Postsynaptic serotonin 5-HT
2A receptors play an important role in mediating the effects of serotonin on local cortical circuitry and are targets for certain antidepressant medications
(1) . The 5-HT
2A receptor is found predominantly in cortical areas and is located on both glutamatergic pyramidal neurons and γ-aminobutyric acid (GABA) interneurons
(2,
3) . The binding density of 5-HT
2A receptors has been investigated extensively in postmortem studies, and evidence suggests an increase in 5-HT
2A receptor numbers in the prefrontal cortex in suicide victims
(4,
5), although there are some notable inconsistencies
(6,
7) . Similarly, there has been some limited evidence for an increase in cortical 5-HT
2A receptor binding in dying patients with depression
(8,
9) .
The difficulties involved in postmortem ligand binding work
(10) have stimulated studies of 5-HT
2A receptors in living human brain through positron emission tomography (PET) and single photon emission tomography (SPET). In contrast to the postmortem work, most imaging studies in depressed patients have found either no change or a decrease in 5-HT
2A receptor binding in the cerebral cortex (reviewed by Stockmeier
[11] ). However, methodological problems related to the available radioligands
(12,
13) as well as to the use of psychotropic medications prior to scanning
(11) limit the conclusions that can be drawn from these studies. In support of this notion, a previous study of acutely depressed patients who were drug free for more than 3 months found increased 5-HT
2A receptor binding in the frontal cortex of subjects with high scores on the Dysfunctional Attitudes Scale
(14) .
The development of [
11 C]MDL 100,907 as a PET radioligand offers potential advantages in terms of receptor selectivity because [
11 C]MDL 100,907 binds with a high and selective affinity to 5-HT
2A receptors and, when used in conjunction with PET, produces high-quality images that correspond well with known 5-HT
2A binding distribution derived from postmortem studies
(15 –
18) . Furthermore, [
11 C]MDL 100,907 does not give rise to radiolabeled metabolites that are likely to cross the blood-brain barrier, and radioligand binding can be reliably quantified
(16,
19,
20) .
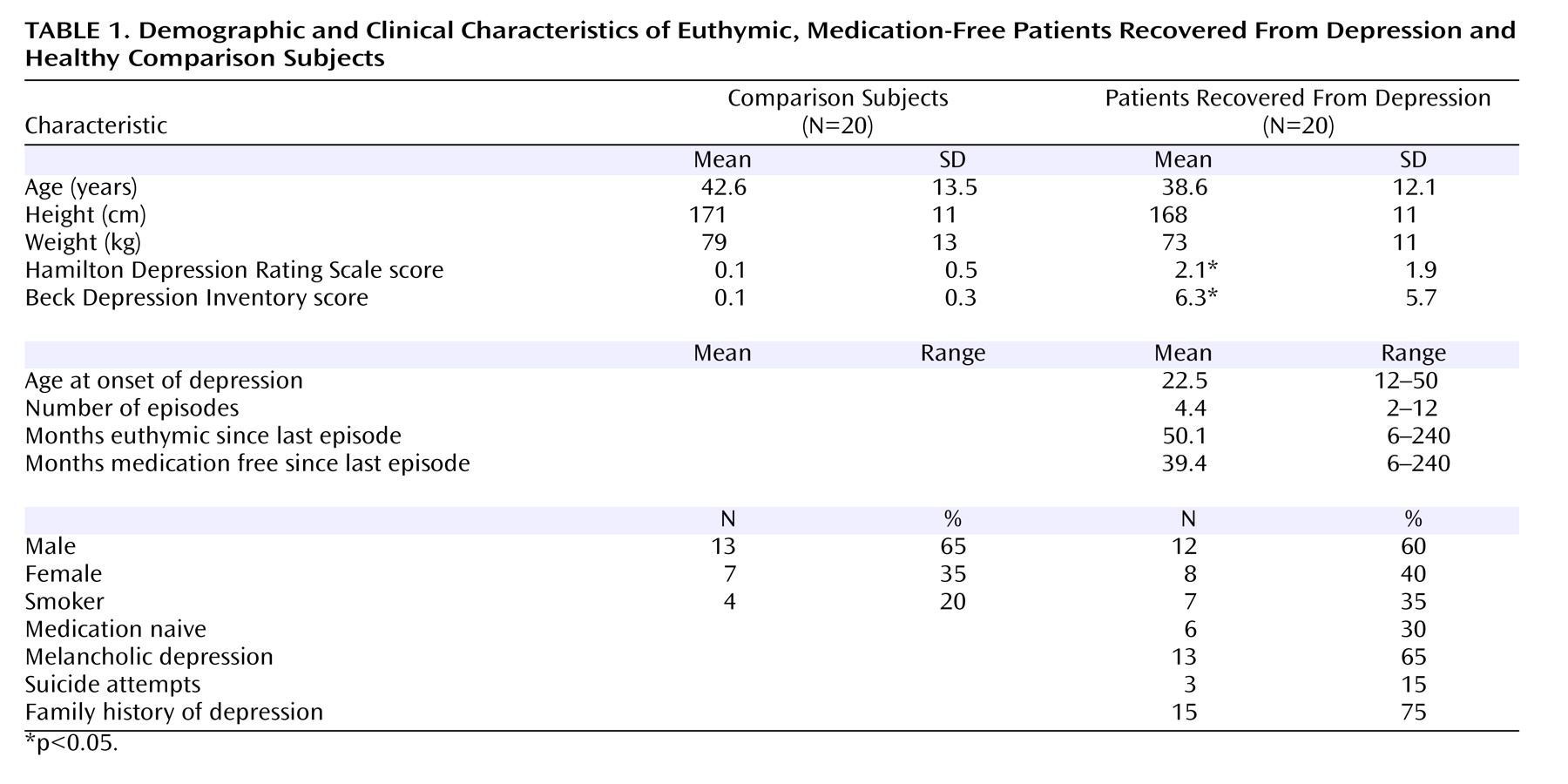
Results
Preliminary analysis showed no main or interactive effect of gender on 5-HT 2A binding potential; gender was therefore omitted from subsequent analyses. There was no statistically significant difference in cerebellar V D between healthy subjects (19.4 ml plasma/ml tissue [SD=1.4]) and patients (19.2 ml plasma/ml tissue [SD=2.8]) (F=0.07, df=1, 37, p<0.79). There was no effect of age on cerebellar V D values (F=1.48, df=1, 37, p=0.23).
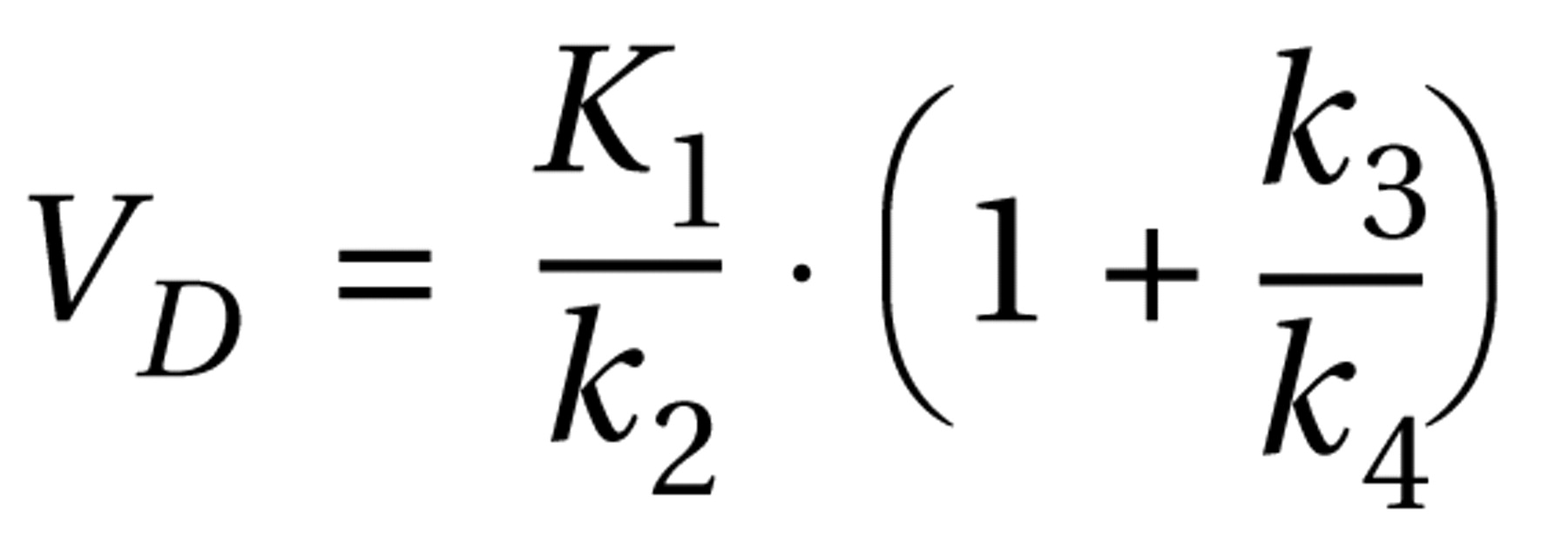
Three outcome measures of PET neuroreceptor quantification are commonly considered, all of which are proportional to the availability of receptors
(32,
33) . In this study, we report our results as f
2 ·BP (i.e., the product of the free fraction in tissue and binding potential) because this outcome parameter has been shown in several neuroreceptor PET studies
(33) to be the most reproducible and least susceptible to experimental error. However, the use of this parameter is based on the assumption of uniformity of the nondisplaceable compartment across subjects and groups. In our study, there was no significant difference in the V
D of the reference region. Therefore, f
2 would appear to be homogeneous across our study group, and results are reported as f
2 ·BP.
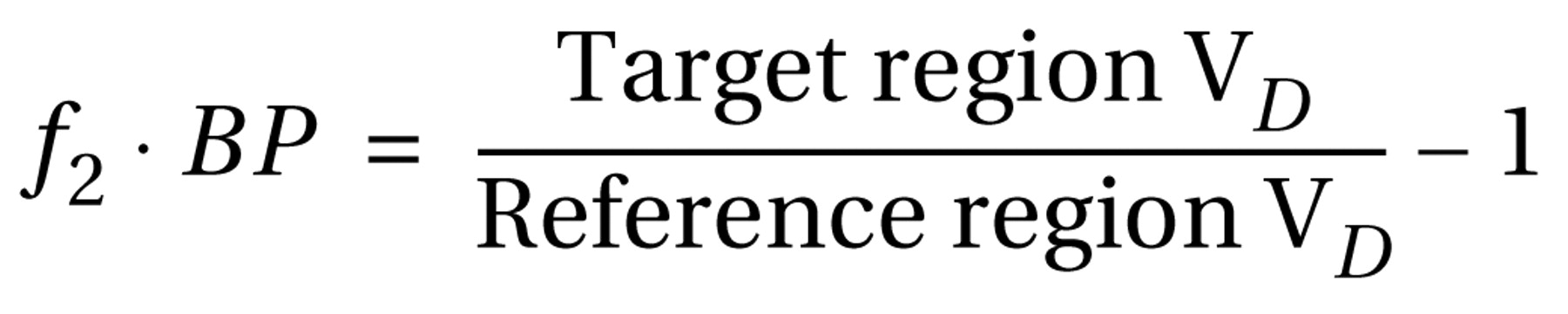
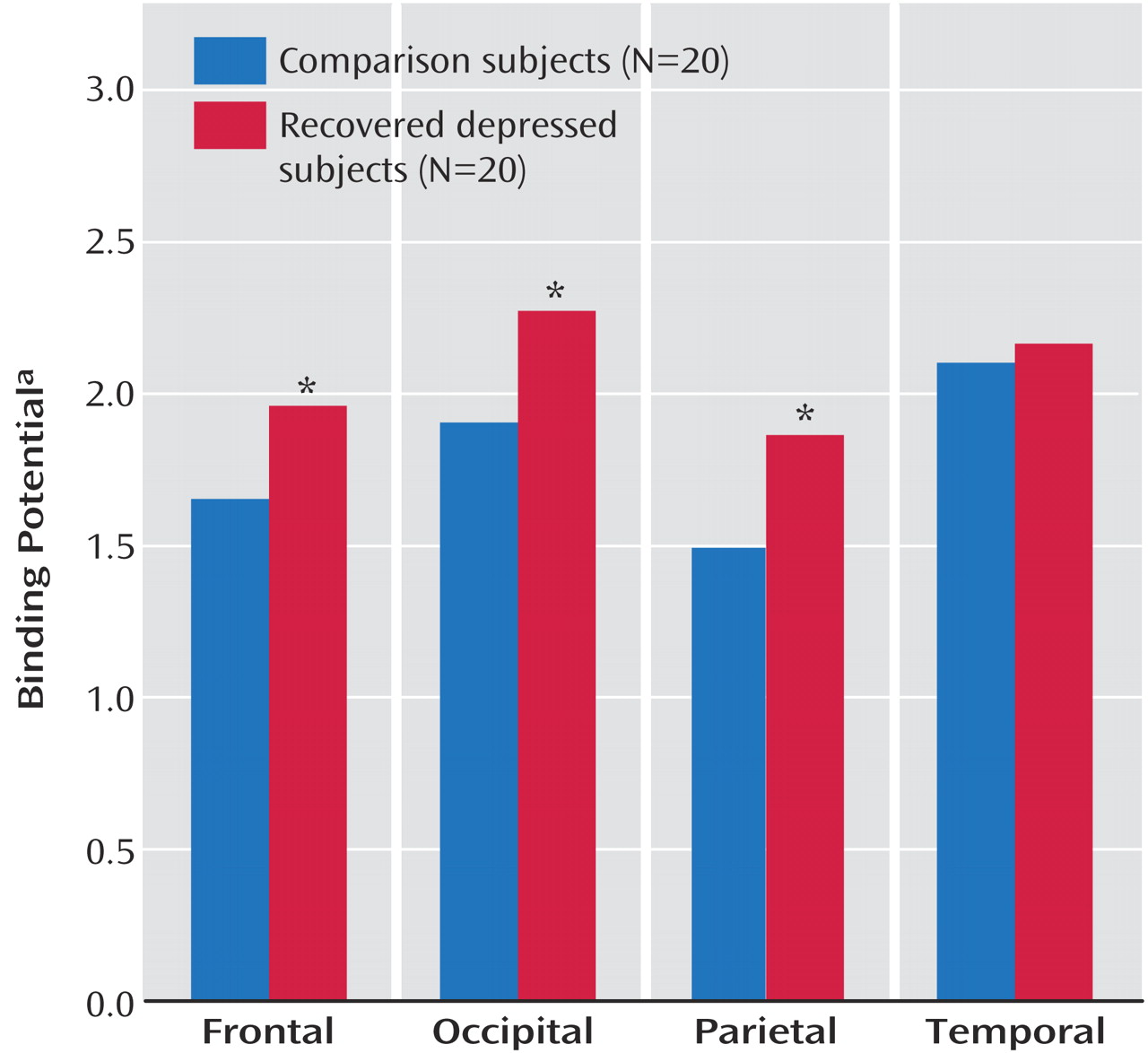
An ANCOVA of regional cortical 5-HT
2A binding potential values with age as a covariate showed significant main effects of region (F=9.40, df=3, 102, p<0.001) and age (F=9.1, df=1, 34, p=0.005) but not diagnosis (F=1.63, df=1, 34, p=0.21). There was, however, a significant diagnosis-by-region interaction (F=4.69, df=3, 102, p<0.02). Post hoc analysis showed that patients had significantly increased 5-HT
2A binding potential in the frontal cortex, occipital cortex, and parietal cortex but not in the temporal cortex (
Figure 1 and
Figure 2 ). Due to the effect of age on 5-HT
2A binding, we further examined a subset of 16 patients and 16 comparison subjects who were individually matched for age to within 1 year (healthy subjects: mean=39.6 years [SD=13.3], patients: mean=39.6 years [SD=13.2]; p=0.99). An ANCOVA (with age as a covariate) also revealed a significant region-by-diagnosis interaction (F=4.26, df=3, 78, p<0.02) and a significant main effect of age (F=9.51, df=1, 26, p=0.005).
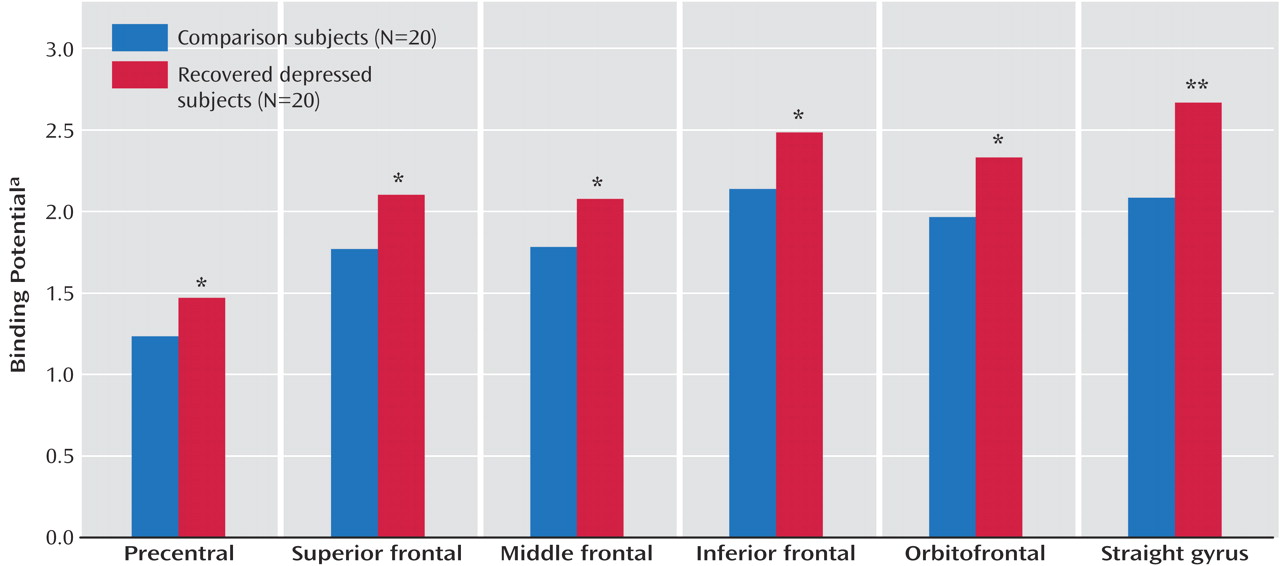
Most of the postmortem work on 5-HT
2A receptor binding in suicide victims has focused on various subregions of the frontal cortex. To explore the increase in 5-HT
2A binding potential in the frontal cortex in more detail, we performed a further analysis of frontal cortical regions examining the superior, middle, and inferior frontal gyri, the orbitofrontal cortex, the straight gyrus, and the precentral gyrus. An ANCOVA of these regions with age as a covariate showed a main effect of diagnosis (F=4.75, df=1, 36, p<0.04) and age (F=6.43, df=1, 36, p<0.02) but no significant interactions between diagnosis and region (F=2.01, df=5, 180, p<0.13). Post hoc analysis of 5-HT
2A binding potential showed that patients had statistically significant increases in binding potential values in all six frontal regions (
Figure 3 ).
In the combined population of patients and comparison subjects, age correlated negatively with 5-HT 2A binding potential in all four cortical regions studied (frontal: r=–0.39, p<0.02; temporal: r=–0.59, p<0.001; parietal: r=–0.36, p<0.03; occipital: r=–0.43, p=0.006). Global 5-HT 2A binding potential in the frontal cortex did not correlate significantly with any of the measured clinical characteristics in the patient group such as age at illness onset, lifetime duration of illness, number of episodes, duration of euthymia, or duration medication free. Notwithstanding the small numbers, there were no statistically significant differences within the patient group in 5-HT 2A receptor binding potential between patients with versus without melancholia, with versus without a family history of depression, or with versus without a history of self-harm.
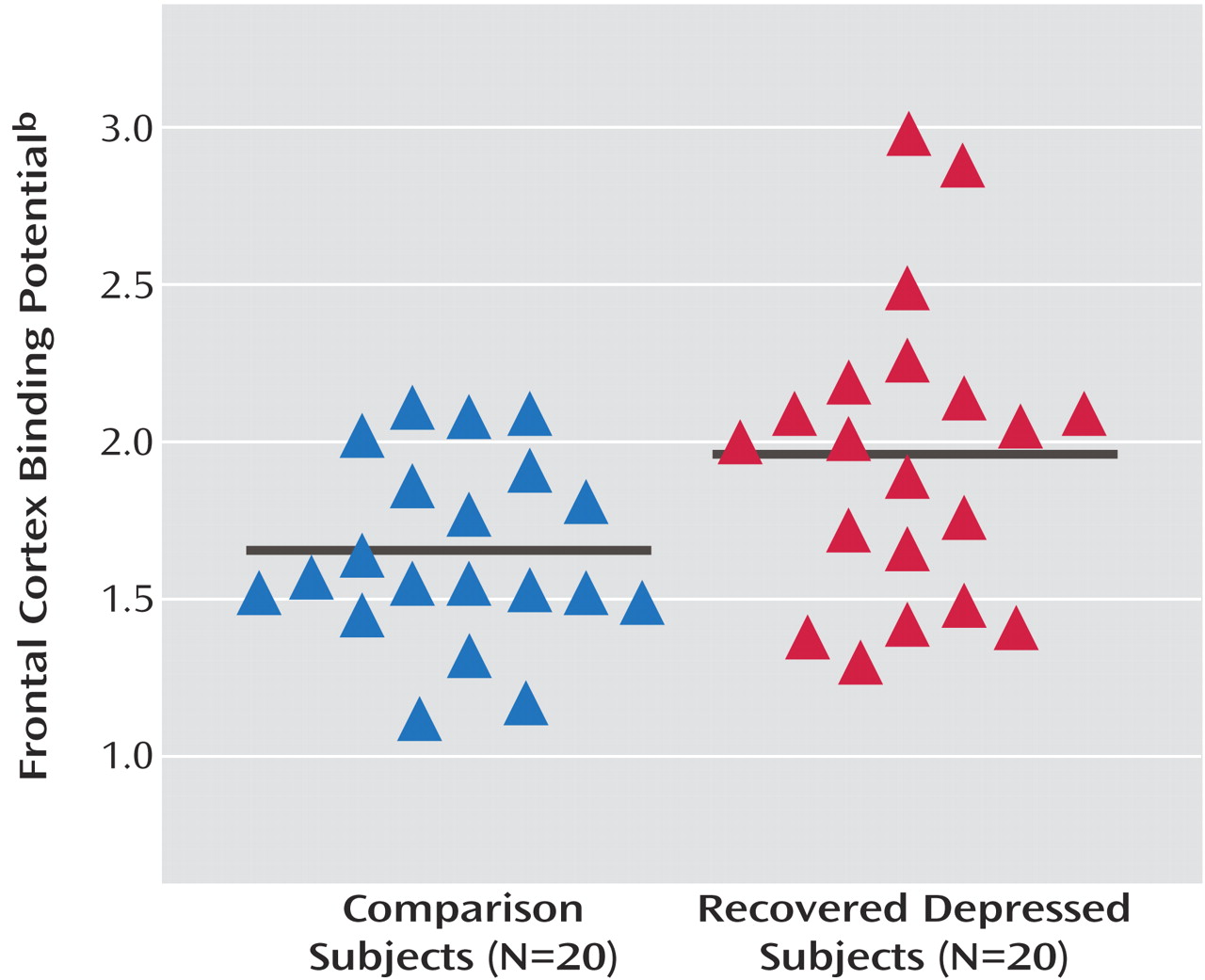
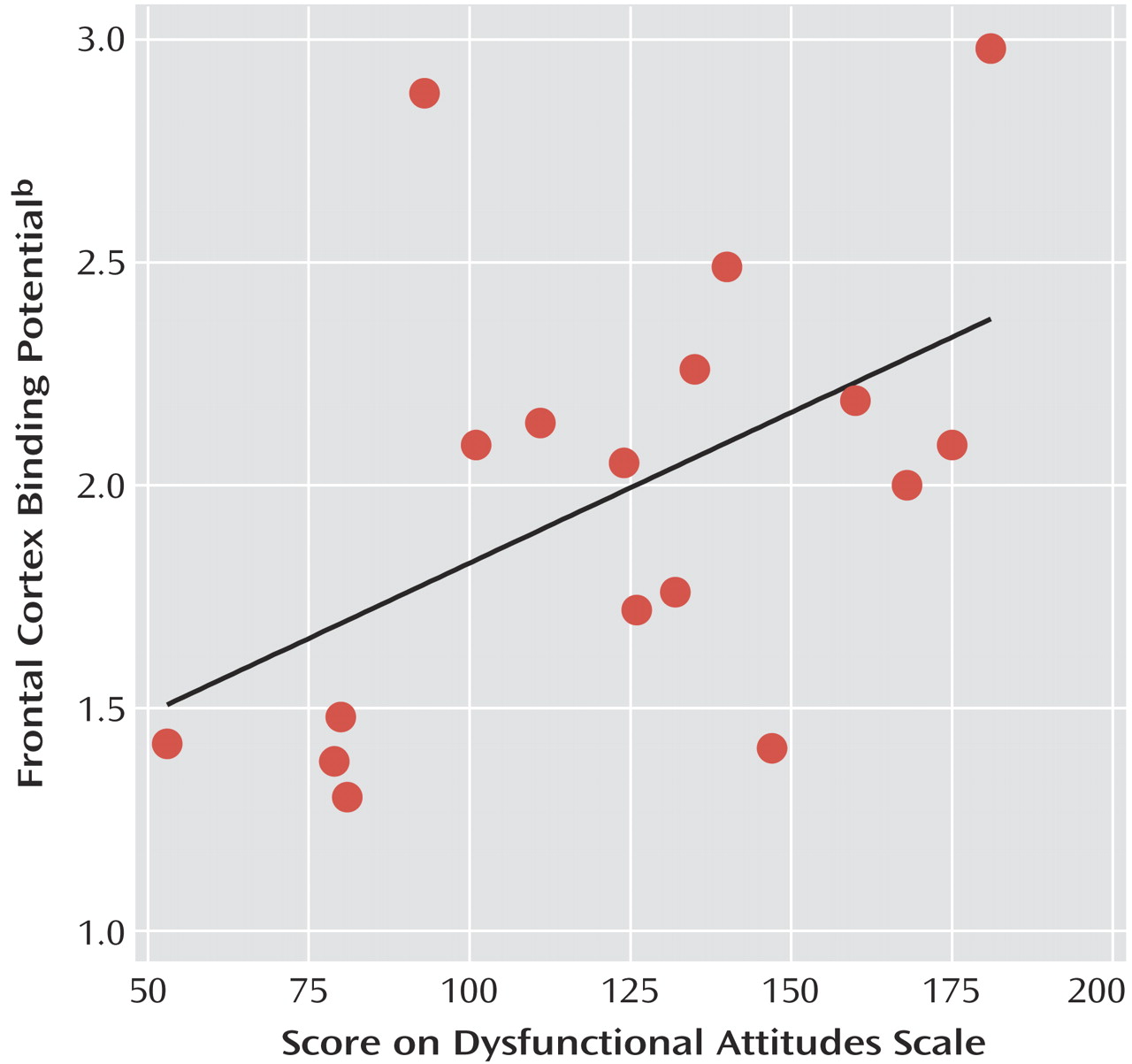
Three of the patients did not complete the Dysfunctional Attitudes Scale and were not included in the analysis. In the 17 remaining subjects, Dysfunctional Attitudes Scale scores were significantly higher (p=0.02) in patients (mean=123 [SD=38]) relative to comparison subjects (mean=97 [SD=19]). In keeping with previous findings
(14), an ANCOVA with age and Dysfunctional Attitudes Scale scores as covariates showed significant main effects of Dysfunctional Attitudes Scale score (F=6.24, df=1, 27, p<0.02) and age (F=6.22, df=1, 27, p<0.02) on frontal 5-HT
2A binding potential. Dysfunctional Attitudes Scale scores also correlated significantly with frontal 5-HT
2A binding potential in the patients (
Figure 4 ) but not in healthy subjects (r=–0.31, df=18, p=0.28). There was no significant correlation between age and frontal binding potential in the patients considered alone (r=–0.37, df=15, p=0.11). However, the correlation of Dysfunctional Attitudes Scale scores and frontal 5-HT
2A binding potential in the patients remained significant after partial correlation that controlled for the effect of age (
Figure 4 ).
Discussion
Our findings indicate that recovered depressed patients have higher [
11 C]MDL 100,907 binding potential in several cortical regions compared with healthy subjects. This is consistent with a greater availability of 5-HT
2A receptors. As reported by others, 5-HT
2A receptor binding showed an inverse correlation with age
(30,
34) . The mean age of our patient group was slightly but nonsignificantly lower than the comparison group, but recovered depressed subjects had significantly higher 5-HT
2A binding potential even after we adjusted for age with a covariance analysis. In addition, individually matching subjects for age also revealed a significant increase in [
11 C]MDL 100,907 binding. Finally, Dysfunctional Attitudes Scale scores were significantly higher in the recovered patients relative to healthy comparison subjects and as reported by Meyer and colleagues
(14) . 5-HT
2A binding potential was significantly and positively correlated with Dysfunctional Attitudes Scale scores in the depressed subjects but not in the comparison subjects. While the effect size (1.06) of the difference in binding potential between comparison and recovered subjects would not be considered trivial
(35), our findings should be considered preliminary until replicated.
In PET neuroreceptor imaging, differences in binding potential do not distinguish between changes in the concentration of binding sites or changes in apparent receptor affinity or the concentration of competing endogenous ligands. There is currently no evidence from postmortem data to suggest that depression is associated with a change in the affinity of 5-HT for the 5-HT
2A receptor. Theoretically, increased 5-HT
2A receptor availability might also be caused by decreased concentrations of synaptic 5-HT
(1) . However, neither human nor animal studies suggest that [
11 C]MDL 100,907 binding is modified by acute increases or decreases in the availability of endogenous 5-HT
(36,
37) . Therefore, the increase in 5-HT
2A receptor binding potential observed in the subjects recovered from depression is likely to represent an increase in the density of 5-HT
2A receptor binding sites.
As noted here, the status of cortical 5-HT
2A receptors has been investigated extensively in depressed patients with varying results. Data from postmortem studies of suicide victims suggest increased 5-HT
2A receptor density in the frontal cortex
(4,
5), but in vivo imaging studies in acutely depressed subjects have found mostly either a reduction or no change in 5-HT
2A receptor availability
(11) . The reason for this apparent discrepancy may relate to particular clinical characteristics associated with suicidal behavior, such as diagnostic comorbidity, substance use, agitation, and insomnia as well as the methodological difficulties involved in carrying out postmortem studies
(10) . In vivo imaging studies allow investigation of prospectively well-characterized subjects, but interpretation of results can be complicated by factors such as previous antidepressant treatment and issues relating to ligand specificity and modeling
(11) .
Our finding of a significant positive correlation between 5-HT
2A binding potential and Dysfunctional Attitudes Scale scores in recovered depressed subjects is in keeping with previous studies in which relative to healthy subjects depressed subjects with higher Dysfunctional Attitudes Scale scores had increased 5-HT
2A receptor binding (as measured by [
18 F]setoperone)
(14) and 5-HTT binding (measured with [
11 C]DASB)
(22) . While Dysfunctional Attitudes Scale scores tend to normalize with clinical improvement, recovered depressed subjects can still demonstrate higher levels of dysfunctional attitudes than never depressed healthy subjects
(38,
39) . Moreover, there are strong correlations between Dysfunctional Attitudes Scale scores of depressed individuals before and after treatment
(39,
40) . This raises the possibility that patients with high Dysfunctional Attitudes Scale scores during recovery would also be the individuals with higher Dysfunctional Attitudes Scale scores when depressed. Taken together, the data suggest that increased cortical 5-HT
2A receptor binding identifies a group of depressed patients with higher levels of dysfunctional attitudes both during depression and after clinical recovery.
If 5-HT
2A receptor binding is increased in depressed subjects with high Dysfunctional Attitudes Scale scores, what might be the mechanism? There is much evidence that major depression is associated with decreased brain 5-HT neurotransmission
(1), and Meyer et al.
(14) suggested that increased 5-HT
2A receptor binding might reflect an up-regulation of cortical 5-HT
2A receptors in response to chronically impaired 5-HT release, particularly in subjects with high Dysfunctional Attitudes Scale scores. Our findings suggest the possibility that this might continue to be the case after clinical recovery and withdrawal of antidepressant treatment. Consistent with this, evidence from 5-HT neuroendocrine challenge tests suggests impaired presynaptic 5-HT function may persist into clinical recovery
(41) . It must be noted, however, that 5-HT
2A receptors do not always appear to be regulated classically in terms of neurotransmitter availability, and changes in local receptor trafficking involving protein kinases and arrestins might play a part in the increased 5-HT
2A receptor availability seen in the present study
(42) .
Recent animal experimental studies have demonstrated strong reciprocal connections between cortical glutamatergic output neurons and ascending 5-HT pathways from the raphe nuclei
(43) . 5-HT
2A receptors are located on glutamatergic cell bodies, postsynaptic to the 5-HT neurons that terminate in frontal cortex
(3) . These receptors are therefore ideally placed to regulate the activity of cortical-raphe pathways, one of the functions of which is to provide the raphe with information coding for the controllability of stress
(44) . The latter formulation is particularly intriguing, given the correlation between increased cortical 5-HT
2A receptor binding and the Dysfunctional Attitudes Scale. Taken together, these preclinical and clinical data suggest that 5-HT
2A receptors, through their effect on the excitability of glutamatergic neurons, form part of a neurobiological substrate underpinning the dysfunctional beliefs that put individuals at risk of depressive episodes.