Long-standing controversy has surrounded the question of whether there are specific clinical and biological risk factors in patients with major psychotic disorders and comorbid anxiety symptoms/disorders. Numerous reports over the years have suggested such an association between schizophrenia spectrum disorders and obsessive-compulsive disorder (OCD)
(1–
8) and panic disorder
(9–
11), with occurrence rates ranging from 1.1% to 60.0% for OCD and from 6.0% to 63.0% for panic disorder. In addition, earlier literature
(3,
12) has suggested that the presence of obsessive-compulsive symptoms in schizophrenia may be associated with a better long-term outcome. However, more recent studies
(1,
6,
13) have reported worse treatment outcome and greater impairment in neuropsychological functioning associated with obsessive-compulsive symptoms. Many of these studies suffer from various methodological shortcomings, such as small study groups, biased patient groups, and unstructured assessments. Specifically, many studies were conducted in large psychiatric institutions or day treatment centers among patients with chronic illnesses. In addition, some investigators used unstructured retrospective chart reviews or cross-sectional clinical assessments to diagnose comorbid anxiety disorders. Therefore, the clinical and biological significance of comorbid anxiety disorders in schizophrenia spectrum and other psychotic disorders remains unclear.
The present report, derived from a longitudinal study of first-admission patients with psychotic disorders, permitted us to examine the clinical significance of the association between schizophrenia and psychotic affective disorders presenting with comorbid anxiety symptoms/disorders in the early stage of illness. In this analysis, we examine three questions related to this early course association: 1) Is there a significantly greater occurrence of obsessive-compulsive symptoms or OCD among patients with schizophrenia/schizoaffective disorder than in those with affective psychoses (i.e., major depression or bipolar disorder with psychosis)? 2) Is there a greater occurrence of panic symptoms/panic disorder among patients with schizophrenia/schizoaffective disorder than in patients with bipolar psychosis or psychotic major depression? 3) Is the occurrence of obsessive-compulsive or panic symptoms at baseline assessment associated with worse clinical status at 24-month follow-up in these groups? In addition to addressing these issues, this report also focuses on the persistence, recognition, and treatment of anxiety symptoms identified at baseline and the incidence of new anxiety symptoms/disorders at the 2-year follow-up.
Method
The present study group is part of the Suffolk County Mental Health Project and was recruited between 1989 and 1995 from the 12 inpatient facilities in the county, including six community hospital units, a university hospital unit, a veterans administration hospital, an adult state psychiatric center, two private facilities (added in 1994), and a children’s state psychiatric center
(14). Inclusion criteria were first admission (or current admission within 6 months of first), aged 15–60 years, resident of Suffolk County, N.Y., and clinical evidence of psychosis, prescription of neuroleptic medication, and/or an admission facility diagnosis indicating psychosis. Exclusion criteria were moderate or severe mental retardation, an inability to speak English, or inability to provide written informed consent.
This report is a post hoc analysis that focuses on respondents diagnosed at the 24-month follow-up with DSM-IV schizophrenia or schizoaffective disorder, bipolar disorder with psychosis, or major depression with psychosis. An initial baseline interview usually took place in the hospital 1–2 weeks after admission. A complete description of the study was provided, and written informed consent was obtained for subjects participating in the study so study staff could review medical records, talk with treating clinicians, and interview significant others. The follow-up interviews were conducted by the same interviewer when possible and took place for the most part in the home.
Measures
The diagnostic assessment was conducted by trained master’s-level mental health professionals and included the Structured Clinical Interview for DSM-III-R (SCID)
(15). The baseline SCID and other ratings combined symptom information obtained during the interview with material obtained from the medical record and from interviews with clinicians and significant others. Follow-up SCIDs were administered at the 6- and 24-month points. Specifics of the diagnostic procedure were detailed in a prior report (16). Briefly, after the 6- and 24-month interviews, diagnoses were assigned by consensus of two to four project psychiatrists after discussion of all relevant clinical information and DSM-IV criteria.
The presence of comorbid anxiety symptoms/disorders was based on their ascertainment during the SCID interviews at baseline and at the 24-month follow-up. A diagnosis of panic disorder required meeting full diagnostic criteria as defined in the SCID, while panic symptoms were defined as meeting the A criterion (a rating of 3) as described in the SCID (i.e., “one or more panic attacks have occurred that were [1] unexpected…and [2] not triggered by situations in which the person was the focus of others’ attention”). For comparability to earlier literature, we also examined whether patients met only this criterion (corresponding to “limited-symptom panic attacks”) or met this criterion plus four panic symptoms but did not meet full panic disorder criteria (“panic attacks”)
(17–
19). A diagnosis of OCD required meeting full diagnostic criteria as defined in the SCID, while obsessive-compulsive symptoms were defined as meeting at a minimum the symptomatic criteria as defined in the SCID (either obsessions that are recurrent and persistent ideas, thoughts, impulses, or images that are experienced at least initially as intrusive and senseless or compulsions that are repetitive and purposeful and intentional behaviors that are performed in response to an obsession or according to certain rules or in a stereotypical fashion). Facility diagnoses of anxiety disorders were abstracted from the discharge summaries of the first hospital admission, as were data regarding discharge medication prescriptions. Demographic data (age, gender, and marital status) were abstracted from the baseline interview.
Clinical data assessed at 24-month follow-up included 1) hospitalizations since baseline (rehospitalization/no new hospitalization), 2) presence or absence of psychotic symptoms as determined by the 24-month SCID interview, 3) 24-month course of illness based on the World Health Organization’s 8-point system
(20), results of which were grouped into three categories (full remission, partial remission, or continuous illness), 4) total score on the Global Assessment of Functioning Scale (from DSM-III-R) for the best month between the 6- and 24-month follow-ups, 5) total score on the Brief Psychiatric Rating Scale
(21) at the 24-month follow-up, 6) total score on the Scale for the Assessment of Positive Symptoms (SAPS)
(22) and the Scale for the Assessment of Negative Symptoms
(22) at 24-month follow-up, and 7) score on the Hamilton Depression Rating Scale
(23) at follow-up.
Analysis
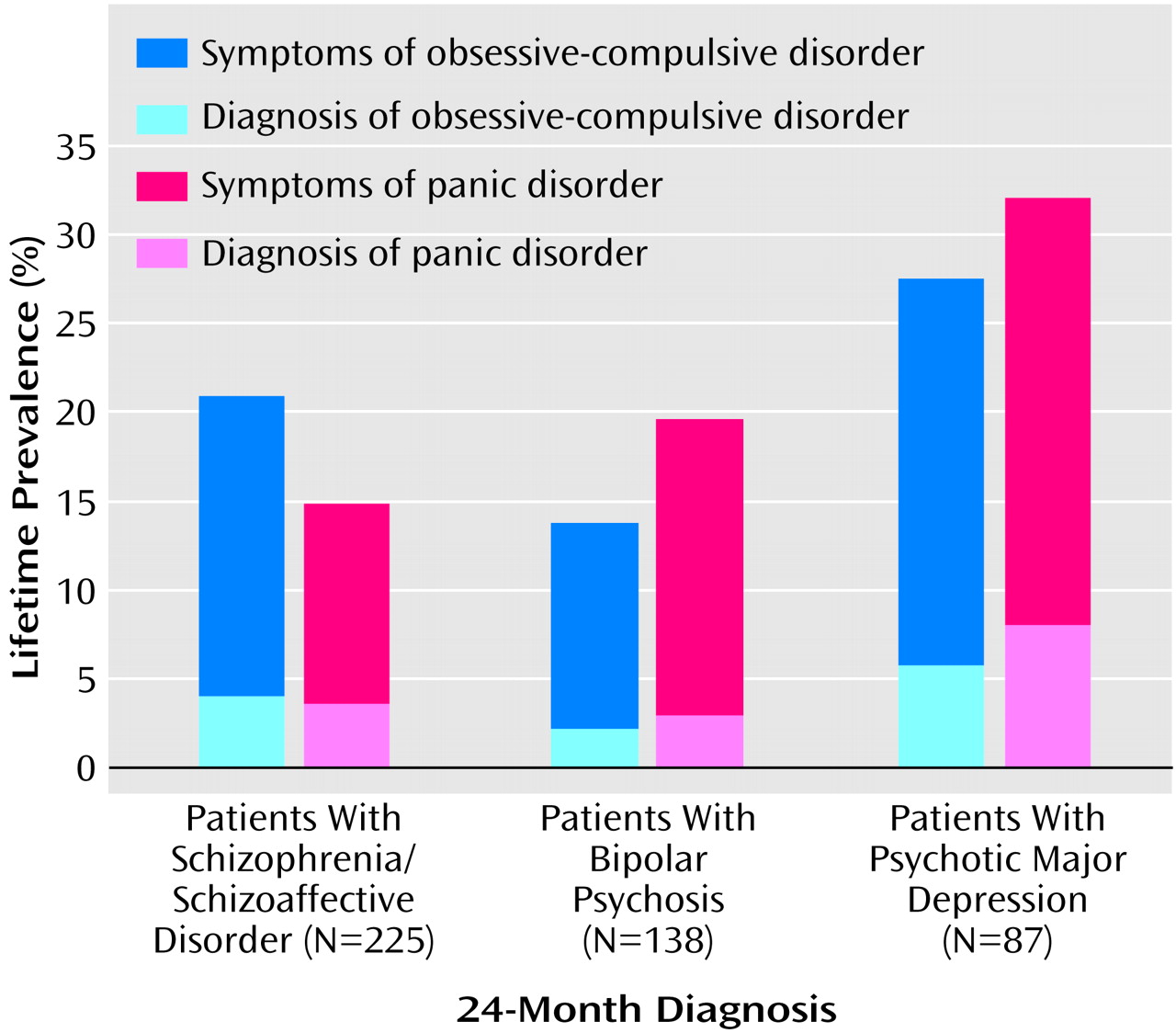
The initial (baseline) study group included 225 patients with schizophrenia/schizoaffective disorder, 138 patients with bipolar disorder with psychosis, and 87 patients with major depression with psychosis. Because of subject attrition or failure to complete a face-to-face 24-month interview and depending on whether the 24-month information was obtained directly from the respondent, the Ns for the 24-month outcome variables included in the analyses of symptom remission, incidence, and 24-month clinical status ranged from 167 to 169 for the patients with schizophrenia/schizoaffective disorder, 100 to 119 for the patients with bipolar disorder with psychosis, and 60 to 69 for the patients with major depression with psychosis. We combined the schizophrenia/schizoaffective disorder diagnostic categories for these analyses primarily because the small subset of patients with schizoaffective disorder (N=30, 13.3%, at baseline) precluded independent analysis.
Pearson chi-square tests were used for analysis of categorical variables and analysis of variance for continuous variables. In cases in which expected cell sizes were fewer than 5, Fisher’s exact test was used.
Results
Diagnosis-Specific Symptom Rates
The lifetime occurrence rates at baseline of obsessive-compulsive symptoms (16.2%, 73 of 450) and OCD (3.8%, 17 of 450) did not differ significantly across the three psychosis groups (obsessive-compulsive symptoms: χ
2=4.27, df=2, p=0.12; OCD: χ
2=1.94, df=2, p=0.38) (
Figure 1). Similarly, the rate of panic disorder (4.2%, 19 of 449) did not differ significantly by diagnosis (χ
2=3.99, df=2, p=0.14). However, the rate of panic symptoms was significantly higher in the subjects with major depression with psychosis (24.1%, 21 of 87) than in the subjects with schizophrenia/schizoaffective disorder (11.2%) or in the subjects with bipolar disorder with psychosis (16.7%) (χ
2=8.37, df=2, p<0.02). A separate analysis stratified by gender showed that this association was due to female patients with psychotic major depression having significantly higher rates of panic symptoms than other female patients (χ
2=8.04, df=2, p=0.02), whereas no significant association was found for male patients (χ
2=0.37, df=2, p=0.83). For all three diagnostic groups, the predominant pattern of panic symptoms was of attacks with limited symptoms (schizophrenia/schizoaffective disorder: 84.0%, 21 of 25; bipolar disorder with psychosis: 78.3%, 18 of 23; and major depression with psychosis: 71.4%, 15 of 21).
Among subjects who had no comorbid anxiety symptoms at baseline and had a 24-month SCID assessment, virtually identical onset rates of obsessive-compulsive symptoms (range=3.5%–4.3%) and OCD (range=0.0%–1.8%) were observed across the three diagnostic groups. In contrast, there was a significantly greater incidence of panic symptoms (15.2%, 7 of 46) and panic disorder (8.9%, 5 of 56) among the subjects with major depression with psychosis than among the subjects with schizophrenia/schizoaffective disorder (5.4%, 8 of 148; and 1.3%, 2 of 158, respectively) and bipolar disorder with psychosis (4.9%, 4 of 81; and 1.1%, 1 of 94) (panic symptoms: χ2=10.85, df=2, p=0.004; panic disorder: χ2=5.95, df=2, p<0.05).
Symptom Persistence
Of the subjects with obsessive-compulsive symptoms at baseline who were assessed with the SCID at the 24-month follow-up, 26.3% (10 of 38) of the subjects with schizophrenia/schizoaffective disorder and 21.1% (4 of 19) of the subjects with psychotic major depression, but none of the subjects with bipolar disorder with psychosis, still had symptoms 24 months later (χ2=5.12, df=2, p=0.08). Similarly, among those with OCD at baseline, 33.3% (3 of 9) of the subjects with schizophrenia/schizoaffective disorder and 40.0% (2 of 5) of the subjects with psychotic major depression, but none of the subjects with bipolar disorder with psychosis, were symptomatic 24 months later.
Among those with panic symptoms at baseline and a 24-month SCID assessment, 8.0% (2 of 25) of the patients with schizophrenia/schizoaffective disorder, 13.0% (3 of 23) of the patients with bipolar psychosis, and 19.0% (4 of 21) of the patients with psychotic major depression had these symptoms at 24-month follow-up. None of the patients with schizophrenia/schizoaffective disorder or bipolar disorder with psychosis who had panic disorder at baseline, but two other patients with bipolar disorder with psychosis (50%, 2 of 4), met the criteria for panic disorder at follow-up.
Demographic Correlates
Among the subjects with schizophrenia/schizoaffective disorder, there was no significant association between the presence of obsessive-compulsive symptoms at baseline and gender, ethnicity, or marital status, but a significantly greater proportion of those with obsessive-compulsive symptoms (39.5%, 15 of 38) than those without such symptoms (19.9%, 37 of 186) were age 21 or younger (χ2=6.89, df=1, p=0.009). No significant associations were found between the demographic variables and lifetime panic symptoms.
Because of small group sizes, the two affective disorder groups were combined for these analyses. There were no significant associations of age, gender, ethnicity, or marital status with the presence of obsessive-compulsive symptoms. However, panic symptoms occurred more frequently in women (27.5%, 33 of 120) than in men (10.6%, 11 of 104) (χ2=10.31%, df=1, p=0.001).
24-Month Clinical Status
Among subjects with schizophrenia/schizoaffective disorder, there were no significant associations between the presence of obsessive-compulsive symptoms and clinical functioning at the 24-month follow-up. In contrast, the subjects with schizophrenia/schizoaffective disorder and baseline panic symptoms were significantly more likely to have psychotic symptoms at follow-up (65.0%, 13 of 20) than those without panic symptoms (36.0%, 59 of 164) (χ2=6.31, df=1, p<0.02) and a higher SAPS score (mean=1.20, SD=0.97, versus mean=0.76, SD=0.80, respectively) (t=–2.01, df=163, p=0.05). Among the subjects with affective psychosis, there were no significant associations between the presence of either obsessive-compulsive or panic symptoms and any of the 24-month clinical status measures.
Anxiety Symptoms at Baseline
A total of 10% or fewer subjects from all three psychosis subgroups with obsessive-compulsive symptoms at baseline had obsessive-compulsive symptoms noted in their discharge summaries (schizophrenia/schizoaffective disorder: 10.5%, 4 of 38; bipolar disorder with psychosis: 6.3%, 1 of 16; major depression with psychosis: 10.5%, 2 of 19). Even fewer of those with baseline panic symptoms had panic symptoms noted in their discharge summaries (schizophrenia/schizoaffective disorder: 0%; bipolar disorder with psychosis: 4.3%, 1 of 23; major depression with psychosis: 4.8%, 1 of 21). However, despite the lack of recognition of the anxiety symptoms, 18% or more of subjects in all three psychosis categories with baseline obsessive-compulsive symptoms received specific anti-obsessional drugs (selective serotonin reuptake inhibitors [SSRIs], clomipramine, or monoamine oxidase inhibitors) (schizophrenia/schizoaffective disorder: 18.4%, 7 of 38; bipolar disorder with psychosis: 25%, 4 of 16; major depression with psychosis: 31.6%, 6 of 19). A similar or greater proportion of those with baseline panic symptoms received specific anti-panic drugs (SSRIs, tricyclic antidepressants, and the like) (schizophrenia/schizoaffective disorder: 20%, 5 of 25; bipolar disorder with psychosis: 21.7%, 5 of 23; major depression with psychosis: 57.1%, 12 of 21) in most cases as treatment for associated depressive symptoms. Included in these numbers are three respondents (all with bipolar disorder with psychosis) who received a benzodiazepine (alprazolam for two patients with panic disorder and clonazepam for one with panic attacks). Most of the respondents with major depression with psychosis who did not receive an antidepressant at baseline received a nonaffective facility diagnosis.
Discussion
This study adds to the existing literature in several significant ways. Most earlier reports examined patient populations with chronic illness, raising the possibility that subjects with two coexisting axis I conditions might be more likely to be sampled, resulting in inflated occurrence rates. Our use of a first-admission study group reduced this likelihood. In addition, while this group cannot be considered an epidemiologically defined sample, it is still more representative than that in the only prior study
(24), to our knowledge, of obsessive-compulsive symptoms in first-admission schizophrenia patients, which drew its study group from consecutive admissions to a single facility. Our study is one of few that used a structured interview of demonstrated reliability to ascertain diagnoses of both psychosis and anxiety disorders and is the only study, to our knowledge, to reexamine these diagnoses at more than one point in time. This methodological approach minimizes the potential biases introduced by use of record reviews, cross-sectional assessments, lay interviewers, and other less structured approaches and allows for the determination of the persistence of the anxiety symptoms over time. Finally, our study design permitted us to examine the comorbidity of two sets of anxiety symptoms/disorders across three groups of patients with psychotic disorders. In this way, we were able to address questions regarding the specificity of comorbid associations and their impact on outcome using identical assessment techniques.
The major potential limitation of this study is the fact that the research identification of anxiety symptoms/disorders is solely based on the SCID interview, unlike the diagnosis of the psychotic disorders, which was based on best-estimate procedures
(16). In an attempt to address this issue, an individual review of each SCID interview was performed by a research clinician (T.C.) for each subject with a potential anxiety symptom or diagnosis. In addition, since the presence of anxiety symptoms/disorders was not a major focus of the parent study, it is unlikely that interviewer bias was present in that regard. Since interviewers tended to follow the same subjects over time and were instructed to carefully examine the symptom profiles elicited in earlier interviews, it is unlikely that our finding of considerable symptom remission at follow-up was due to failure to adequately probe for these symptoms. Since the primary focus of the parent study was psychosis, we did not include assessment instruments more specific to anxiety disorder symptom profiles, such as the Yale-Brown Obsessive Compulsive Scale
(25,
26). Another limitation that bears mentioning is the fact that about one-fourth of participants were either not available for follow-up or did not have a follow-up SCID interview. We compared the diagnostic and demographic characteristics of the subjects with full 24-month interviews (including SCID results) (N=426), those who had an abbreviated 24-month visit (N=100), and those who were lost to or refused further follow up (N=108) to the full group. No significant differences were found for diagnosis, sex, race, age, socioeconomic status, or lifetime substance abuse. However, those who were assessed with the SCID were less likely to have ever married (33.7%) than those in the abbreviated-interview group (44.7%) and those who were lost to or refused further follow up (44.3%) (χ
2=6.61, df=2, p<0.04). Since marital status was not significantly associated with any of the study variables at baseline, it is unlikely that this may have affected our findings. Finally, we must note that the fact that informed consent was obtained may have inadvertently introduced a selection bias against anxious respondents, although this limitation would have been common to all such studies.
Our findings permit the following conclusions regarding the study questions. First, the rates of obsessive-compulsive symptoms or OCD were not higher in the patients with schizophrenia/schizoaffective disorder than in the two groups with affective psychotic disorders. Second, panic symptoms or panic disorder were significantly more prevalent among female patients with major depression with psychosis than among either patients with schizophrenia/schizoaffective disorder or bipolar disorder with psychosis. Third, while the baseline presence of obsessive-compulsive symptoms was not significantly associated with any of the 24-month clinical measures, the baseline presence of panic symptoms was significantly associated with the presence of positive psychotic symptoms at 24-month follow-up only among the subjects with schizophrenia/schizoaffective disorder. We must stress, however, that our findings are derived from respondents relatively early in the course of their psychotic disorder and are not directly comparable to findings in past study groups with more chronic illnesses.
However, our longitudinal findings suggest a much more complex picture than that presented in earlier studies. For example, during the 24-month follow-up, there was an incidence of newly reported obsessive-compulsive symptoms and OCD roughly equal to about one-third of the lifetime prevalence rate found at baseline, with an incidence rate of panic symptoms or panic disorder that was about one-half (for patients with schizophrenia/schizoaffective disorder or bipolar disorder with psychosis) to two-thirds (for patients with major depression with psychosis) of those found at baseline. Concomitantly, for all three groups at 24-month follow-up, there was remission of obsessive-compulsive symptoms in two-thirds to three-quarters of the subjects with these symptoms at baseline and a remission in 75%–80% of those with panic symptoms or panic disorder at baseline. The reason for this dramatic fluctuation in anxiety symptoms is not clear. For example, Zetin and Kramer
(27) have characterized the long-term course of OCD (without comorbid psychosis) as “remarkably variable and unpredictable,” citing several studies showing marked temporal fluctuations
(28,
29). In addition, the method of case ascertainment may contribute to this variation. Nelson and Rice
(30), using the National Institute of Mental Health Diagnostic Interview Schedule, a lay-interviewer-administered diagnostic instrument, reported that only 19.2% of the respondents meeting DSM-III criteria for lifetime OCD at wave 1 continued to meet lifetime criteria at 1-year follow-up. In one of the few studies to compare lay and clinician (SCID) interviews in the same sample, Stein et al.
(31) found a greater than threefold difference in the 1-month prevalence of OCD (3.1% for lay interviews versus 0.7% for clinician interviews). Finally, Regier et al.
(19), using Epidemiologic Catchment Area data, reported the wave 1 prevalence of OCD to be 1.3% in the general population, to which was added a 1-year incidence of 0.8%, yielding a wave 2 lifetime prevalence of 2.1%. This suggested that there may be a substantial influx of incident cases over time, which was similar to our finding. Our SCID-derived rates of lifetime OCD at baseline ranged from two to six times higher than those reported in the general population but are considerably lower than those cited for groups of patients with psychosis and more chronic illness (e.g., 7.8%–26.0% of patients with schizophrenia/schizoaffective disorder [
2,
7], 13%–30% of patients with bipolar disorder with psychosis, and 12.5%–21.0% of patients with major depression with psychosis [
32–
35]). However, the OCD 24-month incidence rate seen in our study group suggests that the lifetime rate of comorbidity may increase with age and the chronicity of the disorder.
Studies using lay interviews
(19,
36) have reported the lifetime prevalence of panic disorder in the general population to range from 0.4% to 3.6%, while one of the few studies to use a clinician interview (SCID)
(17) found a lifetime prevalence of 3.8% for panic disorder. Our findings for baseline rates for panic disorder in patients with schizophrenia/schizoaffective disorder and bipolar disorder with psychosis are comparable, while the rate for our patients with major depression with psychosis was two to three times higher. However, as our patients had comorbidities with psychoses, our rates are considerably lower than those found in other studies
(35,
37–39) (e.g., 12%–38% in patients with bipolar disorder with psychosis and 10%–37% in patients with major depression with psychosis). This discrepancy may also reflect the chronicity of the underlying illness, since one of the few studies of newly admitted patients
(40) showed that 2.1% of the patients with bipolar I disorder met criteria for panic disorder, which is similar to our result.
Lifetime prevalence rates of 6.5%–16.4% have been reported for panic symptoms in general populations
(18,
19) (7.8% using the SCID), which are similar to our findings but again lower than those found in studies using lay interviews in patient groups
(41) (28%–63% for schizophrenia/schizoaffective disorder, 18%–53% for bipolar disorder with psychosis, 24%–42% for major depression with psychosis). Several studies have found, as we have, that attacks with limited symptoms predominate, although one study using the SCID
(17) found full panic attacks to be more common.
Thus, our occurrence rates for both obsessive-compulsive symptoms/OCD and panic symptoms/panic disorder at baseline were generally equal to or higher than those reported in the general population but lower than those found in patient samples with more chronic illnesses. Our observation of a relatively substantial incidence of these conditions over time suggests that the lifetime occurrence rates in groups of patients with psychosis may be correlated with age or duration of illness. We are currently conducting a 10-year follow-up examination of our group to test this hypothesis.
Regarding the recognition and treatment of anxiety symptoms/disorders, only about 10% of our subjects identified by means of SCID interview as having obsessive-compulsive symptoms were so recognized by the clinicians; the proportion of those with recognized panic symptoms was even lower. These findings are similar to those reported in a sample of patients with schizophrenia/schizoaffective disorder or bipolar disorder with psychosis by Cosoff and Hafner
(32), who also used the SCID and found that “almost none of those with anxiety disorders were [recognized or] being treated for them.” Since prior reports showing some of the highest rates for comorbid anxiety symptoms/disorders came from chart reviews, this observation suggests either that clinicians in earlier studies had a lower threshold for the recognition of these symptoms or that higher rates may have been related to the fact that most earlier reports dealt with more chronically ill patient groups, in which these symptoms may be more pervasive. Despite the clinicians’ limited recognition of obsessive-compulsive and panic symptoms, 20% or more of these subjects actually received treatment that was appropriate for a comorbid anxiety disorder (mainly for comorbid depressive symptoms), which may have altered the course of the anxiety disorder, resulting in less of an impact on 24-month clinical status.
However, it is unclear why the baseline presence of panic symptoms/disorder in patients with schizophrenia/schizoaffective disorder was associated with the presence of positive psychotic symptoms at 24-month follow-up, despite the fact that only 13.3% of these subjects retained panic symptoms at the 24-month follow-up. It is possible that the presence of panic symptoms at first admission serves primarily as a marker of vulnerability to continuing psychotic symptoms, even in the absence of active panic symptoms, and suggests the need for replication of this finding in similar study groups to determine its clinical and pathophysiological significance, as has been suggested in earlier reports
(10,
11,
42).
Earlier reports have also suggested that, based on clinical and neuropsychological profiles, schizophrenic patients with obsessive-compulsive symptoms should be carefully assessed and managed
(43). A number of investigators have reported positive responses to adjunctive treatment with SSRIs and clomipramine in patients with schizophrenia and obsessive-compulsive symptoms; they have also reported a marked reduction in obsessive-compulsive symptoms associated with neuropsychological improvement in previously refractory patients
(44). At present, it is not clear whether there is a subgroup of patients with schizophrenia and comorbid anxiety that could be best conceptualized as having a distinct schizophrenia syndromal subtype with prominent anxiety symptom dimensions or as a subset of schizophrenia patients with coexisting specific anxiety disorders, although the similarity of prevalence rates between the subjects with schizophrenia/schizoaffective disorder and those with affective psychosis tends to support the latter conclusion, at least in the early stages of illness.
While there is a need for replication of our findings in other groups of patients with recent-onset psychosis, our results suggest the need for further investigation of the possible link between the panic symptom profile at baseline and subsequent positive psychotic symptoms in patients with schizophrenia/schizoaffective disorder and any etiologic or therapeutic implications of this finding. On a clinical level, our findings support earlier suggestions of the need to use structured and systematized assessment tools (such as the SCID) in the diagnosis of recent-onset psychosis to facilitate the recognition and treatment of comorbid symptoms
(45).