Research has consistently shown associations between posttraumatic stress disorder (PTSD) and poorer neurocognitive functioning as measured by neuropsychological tests, in particular functions related to attention and memory
(1 –
7) . Such findings have been reported for specific population groups—for example, college students
(8) and individuals who have experienced PTSD after childhood sexual abuse
(5), rape
(6), combat
(4,
7,
9), or the Holocaust
(10) . It has been suggested that such deficits are a consequence of abnormalities in the norepinephrine system
(11) or of decreased hippocampal volume, which is also consistently found to be associated with PTSD
(12,
13) . Although reservations have been expressed about the generalizability of the relationship between PTSD and neurocognitive dysfunction
(14), the principal question raised by this association is whether neurocognitive deficits exist prior to traumatic experiences and represent a vulnerability factor for PTSD or whether these deficits are a consequence of neurobiological changes brought about by severe stress. In support of the first position, Brewin and Smart
(15) have argued that individuals with greater working memory capacity may have a greater ability to suppress the unwanted intrusive thoughts associated with PTSD. While lower levels of pretrauma education or intellectual resources have been identified as vulnerability factors for PTSD
(16), it has also been suggested that extreme stress may result in a further decline in neurocognitive functioning
(3,
4) .
One of the difficulties in conducting research in this area is that traumatic experiences are unpredictable. In most studies of associations between PTSD and memory performance, researchers assess the neurocognitive skills of individuals who have already experienced traumatic events, comparing those who have PTSD with those who are mentally healthy
(4,
6,
7) . Without pretrauma neurocognitive measures, however, such studies can do no more than determine whether an association is observed between memory deficits and PTSD.
We present findings of a study examining the impact of a major traumatic event on memory and other cognitive abilities of a large community-based sample of young adults. Participants were first interviewed for a longitudinal study in Canberra, Australia, and then reinterviewed four years later after a major natural disaster in the region—a large bushfire in which several people were killed and nearly 500 homes were destroyed. A number of neurocognitive measures were obtained from participants both before and after the trauma. In the postdisaster interview, participants were also asked about their level of exposure to traumatic events as a result of the fire and the extent to which they were experiencing the PTSD symptoms of reexperiencing and arousal as a result of that exposure. These data allowed us to examine the association between experience of fire-related PTSD symptoms and poorer pretrauma neurocognitive functioning as well as decline in neurocognitive functioning after the trauma. We were also able to examine the differential effects of reexperiencing and arousal symptoms on neurocognitive functioning.
Method
Background
In January 2003, fires triggered by lightning strikes in drought-stricken areas of bushland surrounding Canberra resulted in a 10-kilometer fire front that reached residential areas of the city. As a result of the fire, four people were killed, 440 people presented to local hospitals with fire-related injuries, 488 houses were destroyed, and some 5,000 people were evacuated on short notice to emergency shelters
(17) .
Participants
The PATH Through Life project is following a random selection of three age groups of residents in Canberra and the neighboring town of Queanbeyan (combined population, approximately 340,000 in 2001). The aim of the project is to explore changes in cognitive abilities over the lifetime and to identify risk factors associated with depression, anxiety, and substance use. Potential participants were drawn at random from the electoral rolls (for which enrollment is compulsory for Australians age 18 and over). Participants in this study were 20 to 24 years of age on January 1, 1999. Of 4,105 potential participants, 2,404 (58%) agreed to participate in the project (wave 1). Four years later, at wave 2, 190 (7.9%) wave 1 participants refused to continue in the study, seven (0.3%) had died, and 68 (2.8%) could not be contacted. This left 2,139 participants (89% of the original cohort), who were reinterviewed. Those lost to follow-up were more likely to be male, had significantly fewer years of education, and had poorer scores on neurocognitive measures in wave 1. At both waves, potential participants were given a thorough description of the study and provided written informed consent before participating.
Of the 2,097 participants who responded to both questions about the bushfire and PTSD, this study focuses on the 1,599 who reported having experienced one or more traumatic events related to the fire. The participants’ mean age at the second interview was 26.7 years (SD=1.5); 52.0% of participants were female. The age and sex distribution of this subgroup was not significantly different from that of the overall group of wave 2 respondents. Time between the bushfire and the wave 2 interviews ranged from 12 to 82 weeks (mean=36.3 weeks, SD=11.3), and the mean time between the wave 1 interview and the fire was 3.4 years (SD=0.27).
Measures
When reinterviewed, participants were asked 10 questions concerning their exposure to the bushfire. Five questions concerned uncontrollable events, including fire-related injury or damage to or destruction of property, either their own or that of family members or friends. Two questions covered controllable actions: being personally involved in fighting fires in their home or neighborhood and undertaking other work, including firefighting elsewhere. Three questions were assessed as representing trauma threats: having been put on alert or evacuated and having had buildings in their suburb damaged or destroyed by fire.
Participants also completed the Trauma Screening Questionnaire
(18), which comprises five questions concerning reexperiencing of traumatic events through nightmares, flashbacks, and unwanted thoughts and five concerning symptoms of arousal—that is, symptoms for criteria B and D, respectively, of the DSM-IV diagnosis of PTSD. Questions were worded to assess whether participants had experienced symptoms at least twice in the week preceding their interview as a consequence of their exposure to the fires—for example, whether they had upsetting dreams about the bushfire or had difficulty concentrating when reminded of the bushfire. In a validation study of the Trauma Screening Questionnaire, positive responses to six or more of the 10 questions predicted a diagnosis of PTSD with a sensitivity of 0.86 and a specificity of 0.93
(18) .
Neurocognitive measures obtained from participants at both interviews included the digits backwards subtest of the Wechsler Memory Scale
(19,
20), the Symbol-Digit Modalities Test
(21), and immediate and delayed recall using the first trial of the California Verbal Learning Test
(22) . The Spot-the-Word Test—Version A
(23) was also administered and was included in the analyses. In this test, the participant is presented with 50 pairs of words and nonwords and is asked, for each pair, to identify the word. This measure of verbal intelligence correlates highly with the National Adult Reading Test
(24) and could be expected to remain relatively unaffected by neuropsychiatric disorder. These neurocognitive tests were selected for the PATH interviews because of their ability to identify cognitive change related to aging and because of their relative brevity.
A variety of other factors that could be expected to affect neurocognitive performance were also assessed at both interviews and controlled for in the analyses. These included variables such as level of education and count of current symptoms of depression using the scale developed by Goldberg and colleagues
(25) . Alcohol use disorders, which are commonly found to be associated with PTSD and are likely to affect neurocognitive functioning
(26,
27), were assessed with categorical estimates of weekly consumption of alcohol derived from the quantity and frequency items of the Alcohol Use Disorders Identification Test (AUDIT)
(28) . At both waves, participants were identified as drinking hazardous or harmful amounts of alcohol if they reported usual consumption levels exceeding 28 standard drinks per week for men or 14 standard drinks per week for women
(29) .
Data Analysis
For the first set of analyses, we categorized participants into three groups: those who screened positive for PTSD on the Trauma Screening Questionnaire (six or more PTSD symptoms), those with subthreshold levels of PTSD symptoms (score of 1 to 5), and those with no such symptoms. We included the subthreshold group because of evidence that having any PTSD symptoms can impair functioning
(30,
31) . For the second and third analyses, we classified participants by whether they reported one or more reexperiencing symptoms and then by whether they experienced one or more arousal symptoms. For each of the three analyses, we used repeated-measures analyses to identify the extent to which the neurocognitive skills of those who met or did not meet PTSD symptom classification differed before the trauma and changed as a result of the trauma. In all of these analyses, we controlled for seven factors by including them as covariates: age, gender, education at second interview, time elapsed between fire and interview, level of exposure to the fire, depressive symptoms, and hazardous or harmful levels of alcohol consumption. In the analyses of the delayed recall component of the California Verbal Learning Test, we also controlled for level of immediate recall because delayed recall is dependent on that initial level of recall. Testing in each analysis indicated that there were no significant differences in error variances across groups. All analyses were conducted with SPSS, version 12.0 (SPSS, Chicago).
Results
Of the 1,599 young adults in our study who were exposed to a potentially traumatic fire-related event, 38 (2.4%) screened positive for fire-related PTSD (that is, reported having experienced six or more PTSD symptoms in the past week) in the postdisaster interview, and 605 (37.8%) participants met subthreshold criteria (reported having experienced one to five PTSD symptoms). Among those who met screening criteria, the mean number of PTSD symptoms reported was 7.1 (SD=1.25), and among those in the subthreshold group, it was 1.87 (SD=1.09). A total of 434 participants (27.1%) reported having one or more reexperiencing symptoms at least twice in the week preceding the interview, and 472 (29.5%) reported one or more arousal symptoms.
Main Effects
PTSD Symptom Level
For the first set of analyses, we examined the extent to which level of PTSD symptoms was associated with having significantly different neurocognitive scores before and after the fire.
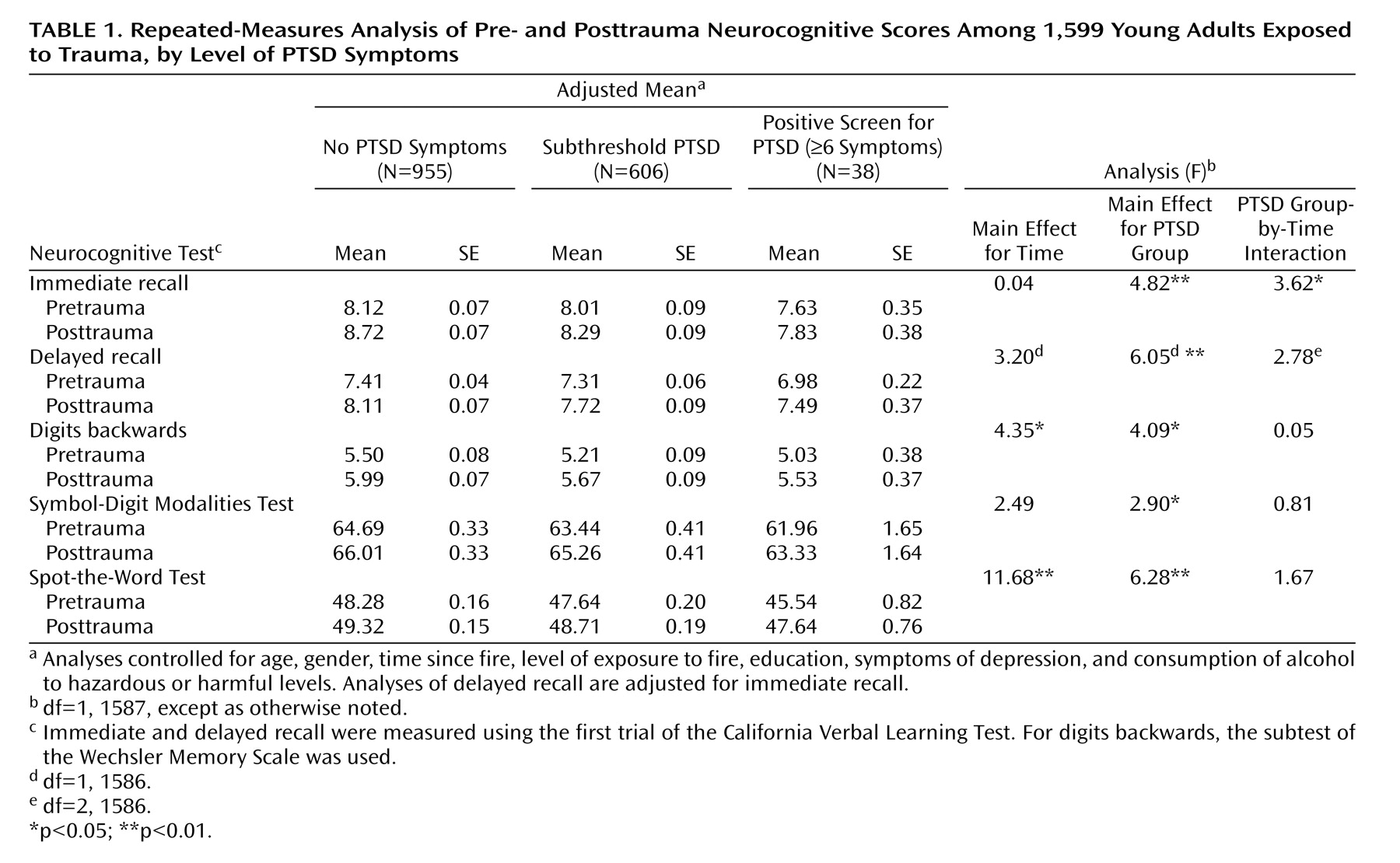
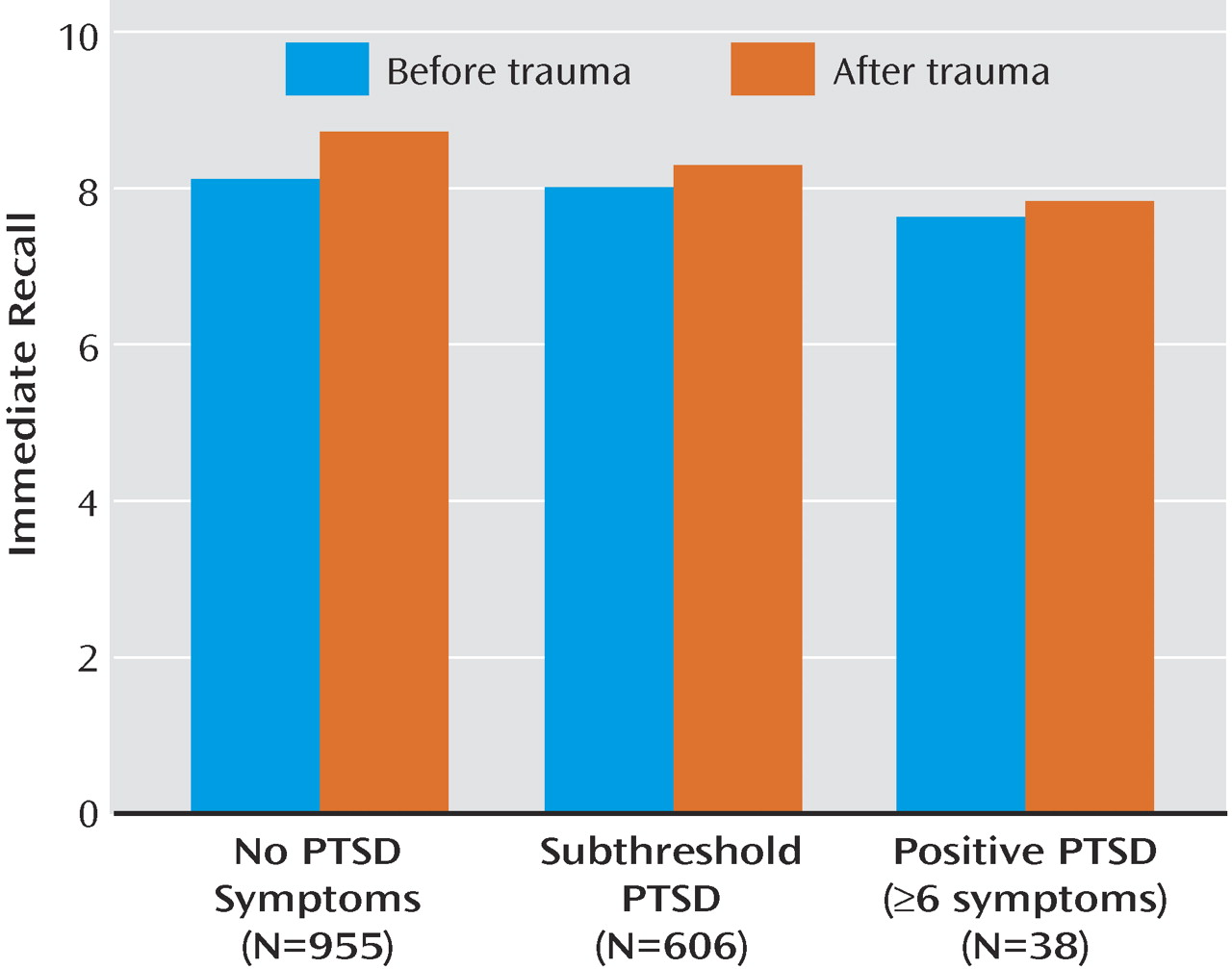
Table 1 presents results of the repeated-measures analyses of the changes in neurocognitive scores for the three groups: those with no symptoms, those with subthreshold PTSD, and those who screened positive for PTSD. The analyses controlled for age, gender, education, degree of exposure to the fire, time since the fire, depressive symptoms, and hazardous or harmful alcohol consumption. Individuals with higher levels of PTSD symptoms had significantly lower scores on the five neurocognitive measures: immediate recall (see
Figure 1 ), delayed recall, the digits backwards test, Symbol-Digit Modalities Test, and verbal intelligence both before and after the trauma.
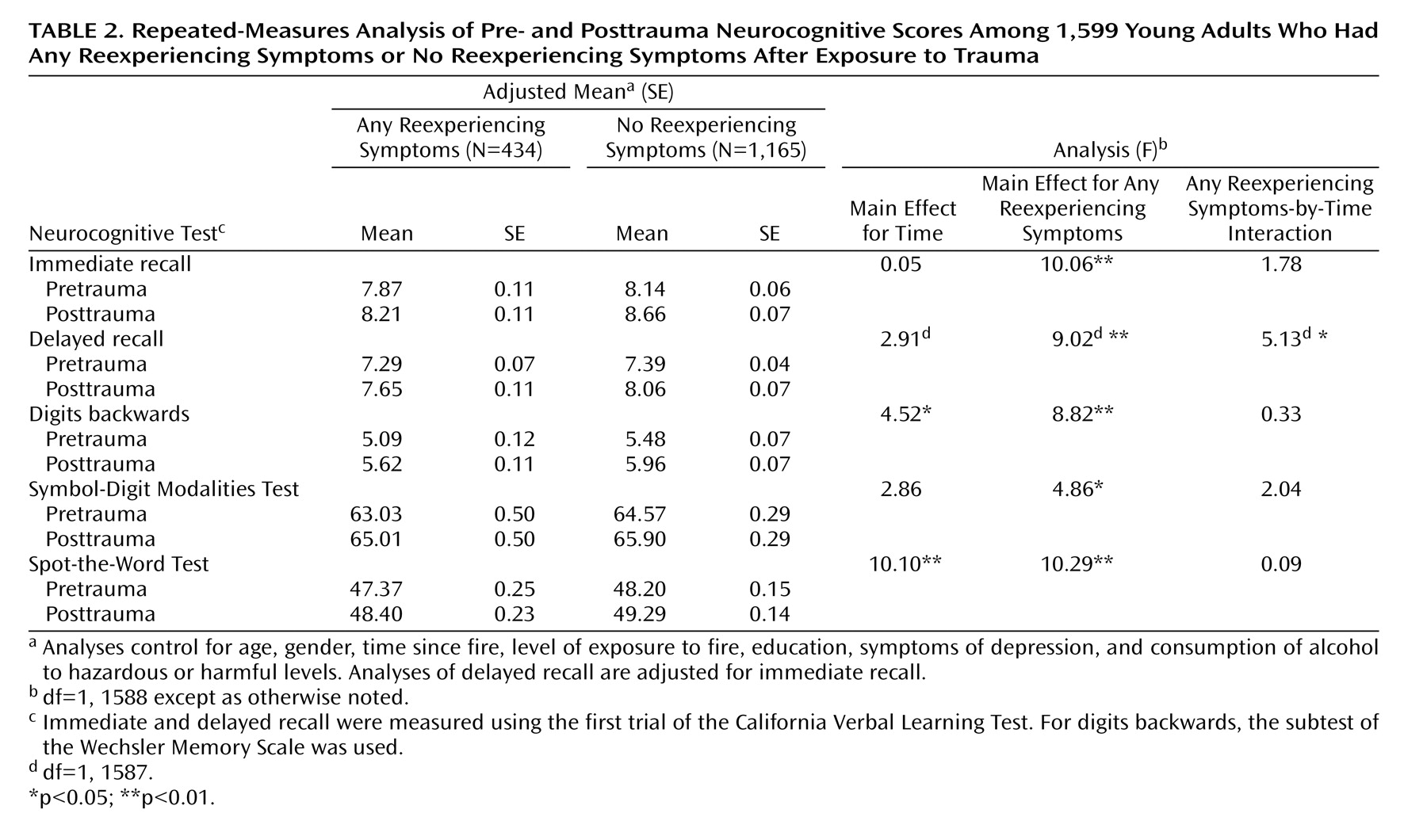
Table 2 presents results of the analyses examining associations between reexperiencing symptoms and pretrauma and posttrauma neurocognitive scores. Again, those who reported having any reexperiencing symptoms at least twice during the week preceding their second interview had significantly lower pretrauma and posttrauma scores on all tests.
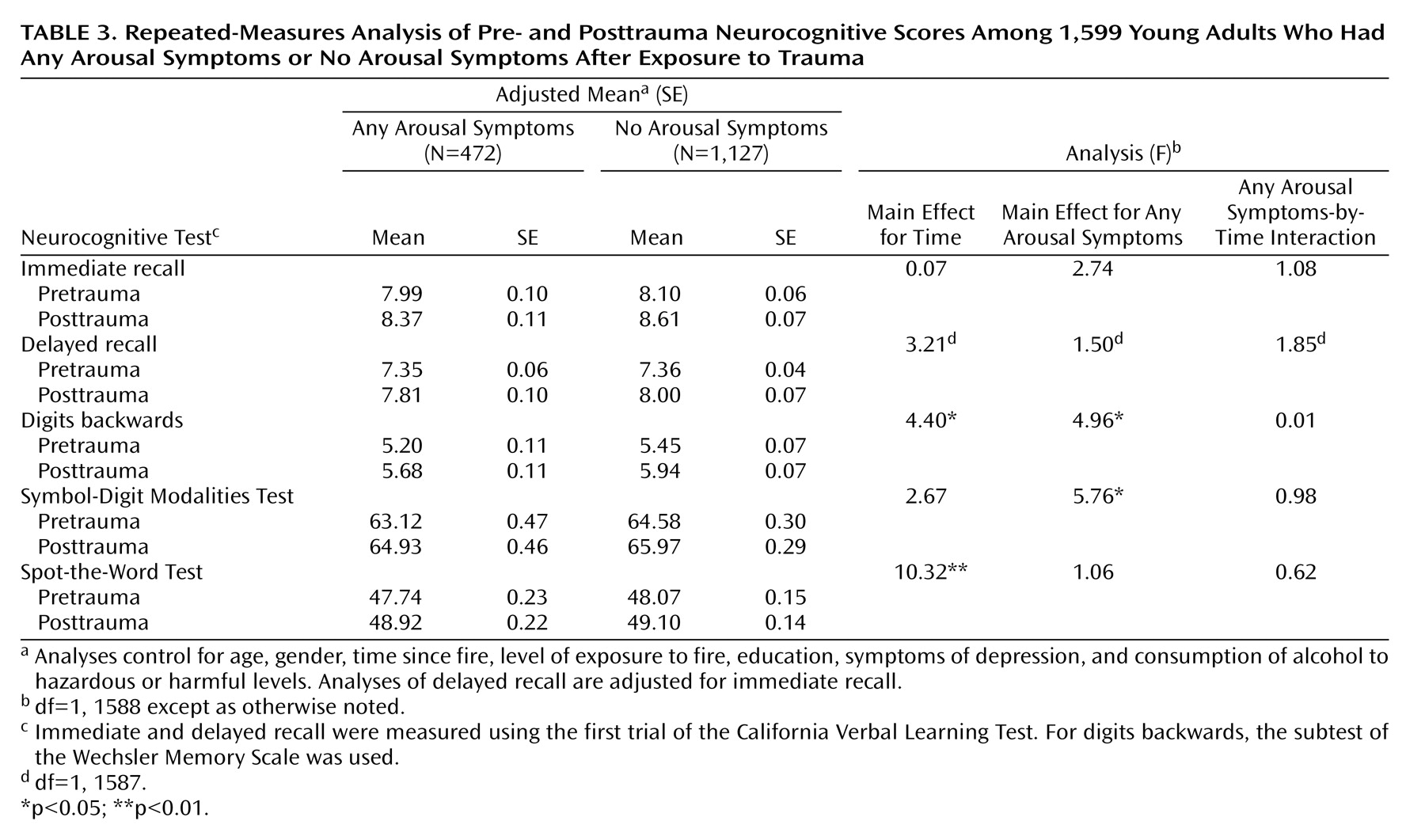
Table 3 presents the analyses examining associations between arousal symptoms and neurocognitive measures. Participants who reported any arousal symptoms had significantly poorer scores on the digits backwards test and the Symbol-Digit Modalities Test both before and after their experience of the trauma. (Additional data are presented in larger versions of Tables 1–3 in a data supplement that accompanies the online version of this article.)
Time Effect
In all analyses, there was a significant increase in participants’ scores on verbal intelligence and the digits backwards test over the 4-year period between wave 1 and wave 2.
Time-by-PTSD Measure Interaction
We found a significant time-by-PTSD measure interaction in the first analysis. The improvement in scores for immediate recall from wave 1 to wave 2 was significantly lower for participants who reported higher levels of PTSD symptoms. The mean improvement in adjusted immediate recall score was 0.60 for those with no symptoms, 0.28 for those with subthreshold symptoms, and 0.20 for those who screened positive for PTSD. A similar result was observed in the second analysis: those who reported any reexperiencing symptoms showed significantly less improvement in delayed recall scores compared with participants who had no reexperiencing symptoms. The mean improvement in adjusted delayed recall score for those with any reexperiencing symptoms was 0.36, compared with 0.67 for those with no such symptoms.
Discussion
We compared pre- and posttrauma functioning on several neurocognitive measures for 1,599 young adults who were interviewed for a longitudinal epidemiological study before and after a major natural disaster occurred in the region in which they lived. As expected, our findings consistently showed that participants improved in verbal intelligence, word recall, and digit span when reinterviewed, a change attributable to practice effects
(32) . On the second interview, however, those who had higher levels of reexperiencing and arousal symptoms as a result of the disaster had significantly less improvement in their word recall scores on the California Verbal Learning Test immediate recall test compared with those who reported no such symptoms. Those with any reexperiencing symptoms also had lower levels of improvement in delayed recall. These findings give some support to the view that highly stressful experiences may have a detrimental effect on verbal memory
(4,
5) .
The key and consistent finding in this study was that the development of the PTSD symptoms of reexperiencing and arousal was inversely associated with word recall, digit span, coding speed, and verbal intelligence, as assessed some 3 years before the trauma. Consistent with the position of Brewin and Smart
(15), we found that greater verbal working memory capacity was associated with lower risk of PTSD reexperiencing or arousal symptoms. However, our findings were not specific to working memory. Better performance on each of the available neurocognitive tests covering word recall, digit span, coding speed, and vocabulary was associated with a lower likelihood of reporting PTSD reexperiencing and arousal symptoms after the fire.
We found that participants who reported any reexperiencing symptoms of PTSD also had significantly lower scores on all five measures of neurocognition: immediate and delayed recall from the California Verbal Learning Test, the Symbol-Digit Modalities Test, the digits backwards test, and the Spot-the-Word Test. Associations between reexperiencing symptoms and these measures were considerably stronger than those for arousal symptoms. This differential effect of PTSD symptoms on neurocognitive abilities has been previously reported in a small study of 43 military veterans, 19 of whom had PTSD
(33) .
Previous studies reporting poorer posttrauma neurocognitive functioning in subjects with PTSD have been hampered by a number of limitations that we were able to address in this study. Most studies have been cross-sectional in design and did not have pretrauma measures for their participants. Where such measures have been available, they have usually been limited to data collected a number of years before, such as at time of enlistment for military service
(16) . By contrast, our study first collected neurocognitive measures from participants 3–4 years before the trauma and again within 18 months after the trauma.
Sample size and selection of comparison groups have also presented limitations in previous studies
(2) . Our sample comprised 1,599 young adults who had been exposed to a natural disaster, of whom 2.4% met screening criteria for a diagnosis of PTSD and 37.8% had subthreshold PTSD symptoms; the proportions reporting any reexperiencing or any arousal symptoms were 27.1% and 29.5%, respectively.
A number of previous studies have also been unable to take into account potentially confounding measures that could affect some measures of neurocognitive functioning. Our analyses controlled for various factors that could help explain poorer measures at initial interview, including experience of depressive symptoms and hazardous or harmful levels of alcohol consumption. More commonly available potential confounders, including age, level of education, gender, time since trauma, and extent of exposure to trauma, were also taken into account in the analyses.
Limitations
An important limitation of our study is our measurement of PTSD. We used the Trauma Screening Questionnaire because it is brief and could be administered by self-report on a computer. When a cutoff of six or more PTSD symptoms is used, this instrument has been shown to have good sensitivity and specificity
(18) . However, the questionnaire does not assess level of fear, helplessness, or horror experienced by the trauma-exposed individual, nor does it obtain information about criterion C avoidance symptoms. Another limitation is the restricted number of neurocognitive measures on which the effects of posttraumatic stress could be measured. As noted, we selected the instruments we used because of their suitability for measuring cognitive change resulting from aging in a general population, not for examining associations between neurocognition and PTSD symptoms. Although our instruments primarily measured verbal abilities, the Symbol-Digit Modalities Test is a measure of performance intelligence
(34), and our major findings also applied to this measure in all three analyses. However, it is possible that had we included measures tapping into a broader range of neurocognitive functions, deficits in functioning may have been found following the traumatic event. The level of PTSD symptoms at the time of first interview may have affected participants’ wave 1 responses, but we did not collect PTSD-related data at that time. Finally, the generalizability of our findings is limited because our sample comprised only young adults 20–24 years of age at first interview.
PTSD symptoms of reexperiencing and arousal may result in a relative decline in some measures of verbal memory over time. Our findings also support the position that performing more poorly on neurocognitive measures after exposure to trauma cannot be attributed only to having PTSD symptoms; having poorer abilities in some neurocognitive measures may represent a vulnerability factor for developing symptoms of PTSD.