When compared to healthy subjects, patients with substance use disorders have been characterized by diverse maladaptive personality traits (e.g., references
1–4). Findings such as these have been frequently explained by the notion that personality traits may serve as risk factors for substance-related problems. Indeed, several longitudinal studies have implicated personality characteristics as predisposing vulnerabilities for the subsequent development of substance-related disorders. For example, young children
(5,
6), adolescents
(7), and college freshmen
(8) who later became alcoholic tended to be more impulsive, neurotic, nonconforming, and extraverted than those who did not develop drinking problems. High scores on measures of negative emotionality and behavioral disinhibition have also predicted the onset or age of expression of substance-related problems
(9,
10), and treated substance abusers who score high on neuroticism and low on conscientiousness have been found to be most likely to have a relapse within a 12-month period. Some personality theorists, such as Tellegen and colleagues
(11), have further specified that such personality traits are to a large degree heritable. This possibility is supported by a growing base of research in behavioral genetics indicating that between 40% and 50% of the variance in personality traits can be attributed to genetic factors
(12,
13).
Aside from the notion that certain maladaptive personality traits may play an important role in the development of substance use disorders, alternative explanations for this association include the possibility that chronic substance abuse is in turn associated with behavioral, cognitive, or affective changes that may be misinterpreted as stable personality characteristics. The social withdrawal, irritability, and negative emotionality often observed in patient groups may in fact be best attributed to substance-induced anxiety and depressive syndromes
(14,
15). Furthermore, evidence that maladaptive personality traits improve after successful substance abuse treatment supports the interpretation that these maladaptive “personality” traits may be at least in part acquired
(16,
17). In this way, specific maladaptive traits may be shaped, reinforced, or accentuated over time either because they facilitate acquisition of substances or because they help protect the individual from the salient negative life circumstances associated with substance use disorders.
The comparison of opposing explanations for the association of personality traits with substance use disorders has been hindered by specific methodological constraints of the existing literature. Among the most fundamental of these issues concerns the overreliance on patient groups in which, even in the context of longitudinal research designs, it often is impossible to separate risk factors for the development of substance abuse or dependence from the potentially enduring consequences of these disorders. A family study should therefore be particularly informative in this regard because of its ability to identify familial risk factors independently from the disorders with which they are associated. That is, as substance abusers and their non-substance-abusing relatives share both genetic and environmental factors, but not substance abuse itself, the concentration of personality traits among relatives unaffected by substance abuse or dependence would provide clearer support for their role as a true family-based risk factor.
In the present study we examined these issues within the context of a controlled family study of substance use disorders using direct diagnostic interviews of both probands and first-degree adult relatives. The study had two goals: 1) to examine whether individuals with substance use disorders (both probands and relatives) differ from those without substance use disorders on the personality traits measured by the Multidimensional Personality Questionnaire
(18) and 2) to examine the concordance of these personality traits among relatives who do not have substance use disorders but who have a family history of this condition. If personality traits are familial risk factors for substance use disorders, then relatives without substance use disorders but having a positive family history for these conditions should differ from unaffected relatives without a positive family history. In order to control for the confounding influence of common forms of psychopathology, in all analyses we adjusted statistically for comorbid anxiety, affective, and antisocial personality disorders.
Method
Subjects
The study group comprised 325 probands and 262 of their first-degree adult relatives participating in the Yale Family Study, a family study investigating the relation between substance use disorders and anxiety disorders in families. In order to minimize bias associated with treatment seeking (e.g., Berkson’s bias), subjects were recruited from both outpatient treatment facilities and the local community. Specifically, 69% were recruited from clinics specializing in the treatment of substance use or anxiety disorders at the Connecticut Mental Health Center or the APT Foundation in New Haven, Conn. The remainder of the subjects having substance use disorders (31%) and the comparison subjects were drawn from the same general geographic area as the clinic-recruited subjects through a random-digit telephone dialing procedure. The majority of the clinic-recruited subjects were interviewed at the end of treatment, and none was interviewed during the first 3 weeks of treatment. Subjects with lifetime comorbid affective disorders, antisocial personality disorder, or other nonpsychotic axis I disorders were not excluded from the study. Additional details regarding the methods used in the Yale Family Study are available elsewhere
(19–
21).
Procedure
After receiving a description of the study, the participants gave written informed consent to participate in the study. So that the two groups with substance disorders would be comparable (individuals recruited from treatment settings may differ from community residents on diverse clinical characteristics), all participating probands were interviewed directly by using current and lifetime versions of the modified Schedule for Affective Disorders and Schizophrenia
(22) to determine whether they met DSM-III-R criteria. Diagnoses were assigned initially by interviewers who were either psychologists or psychiatric social workers with clinical experience in psychiatric settings, and they were then reviewed by psychiatrists or psychologists who were blind to the diagnosis of the proband. Extensive effort was devoted to establishing the reliability of the diagnostic assessments. Kappa values derived from joint ratings of individual interviews were high for substance abuse (0.72–0.94) across the first three series of training sessions. The final “best estimate” diagnoses were based on all available information, including the diagnostic interview, family history reports, and a review of medical records. Probands were excluded if there was evidence of significant organic mental impairment or if they were found to have schizoaffective disorder or schizophrenia. The 325 subjects who completed the diagnostic and self-report assessments reflected four predominant categories of drugs of abuse/dependence—opioids (N=81), cocaine or stimulants (N=18), marijuana or sedatives (N=29), or alcohol (N=77)—and a fifth category representing no lifetime history of substance abuse/dependence (N=120). For the purposes of the present study, individuals meeting the criteria for the broader category of substance use disorder (abuse or dependence of any type) were compared to those without a substance use disorder.
A total of 262 first-degree adult relatives of the probands were also included in the investigation. Permission to contact the relatives was obtained at the initial interview, and an independent interviewer (blind to the diagnosis of the proband) was assigned to interview relatives. The interview procedures and diagnostic assessment of the relatives were identical to those for the probands, except that the majority of the relatives were interviewed over the telephone. In general, studies comparing the reliability of telephone and personal interviews have shown that there are no significant differences in reporting from the two types of interview
(23–
25).
Personality Assessment
The Multidimensional Personality Questionnaire
(18) was used in the current study because it measures three higher-order personality dimensions—positive emotionality, negative emotionality, and constraint—that are highly independent and match or closely resemble those used in prior substance abuse research. The questionnaire is a factor-analytically derived scale consisting of 300 self-report true/false questions that measure 11 primary personality dimensions and three higher-order traits considered to be pervasive and stable dimensions of personal style
(18). The instrument has demonstrated acceptable levels of validity and reliability
(18,
26,
27).
The questionnaire was designed to provide dimensional assessments of personality traits (or risk factors) rather than absolute thresholds for personality disorder. Individuals with high scores on the higher-order factor of positive emotionality tend to interact more actively, efficaciously, and pleasurably with their environment. Positive emotionality consists of four primary dimensions—well-being, social potency, achievement, and social closeness—and resembles extraversion
(28) and surgency (factor I) and agreeableness (factor II) from the “big five” personality factors
(29,
30). High scores on the second higher-order factor, negative emotionality, occur in individuals who frequently experience feelings of distress, hostility, and harassment in response to minor everyday adversities. Negative emotionality is defined primarily by stress reaction, alienation, and aggression, and it closely resembles neuroticism
(28) and emotional stability (factor IV). The third higher-order dimension, constraint, is most strongly associated with the primary dimensions of control, harm avoidance, and traditionalism. Because persons scoring high on this factor tend to adhere to traditional values and respond to their environment with caution, deliberation, and restraint, low constraint resembles behavioral disinhibition, impulsivity, and sensation seeking and has been related to Eysenck’s psychoticism
(28) as well as the dimensions of conscientiousness (factor III) and intellect/openness to experience (factor V). In addition, the personality trait of absorption was originally considered to be a broad personality factor that combined several primary traits that converge to reflect a tendency toward hypnotic susceptibility and self-altering experiences, including openness to experience, fantasy absorption, and dissociation. As such, this trait overlaps considerably with intellect/openness to experience (factor V). Nevertheless, absorption has been considered a distinctive personality dimension that does not load onto any of the higher-order traits
(27).
Data Analysis
The data analyses in this study included chi-square tests for n-way tables of categorical variables and analyses of variance for continuous data. The multivariate general linear models procedure of the SAS package (Cary, N.C., SAS Institute) was used to compare scores of different groups (based on lifetime diagnoses of substance use disorders) for each primary and secondary dimension of the Multidimensional Personality Questionnaire. A Bonferroni correction was applied to the alpha levels for the 11 primary comparisons and the three higher-order dimensions. The models included several covariates accounting for the effects of gender, age, and socioeconomic status (based on Hollingshead score). In addition, as comorbid psychopathology varied by both recruitment source and substance use disorder status, all analyses controlled for comorbid affective, anxiety, and antisocial personality disorders.
Results
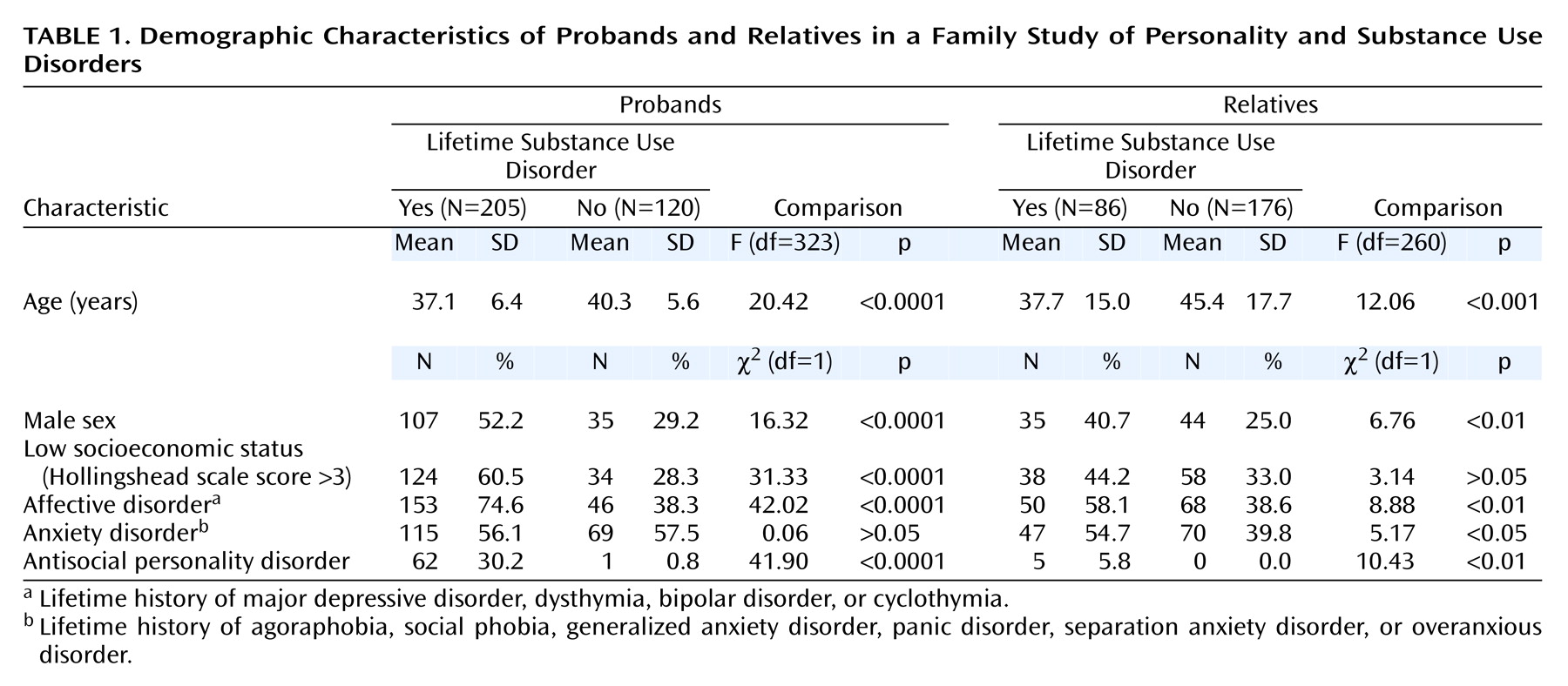
A description of the 325 probands who completed the Multidimensional Personality Questionnaire, and their relatives, appears in
Table 1, which is organized according to the presence or absence of substance use disorder. Significant differences across the proband groups were found for gender (women were less likely to have a substance use disorder), age (those with substance use disorders were younger), and socioeconomic status (those without a substance use disorder tended to belong to higher socioeconomic strata). Although the rates of anxiety disorders differed between subjects with and without substance use disorders only in the relatives, comorbid depression and antisocial personality disorder were concentrated among both probands and relatives with substance use disorders. As noted previously, all subsequent analyses controlled for these sources of variance in examining the association of personality with substance use disorders.
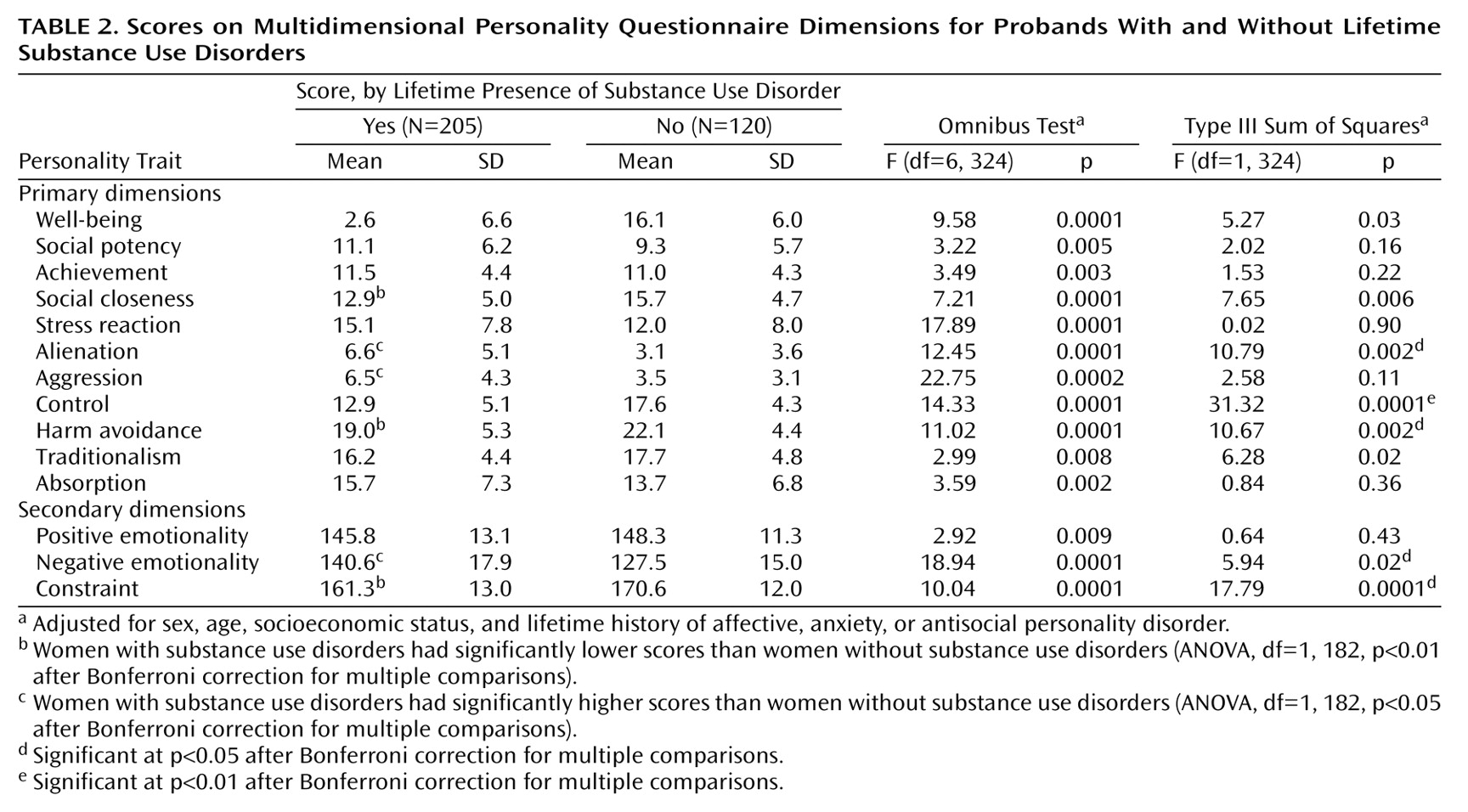
Personality Traits in Probands and Relatives With Substance Use Disorders
Table 2 presents the scores on the primary and secondary dimensions of the Multidimensional Personality Questionnaire scales for the probands with and without substance use disorders. The probands with substance use disorders scored higher on the primary dimension of alienation and lower on control and harm avoidance. In terms of the higher-order traits, the probands with substance use disorders also displayed higher mean scores for negative emotionality and lower scores for constraint. The findings were generally similar among men only and among women only, although more significant differences were found for the women. Both men and women with substance use disorders scored lower on control, but the women also had lower mean scores for social closeness, harm avoidance, and constraint and higher scores for alienation, aggression, and negative emotionality.
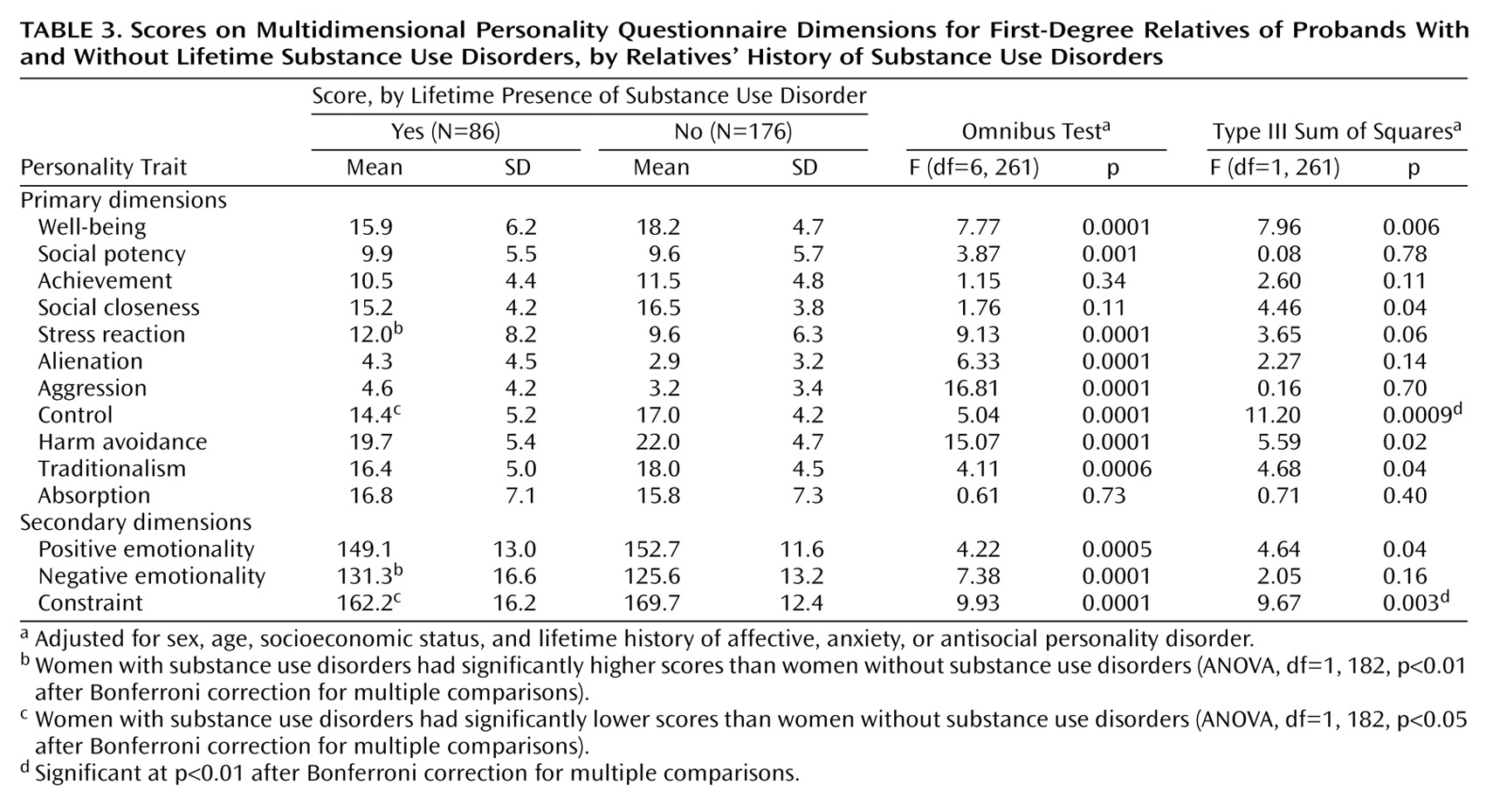
Table 3 presents scores on the primary and secondary dimensions of the Multidimensional Personality Questionnaire for the first-degree relatives. The findings are similar to those reported for the probands with and without substance use disorders. The total group of substance-abusing relatives had lower scores than the non-substance-abusing relatives on the primary dimension of control and on the higher-order trait of constraint. Female substance abusers scored higher on stress reaction and negative emotionality and lower on control and constraint.
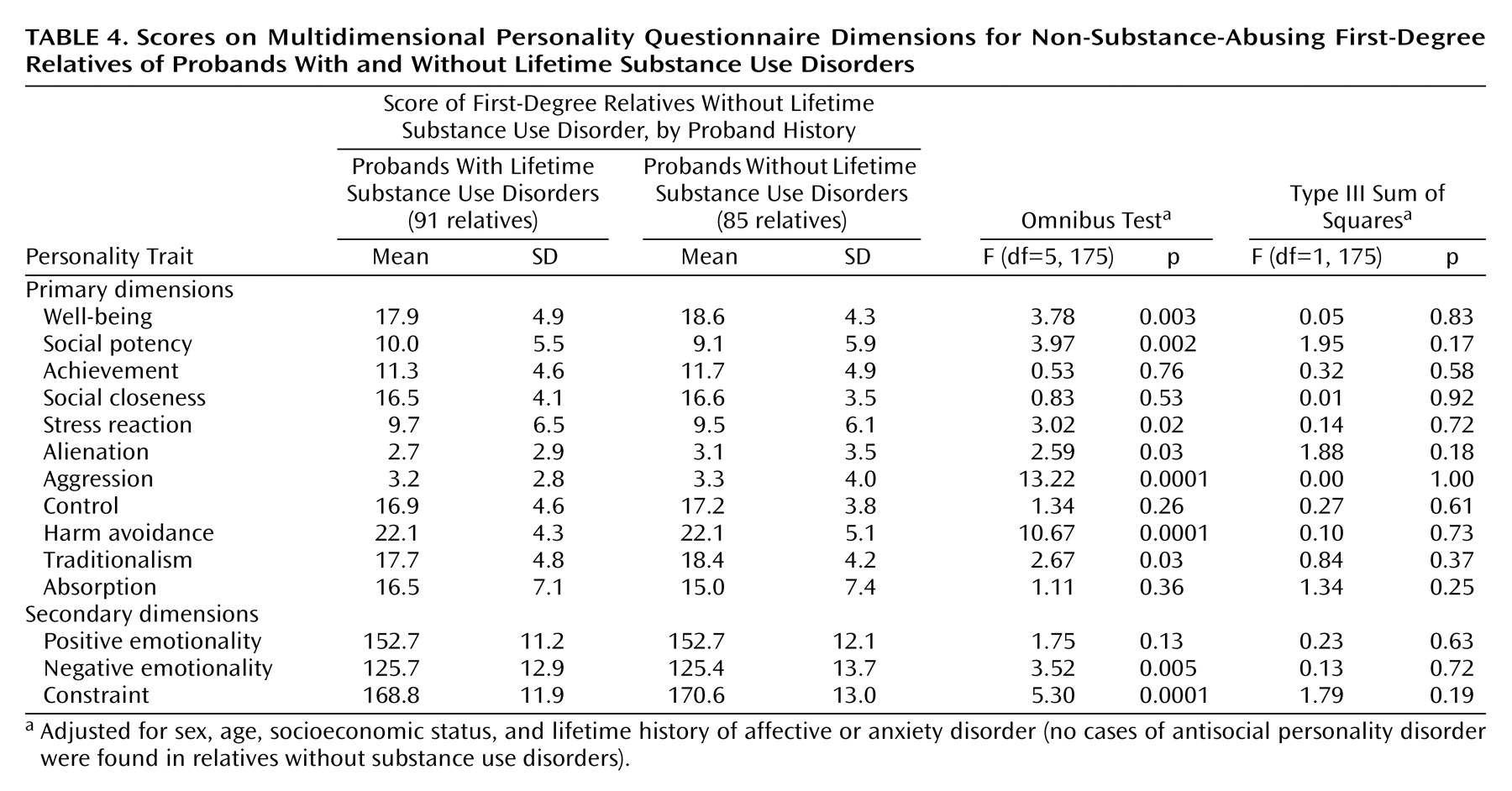
Personality Traits in Relatives Without Substance Use Disorders
Although the findings presented in
Table 2 and
Table 3 attest to the association of specific personality traits with substance use disorders, a series of analyses were conducted to examine the possibility that these personality traits represent familial risk factors for the development of substance use disorders. In order to control for the possibility that personality traits can be influenced by substance abuse or dependence, these analyses compared only the relatives without substance use disorders themselves but having or not having a family history for this condition (as defined by proband status). As demonstrated by
Table 4, no significant differences were observed concerning any of the Multidimensional Personality Questionnaire dimensions. When these analyses were replicated by selecting only the siblings of probands with and without substance use disorders (to control for cohort effects), again no significant differences emerged. From the numbers of subjects presented in
Table 4, a post hoc power analysis of the models reported for relatives without substance use disorders demonstrated over 0.95 power for detecting the same magnitude of effects as reported in previous tables.
Discussion
The concentration of specific personality traits among individuals with substance use disorders is a topic of considerable importance for improving both clinical and public health interventions. Among the diverse explanations for this association, the present investigation tested the specific hypothesis that maladaptive personality traits are familial risk factors for the development of substance use disorders. This mechanism of association was tested within the context of a large-scale controlled family study that used direct diagnostic interviews with probands and adult first-degree relatives. All analyses controlled for biases introduced by comorbid psychopathology and multiple comparisons.
Concerning the general association of personality traits with substance use disorders, the findings are similar to previous results indicating that substance abusers differ from people without substance use disorders on diverse personality dimensions
(1–
4). Specifically, the subjects with substance use disorders differed on the dimensions of alienation, control, harm avoidance, and the higher-order traits of negative emotionality and constraint. Women with substance use disorders differed on more personality dimensions than did men, a result that is also consistent with the notion that substance use disorders are less normative, and therefore potentially more pathological, in women
(31,
32). Relatives with substance use disorders likewise differed from comparison relatives on the dimensions of control and constraint, and female relatives with these conditions also had higher scores for stress reactivity and negative emotionality. Although the effects in relatives are somewhat smaller than those in probands, a finding that is not unexpected in light of Berkson’s bias, the results overall indicate an association between behavioral undercontrol and substance use disorders
(1,
4,
32–35). Not only do such findings have potential etiologic implications for the identification of risk factors for substance use disorders, but the presence or absence of these traits may also play an important role in determining treatment success and continued abstinence. The identification of persons at high risk on the basis of such personality dimensions may therefore serve as an important source of information for both treatment and prevention efforts.
The most novel contribution of the present study concerns its test of the hypothesis that the personality traits observed in substance abusers are familial risk factors
(11). In order to constitute a true family-based risk factor for substance use disorders, a reasonable assumption is that maladaptive personality traits should be observable among persons who are free of a diagnosis of substance use disorder but who have a first-degree relative with this condition (in the absence of full penetrance). The second set of analyses therefore compared only non-substance-abusing relatives of substance abusers to non-substance-abusing relatives of probands without substance use disorders, and they again corrected for the multiple comparisons. On the basis of this conservative approach, no evidence was found that the specific personality traits observed to be associated with substance use disorders could be conceptualized as familial risk factors for this disorder. Furthermore, a post hoc analysis confirmed that these nonsignificant results were observed despite adequate statistical power. Such findings therefore argue for caution in characterizing the personality correlates of substance use disorders as representing familial or heritable risk factors.
The strengths of the present investigation include the use of data from a controlled family study in which diagnostic interviews were administered directly to probands and their first-degree relatives, as well as the application of rigorous criteria for testing models of association between personality traits and substance use disorders. However, several methodological characteristics are important to consider in drawing broader conclusions. In this study we did not attempt to distinguish among the potentially diverse nonheritable explanations for the concentration of specific personality traits among subjects with substance use disorders. Similarly, despite procedures aimed at minimizing the risk that the links between personality and substance use disorders were due to the effects of acute substance abuse, this possibility remains an important consideration. An additional limitation is that these subjects had high rates of comorbid psychopathology (anxiety, mood disorders, and antisocial personality disorder), and such conditions may affect the generalizability of findings to other populations. Future investigations may benefit not only from testing specific nonheritable mechanisms of association, but also from examining them in relation to specific classes of substances.