repeated with the traffic accident victims 1, 3, 6, and 12 months after the accident and 3 and 12 months after surgery in the case of the comparison group. Because this article’s focus is on the relationship between early stress symptoms and later development of PTSD, findings related to some of these measures will be reported elsewhere.
Severity of physical injury was assessed through use of the Abbreviated Injury Scale
(20). Abbreviated Injury Scale ratings were determined by a surgeon experienced with traumatic injuries on the basis of examination of the patient and the medical records. Ratings between 0 and 6 were given for injuries to seven bodily areas and were then summed.
In order to assess PTSD symptoms, the Impact of Event Scale
(21) and the DSM-III-R Scale for Severity of PTSD Symptomatology
(22) were used. Because these scales have been used in previous studies of PTSD, they will not be described here. A broader spectrum of psychiatric symptoms was evaluated through use of the SCL-90
(23). Levels of general psychosocial and environmental stress in the year before and year after the accident were assessed with the Abbreviated Life Event Questionnaire
(24). Both weighted (by severity of event) and simple life change unit scores were calculated.
At 12 months, the Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP)
(25) was administered in order to reach a formal DSM-III-R diagnosis for PTSD. All participants were interviewed by an experienced clinical psychologist (I.A.) trained in the use of the SCID-NP. In addition to PTSD diagnosis, current and lifetime diagnoses (before and after the traffic accident) of the various DSM-III-R axis I disorders covered by the SCID-NP were determined as well. In order to ensure independence of PTSD diagnosis at 1 year from PTSD symptom measures collected earlier, the SCID-NP interviewer did not have access to the data collected at earlier time points.
Data Analysis
In order to examine relationships between continuous demographic and accident-related characteristics and the presence or absence of PTSD, a set of one-way univariate analyses of variance (ANOVAs) was performed (PROC GLM)
(26). Chi-square tests were used for categorical variables (PROC FREQ)
(26).
In order to compare the overall longitudinal pattern of clinical scale scores among the PTSD, non-PTSD, and comparison groups, a set of multivariate repeated measures ANOVAs (MANOVAs) (PROC GLM)
(26) was used. Comparisons between successive points in time were performed by using the profile transformation. One-way univariate ANOVAs with Tukey post hoc tests were performed separately for individual points in time, only in the presence of a significant multivariate effect (alpha=0.05). This conservative approach to data analysis reduced the likelihood of a type I error.
Approximately 12% of the data on the clinical psychometric scales were missing because of logistical constraints. In order to apply multivariate techniques while retaining a reasonable group size, we input missing data points on the individual scale scores by setting them equal to the overall group means for that point in time. A set of t tests was used to ascertain that the data were missing in a random fashion in regard to criterion variables such as age, education, socioeconomic status, and clinical scale scores.
In order to assess the stability of posttraumatic symptoms over the various points in time, a set of within-measure correlations, between successive points in time and between each point in time and 1 year, was computed. Finally, in order to assess which variables best predict PTSD diagnosis at 1 year, a set of logistic regression analyses (PROC LOGISTIC)
(26), with PTSD status as the dependent variable, was used.
RESULTS
PTSD 1 Year After the Accident
Seventy-four (75%) of the 99 traffic accident victims (who were mildly to moderately injured) and 19 (91%) of the 21 comparison subjects who initially volunteered to participate in the study completed the full 1-year follow-up. Twenty-four (32%) of the 74 traffic accident victims met DSM-III-R criteria for PTSD at the 12-month SCID-NP assessment, and 50 did not. None of the 19 comparison subjects was diagnosed with PTSD at the 1-year evaluation.
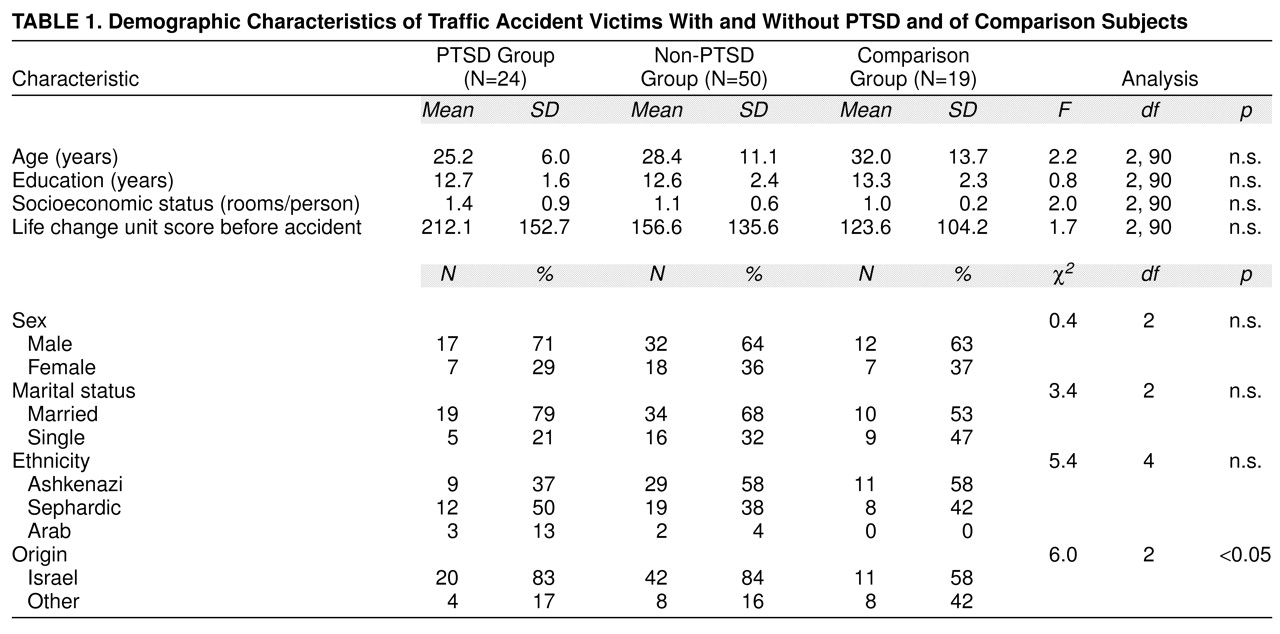
The three groups (i.e., traffic accident victims with and without PTSD and comparison subjects) did not differ significantly on any of the sociodemographic measures, such as age, gender, marital status, ethnicity, reported level of education, and socioeconomic status, as well as on amount or severity of life events in the year before the accident (
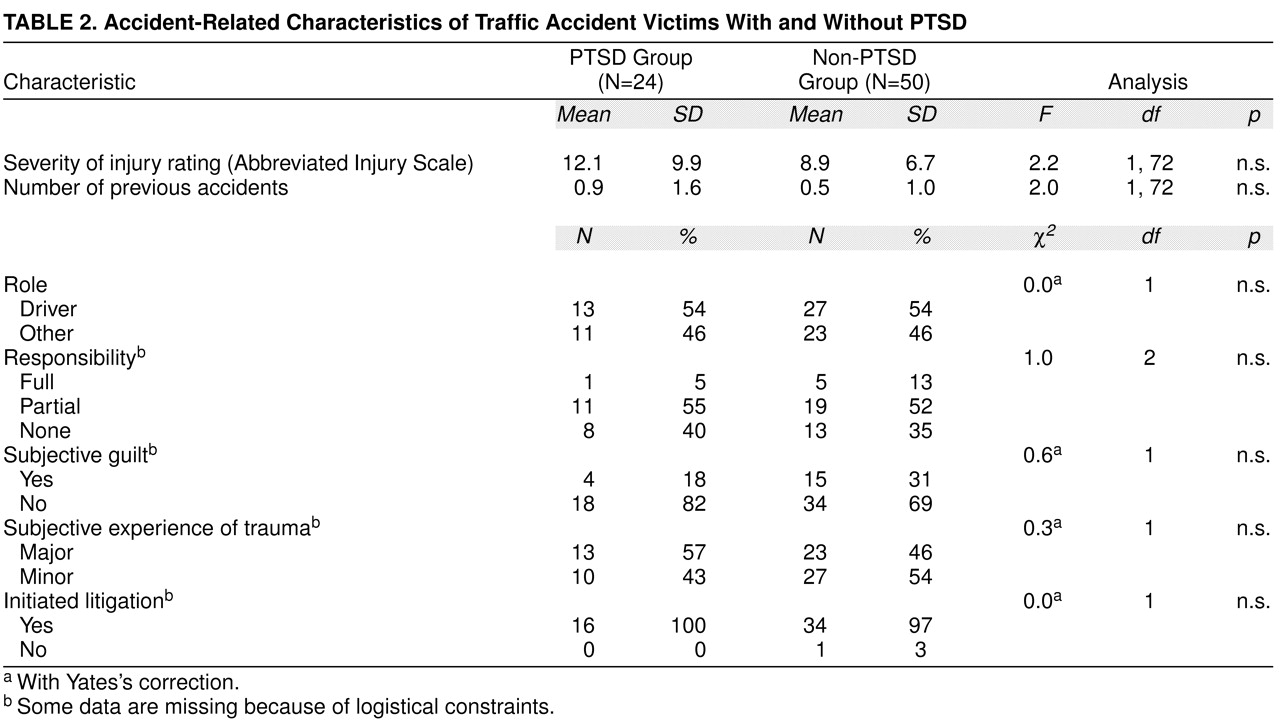
table 1). The only significant difference was in the percentage of Israeli-born subjects, which was lower in the comparison group than in both traffic accident groups. Similarly, PTSD diagnosis among traffic accident victims was not significantly associated with any of the accident-related characteristics assessed in this study, including severity of injury, objective responsibility as judged by the police, subjective sense of guilt, and initiation of litigation (
table 2).
The PTSD and non-PTSD groups exhibited different rates of psychiatric comorbidity. Sixteen (67%) of the 24 traffic accident victims who met diagnostic criteria for PTSD qualified also for other concurrent psychiatric diagnoses (11 for affective disorder and five for anxiety disorder), whereas only nine (18%) of the 50 non-PTSD traffic accident victims received another psychiatric diagnosis (six for affective disorder and three for anxiety disorder). This difference was statistically significant (Yates’s corrected χ2=15.1, df=1, p<0.001; odds ratio=9.1; 95% confidence interval=3.0–27.8). Diagnosis of PTSD at 1 year showed a trend toward a significant relationship with premorbid psychiatric history (Yates’s corrected χ2=2.7, df=1, p<0.10; odds ratio=3.1, 95% confidence interval=1.0–9.9). It was found, retrospectively, that eight (33%) of the traffic accident victims with PTSD had histories of premorbid psychiatric disorders (seven had affective disorder and one, anxiety disorder). Seven of these eight patients had a comorbid diagnosis at 1 year. Seven (14%) of the non-PTSD traffic accident victims were found to have a history of premorbid psychiatric disorders (four had affective disorder and three, anxiety disorder). Only one of these seven individuals received a psychiatric diagnosis at 1 year.
All 25 traffic accident victims and two comparison subjects who dropped out of the study did so after the initial evaluation during hospitalization. Dropping out was not significantly related to any of the sociodemographic measures, except for ethnicity; dropout traffic accident victims were significantly more likely to be Sephardic (60%) or Arab (28%) (χ2=22.8, df=6, p<0.001). Similarly, dropping out was not related to any of the accident variables, except for responsibility for the accident as determined by the police; dropout traffic accident victims were more likely to be either fully or partially responsible for the accident (81%) (χ2=29.2, df=4, p<0.001).
Longitudinal Course of PTSD Development
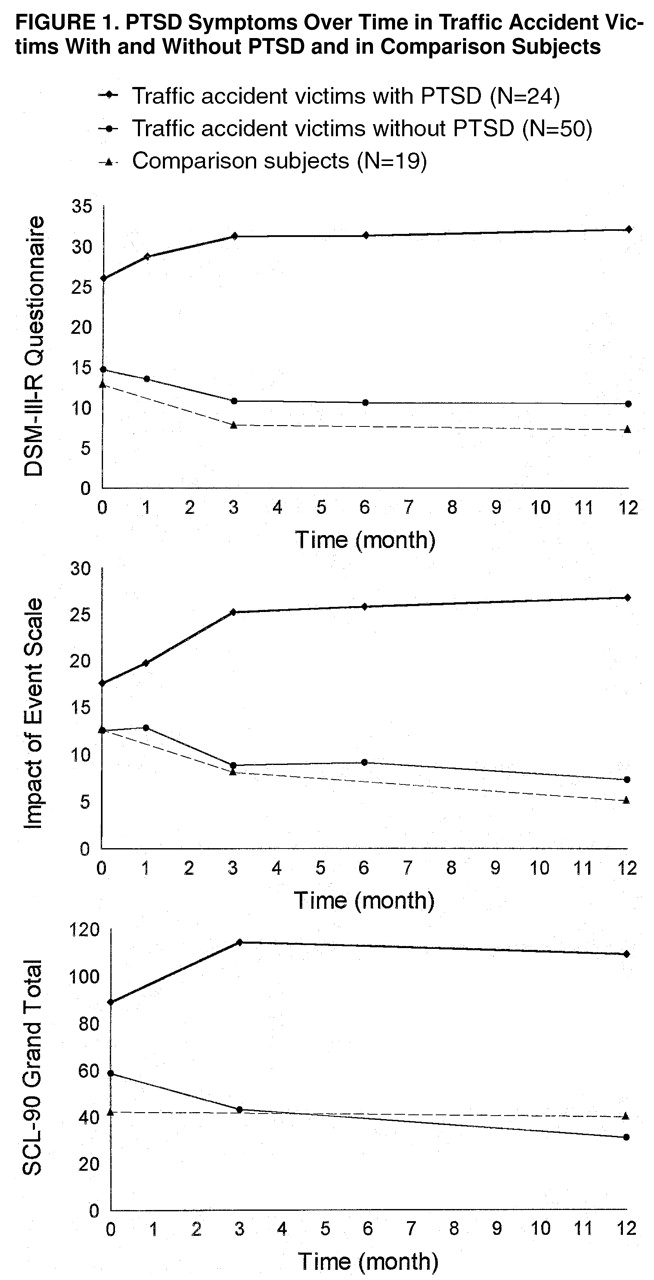
Figure 1 presents the development of posttraumatic as well as general psychiatric symptoms as measured by the DSM-III-R questionnaire, the Impact of Event Scale, and the SCL-90 in the three study groups over the multiple points of assessment. Visual inspection of
figure 1 reveals opposite trends in the PTSD and non-PTSD groups on all three measures. The nature of these opposite trends is such that an initial, relatively small difference between the scores of the PTSD and non-PTSD groups on these scales appears to increase progressively over the first 3 months following the accident. No apparent difference is evident between the non-PTSD and comparison groups.
Quantitatively, a MANOVA for repeated measures revealed a significant group-by-time interaction for the total scores of both the DSM-III-R Questionnaire (Wilks’s lambda F=4.40, df=4, 69, p<0.005) and the Impact of Event Scale (Wilks’s lambda F=12.03, df=4, 69, p<0.0001). The main time contribution to the overall interaction effect of PTSD on DSM-III-R came from the second time interval, that is, the period from 1 month to 3 months (F=4.75, df=1, 72, p<0.05). Similarly, the main source for the interaction effect on the Impact of Event Scale score was also the second time interval (F=15.22, df=1, 72, p<0.0002). The difference between the two groups at time of initial assessment, 1 week after the accident, was significant for the DSM-III-R total score (F=12.54, df=1, 72, p<0.0007; 95% confidence interval=5.0–17.7) but not for the Impact of Event Scale total score (F=2.49, df=1, 72; 95% confidence interval=–1.3–11.2). However, there was a significant effect of later PTSD on Impact of Event Scale total scores at the 1-month assessment (F=7.17, df=1, 72, p<0.009; 95% confidence interval=1.8–12.1). Replication of these analyses through use of the three DSM-III-R subscales (i.e., reexperiencing, avoidance, and hyperarousal) and the two Impact of Event Scale subscales (i.e., intrusion and avoidance) yielded a similar pattern of results, with no major differences between the subscales.
Last, a MANOVA for repeated measures revealed a significant group-by-time interaction for the total score on the SCL-90 questionnaire (Wilks’s lambda, F=5.40, df=2, 71, p<0.006). The contribution to the overall interaction effect came from both the first time interval (the period between the first week and 3 months) (F=9.97, df=1, 72, p<0.002) and the second time interval (the period from 3 to 12 months) (F=6.53, df=1, 72, p<0.05).
Relationship Between Acute Stress Reaction and PTSD at 1 Year
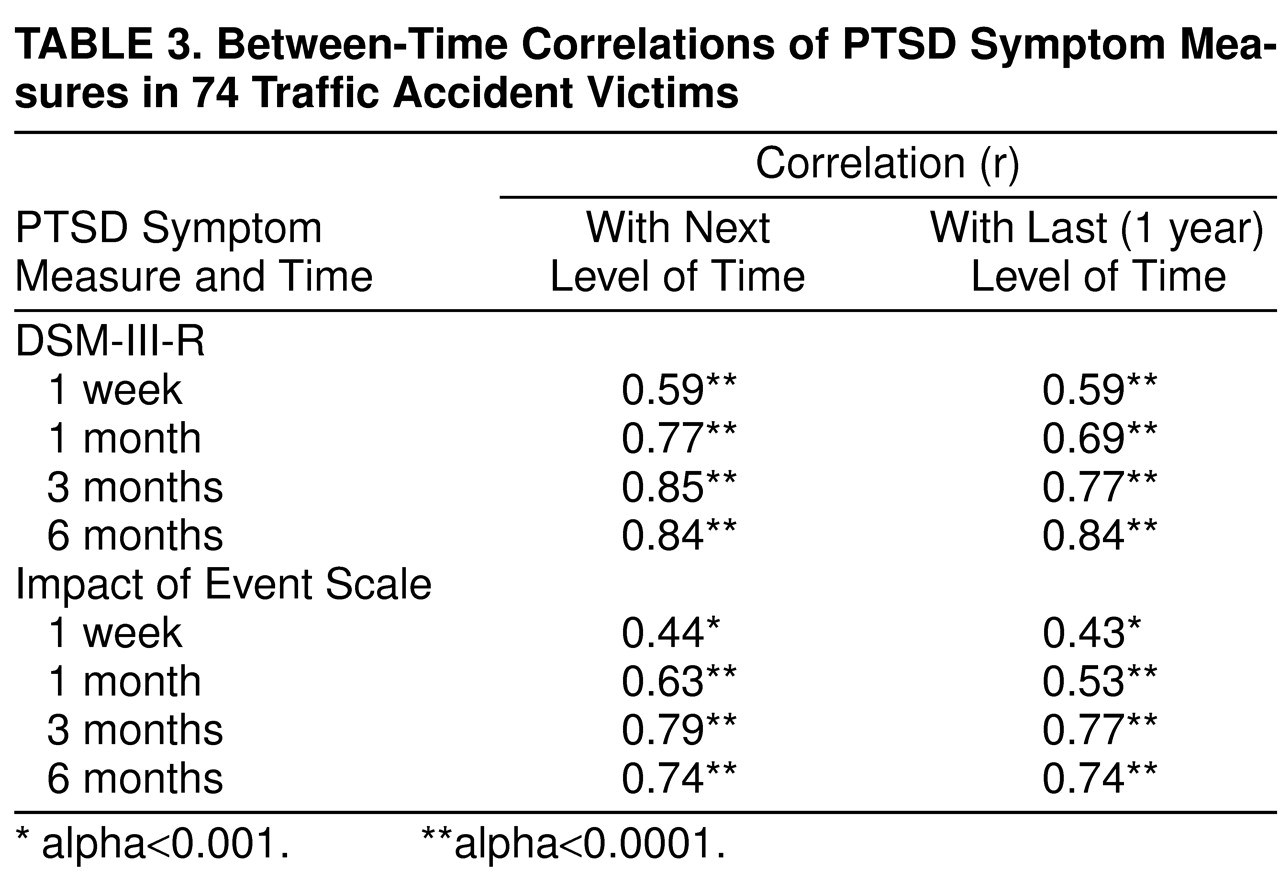
Next, in order to examine the stability of stress symptoms along the course of the first year after the accident, we correlated DSM-III-R and Impact of Event Scale scores at each point in time, with scores for the next and last points in time, within the entire group. As seen in
table 3, the between-time correlations increased progressively during the first 3 months after the accident and remained stable thereafter. Moreover, DSM-III-R and Impact of Event Scale scores at 3 months appear to be the best predictors of posttraumatic symptoms at 1 year.
In order to further examine the relationship between the different points in time and PTSD at 1 year, we performed a set of logistic regression analyses in which DSM-III-R and Impact of Event Scale scores from 1 week to 6 months were included as predictors of the presence or absence of PTSD at 1 year. The overall models, for both DSM-III-R and Impact of Event Scale scores, were highly significant (χ2=27.59, df=4, p<0.0001, and χ2=20.73, df=4, p<0.0005, respectively). When we tested each predictor, after adjusting for its scores at the other points in time, only month 6 DSM-III-R score was significant (χ2=4.26, df=1, p<0.05). Month 3 DSM-III-R and Impact of Event Scale scores showed a trend toward significance (χ2=2.74, df=1, p<0.09, and χ2=3.11, df=1, p<0.07, respectively). When DSM-III-R scores from all points in time were entered into a stepwise logistic regression, only month 3 and month 12 were selected for the model (χ2=5.17, df=1, p<0.02, and χ2=4.36, df=1, p<0.04, respectively). For Impact of Event Scale scores, only month 12 was included in the model (χ2=12.56, df=1, p<0.0004).
Last, we tested the diagnostic efficacy of the DSM-III-R questionnaire when treated as a dichotomous variable. Subjects were determined to have or not to have PTSD if the pattern of their answers to the DSM-III-R questionnaire did or did not meet the DSM-III-R criteria for PTSD. At 1 week, the DSM-III-R questionnaire correctly classified 70.3% of all subjects, including 70.8% of the PTSD patients (sensitivity) and 71.4% of the non-PTSD patients (specificity) (χ2=11.78, df=1, p<0.001). At 1 month, the overall accuracy was 70.6%, with 95.0% sensitivity and 60.4% specificity (χ2=17.59, df=1, p<0.001). At 3 months, the overall accuracy was 74.6%, with 89.5% sensitivity and 68.8% specificity (χ2=18.49, df=1, p<0.001).
DISCUSSION
In this study of 74 mildly to moderately injured traffic accident victims, 24 (32%) satisfied diagnostic criteria for PTSD 1 year after the accident. This figure is consistent with findings from previous prospective studies on other traumatized populations
(8,
27), as well as with studies of traffic accident victims
(5,
16,
17). Furthermore, the presence of additional axis I morbidity, primarily affective and anxiety disorders, in the PTSD (71%) and non-PTSD (14%) groups supports previous findings
(15,
16) that suggest that psychiatric sequelae of traffic accidents are not limited to posttraumatic symptoms. In light of reports on high rates of comorbidity in PTSD patients
(22,
28,
29), and spontaneous remission of PTSD symptoms in a significant portion of patients
(6) these results highlight the need to further investigate, over longer periods of time, the relationship between PTSD and other psychiatric morbidity in traumatized subjects.
The only premorbid factor that, in the current study, was related to PTSD at 1 year was previous psychiatric morbidity, especially affective and anxiety disorders. These findings are in accordance with data from previous studies
(5,
7) that found prior major depression to be an important risk factor for PTSD in traffic accident victims. Given that current views of anxiety and affective disorders link their onset to increased sensitivity to stressful life events, the development of PTSD in these subjects might reflect a diathesis to abnormal reactions to stress in general. In addition, this might account for the significantly different rates of comorbid disorders in the PTSD and non-PTSD groups.
The current data do not support a link between PTSD and major characteristics of the traumatic stressor itself. In contrast to previous studies
(5,
7), but as in the study by Shalev et al.
(8), trauma- and injury-related characteristics assessed in the present study, such as accident and injury severity and subjective perception of a threat to life, were not found to be associated with PTSD at 1 year. Considering the important implications of these results for the diagnosis of PTSD (the “criterion A” issue) and the equivocal findings in the literature, further investigation of the relationship between stressor characteristics and PTSD is warranted.
A major goal of this study was to examine prospectively the developmental course of PTSD formation in traffic accident victims throughout the first year after the accident. Our findings indicate a clear divergence of symptom profiles between traffic accident victims who did and did not meet diagnostic criteria for PTSD at 1 year. Three key features characterize these diverging trends. First, even though most subjects manifest acute stress symptoms immediately after the accident, their severity is significantly higher in the PTSD group. Second, this initial difference appears to intensify over the first 3 months, in that PTSD subjects show a marked and progressive worsening of symptoms, whereas non-PTSD subjects manifest gradual amelioration of symptoms to a level very similar to that of the comparison group. And last, during the period from 3 months to 1 year after the accident, distinct symptom levels in both groups seem to stabilize. The similarity between the symptom profiles of the non-PTSD and comparison groups suggests that hospitalization, in and of itself, was not responsible for PTSD.
Additional support for the importance of 3 months as a critical period for symptom crystallization was obtained from the peak of between-time correlations at this point in time. If true, these findings suggest that 3 months, rather than 1 month as reflected in the DSM-IV criterion for PTSD, might be a more appropriate cutoff for the transition from acute stress disorder to PTSD. In addition, the initial significant difference between the two groups supports the hypothesis that PTSD is an abnormal response to traumatic events in predisposed individuals
(8). On the other hand, considering the gradual amelioration of symptoms in the non-PTSD group, the alternative hypothesis viewing PTSD as a failure to extinguish an initially normal response to a traumatic event
(8) cannot be dismissed.
Our final goal in this study was to explore the diagnostic efficiency of early predictors for PTSD at 1 year. Using both the continuous and dichotomous approaches, we obtained relatively high sensitivity and specificity figures for the DSM-III-R questionnaire and, to a lesser degree, for the Impact of Event Scale. While firm conclusions regarding absolute levels of diagnostic accuracy cannot be drawn without cross-validation in an independent sample, these results clearly indicate that it is possible, as early as 1 week after the traumatic event, to detect subjects who will later develop PTSD.
The fact that formal diagnosis of PTSD was assessed only at 1 year limits our ability to address the issue of acute- versus delayed-onset PTSD in our group, namely, to identify subjects who were initially diagnosable but who later recovered or others who were initially free of symptoms but who were diagnosable at 1 year. However, the diagnostic efficiency results, as well as the high between-time correlations, suggest that the vast majority of PTSD subjects in our group (about 90%) had an acute rather than a delayed onset.
Another limitation of our findings relates to the fact that litigation status was only partially controlled for. This might be a potential confound. However, we believe that this could not account for the current results for several reasons. First, in Israel, all victims of traffic accidents, regardless of their legal responsibility, are entitled to free medical care and disability compensation. Thus, in actuality, all traffic accident victims, independent of their long-term morbidity, file litigation. This was true for our subjects as well (
table 2). Second, our results show significant intergroup differences on some of the measures as early as 1 week after the accident, when none of the subjects was in a medical condition to obtain legal advice. Finally, while traditional views, dating back to Miller’s concept of “accident neurosis”
(30), suggest a perpetuating role for litigation in the formation of PTSD, more recent studies
(16,
31,
32) question this relationship, showing that litigation settlement does not result in improvement of posttraumatic stress symptoms in those who develop them.
In summary, the results of this study provide further support for the fact that injured victims of traumatic events, traffic accidents in our case, are at considerable risk for development of PTSD even when they are only mildly injured. Furthermore, those who develop PTSD can be identified shortly after the traumatic event, even though the optimal point for making a diagnosis of PTSD appears to be 3 months. Finally, given the high percentage of subjects who develop PTSD and the apparent feasibility of early diagnosis, the preventive efficacy of early pharmacological and psychotherapeutic intervention needs to be studied. This is particularly important given the chronic course that PTSD tends to follow.