The term “minor depression” has been used to describe depressive conditions that are not of sufficient severity and duration to meet criteria for a major depressive episode
(1–
6). DSM-III included a chronic form of minor depression as a diagnostic category (dysthymia), but minor depression lasting less than 2 years was folded in with atypical depression, identified as depressive disorder not otherwise specified in DSM-III-R. In DSM-IV, minor depressive disorder was identified as a potential diagnostic category that requires empirical validation. The proposed diagnostic criteria for minor depressive disorder required the presence of two to four symptoms of depression lasting for at least 2 weeks and excluded individuals with a previous history of major depressive disorder.
Epidemiologic studies, primarily based on the Epidemiologic Catchment Area (ECA) and National Comorbidity Survey databases, document the prevalence, societal costs, functional disability, and long-term consequences of minor depression
(3–
9). Although investigators have used a variety of definitions and analytic strategies, the overarching findings from these studies are as follows: 1) Minor depression has a point prevalence rate of 2%–5%. 2) Minor depression is associated with functional impairment and greater service utilization. 3) Minor depression is associated with a greater risk of developing major depressive disorder. 4) The presence of depressed mood or anhedonia (the “A criterion”) is associated with even greater dysfunction and risk of developing a future episode of major depressive disorder. 5) The greater the number of symptoms of depression, the greater the number of episodes, length of longest episode, degree of impairment, and likelihood of having a comorbid diagnosis and family history of psychiatric disorders. 6) Individuals with a history of major depressive disorder freely traverse between major depressive disorder, minor depression, and subsyndromal depressive symptoms
(3–
5,
8–14).
The most common symptoms reported for individuals with minor depression in the ECA data set are recurrent thoughts of death, insomnia, feeling tired all the time, trouble concentrating, poor appetite, and feelings of worthlessness
(4).
These data, as well as analyses of other large data sets
(15,
16), suggest that we need to broaden our conceptualization of depressive disorders. Kendler and Gardner’s 1998 longitudinal analysis of the Virginia Twin Registry
(16) demonstrated that the presence of five or more symptoms of depression was not a more accurate harbinger of depression at 1-year follow-up than the presence of three or four symptoms. Data from the NIMH Collaborative Study on Depression
(15) demonstrated that, following an entry episode of major depressive disorder, patients spent an average of 58% of the weeks during the next 9 years experiencing major depressive disorder (15% of the weeks), minor depression (27% of the weeks), or subsyndromal depressive symptoms (16% of the weeks). The confluence of these findings suggests that there may be value in considering depression as a spectrum of disorders rather than a single categorical disorder.
Despite considerable evidence of the prevalence and disability associated with minor depression, many questions remain. Is minor depression an evanescent phenomenon or an enduring and disabling condition? What is the nature of the relationship between minor depression and an individual’s personal or family history of major depressive disorder? Do these factors influence the qualitative presentation of minor depression? In this article we address the following hypotheses: 1) Minor depression is not evanescent. 2) There is a strong family history of unipolar disorder associated with minor depression. 3) A substantial number of individuals with minor depression previously have had episodes of major depressive disorder. 4) Minor depression shares mood and cognitive symptoms with major depressive disorder but not the neurovegetative and reverse neurovegetative symptoms of depression. 5) One cannot differentiate individuals with minor depression from one another on the basis of past history of major depression or family history of depression.
Method
Overview of the Study
Data for this report are derived from a comprehensive study of the diagnosis and treatment of minor depression. The study had three distinct phases: 1) an initial diagnostic evaluation followed by a 4-week single-blind placebo lead-in period; 2) a 12-week double-blind, placebo-controlled treatment phase; and 3) a 24-week randomized crossover continuation phase. In-depth discussion of the acute and continuation treatment study design and results will be presented elsewhere.
This descriptive report of minor depression is based on data from the placebo lead-in phase of the study. Demographic and clinical ratings presented here were obtained at the initial study visit. Data pertaining to the stability of symptoms and overall criteria for minor depression were obtained during the subsequent four weekly visits constituting the placebo lead-in period.
Subject Recruitment
The subjects were recruited at three sites (University of California, San Diego; University of Pittsburgh; and University of Texas, Southwestern Medical Center) primarily by means of advertisements in local newspapers. Some subjects were referred to the study by psychiatrists and family practitioners in the local community. A few subjects entered the study through referral from subjects already involved in research at the institution. After telephone screening, subjects were invited in for a diagnostic evaluation.
Subjects who were invited in for a diagnostic interview participated in the process of informed consent before this interview. Informed consent involved the subject’s reviewing a written document describing the study with the principal investigator’s staff, who answered any questions before the subject signed the consent form.
All subjects were at least 18 years of age, conversant in English, and willing to be available for participation in the 40-week study.
Evaluation of Subjects
Measures used for the initial evaluation of subjects included the Structured Clinical Interview for DSM-IV (SCID)
(17); the depression module of the National Institute of Mental Health Diagnostic Interview Schedule (DIS)
(18); the Medical Outcomes Study 36-item Short-Form Health Survey
(19); the 28-item version of the Hamilton Depression Rating Scale, which was also scored for the 17-item and 21-item versions
(20–
22); the Hamilton Anxiety Rating Scale
(23); the 30-item version of the clinician-rated Inventory for Depressive Symptomatology
(24); the Beck Depression Inventory
(25); the HSCL
(26); and the Clinical Global Impression (CGI) severity scale
(27). The extensive demographic evaluation of the subjects included determination of Research Diagnostic Criteria family history diagnoses. Subjects had to have normal physical examination and laboratory results, including a complete blood count, urine toxicology screen, urine analysis, and serum chemistries for hepatic and renal function.
Subjects were reevaluated weekly for the 4 weeks after study entry with the DIS depression section, Hamilton depression scale, Inventory for Depressive Symptomatology, Short-Form Health Survey, Global Assessment of Functioning Scale (DSM-III, p. 122), CGI severity scale, and CGI improvement scale.
Diagnostic Criteria for Minor Depression
In defining minor depression for this study, we made several methodological and conceptual decisions. First, at the inception of this study in 1992, the majority of available data regarding minor depression resulted from ECA analyses, which used the depression section of the DIS; therefore, we adopted the DIS as our primary diagnostic tool for defining minor depression. Second, anticipating concerns that minor depression might be perceived as trivial, we required that functional disability be evident according to scores on both the Global Assessment of Functioning Scale and at least one of two Short-Form Health Survey subscales. Third, we included subjects with a past history of major depressive disorder or dysthymia so that our study group would be more representative of the larger group of patients with minor depressive symptoms. However, to eliminate the possibility that the minor depression was a residual phase of another type of depressive episode, we did not include subjects who had experienced major depression or dysthymia within the last 2 years. Fourth, because the antidepressants used in treatment phases of this trial (serotonin reuptake inhibitors) are effective treatments for a variety of psychiatric disorders, we excluded individuals with any current axis I disorder.
To qualify as having “confirmed” minor depression, subjects in this study had to meet the following three criteria at the initial diagnostic visit and at least three of the four subsequent visits, including those during the last 2 weeks of the single-blind study period:
1. At least 2 weeks of depressed mood/dysphoria/sadness (DIS item 1) and pervasive loss of interest/pleasure in all or almost all activities (DIS item 2) and at least one additional depressive symptom group from the DIS or at least 2 weeks of depressed mood/dysphoria/sadness (DIS item 1) or pervasive loss of interest/pleasure in all or almost all activities (DIS item 2), but not both of these, and at least two additional depressive symptom groups from the DIS.
2. A Global Assessment of Functioning Scale score of 70 or less for the last month. (The time frame was decreased to the last week during the 4 weeks of single-blind evaluation.)
3. A score of 75 or less on the social role function scale or a score of 67 or less on the emotional role function scale of the Short-Form Health Survey for a time period including the last month.
Subjects who had developed five or more symptoms of major depressive disorder when they were interviewed with the DIS depression section were interviewed with the depression module of the SCID to determine whether their minor depression had progressed to major depressive disorder.
Exclusion Criteria
Exclusion criteria for the study were current major depressive disorder or dysthymia; major depressive disorder or dysthymia within the last 2 years; major depressive disorder in partial remission; loss of a loved one or significant other within the past year; serious suicidal risk; substance or alcohol abuse or dependence within the last year; a current diagnosis of any axis I disorder; a lifetime diagnosis of bipolar disorder (type I), borderline personality disorder, antisocial personality disorder, psychotic disorder, organic mood disorder, organic psychotic disorder, or schizophrenia; use of any psychotropic drug except chloral hydrate within 7 days or a monoamine oxidase inhibitor within 14 days of starting active treatment; the presence of a serious medical condition that was not currently stabilized; seizure disorder within the last year; a history of severe allergies or multiple adverse drug reactions; previous nonresponse or adverse reaction to fluoxetine; or previous participation in a fluoxetine study.
Statistical Analyses
Descriptive statistics are presented for key demographic and clinical characteristics of the study group. After evaluating continuous data for homogeneity of variance and normal distribution, we compared different study subgroups using t tests. Chi-square tests or Fisher’s exact tests were used to compare groups on categorical variables, and Wilcoxon rank sum tests were used for measures with ordinal values such as CGI and Short-Form Health Survey scales. A probability level of p=0.05 (two-tailed) was used to determine statistical significance of group differences. Group sizes for the two comparisons of interest (positive versus negative patient history of major depressive disorder and positive versus negative family history of depression) were considered sufficiently large to detect group differences. Since this is a descriptive report, statistics and resulting probability values are to be taken as descriptive indicators, not inferential ones.
Results
Of the 226 subjects who met criteria for minor depression at initial screening, 64 did not complete the 4-week lead-in phase of the study for the following reasons: adverse effects (N=4), lack of efficacy (N=5), withdrew consent or declined further participation (N=17), had contraindicated medical conditions (N=10), other protocol violations (N=3), were lost to follow-up (N=6), developed major depressive disorder (N=5), or no longer met criteria for minor depression (N=14). The 162 individuals (72% of the initial sample) who remained in the study for 4 weeks and continued to meet criteria for minor depression constitute the study group of subjects with confirmed and nontransient minor depression who are the focus of this report.
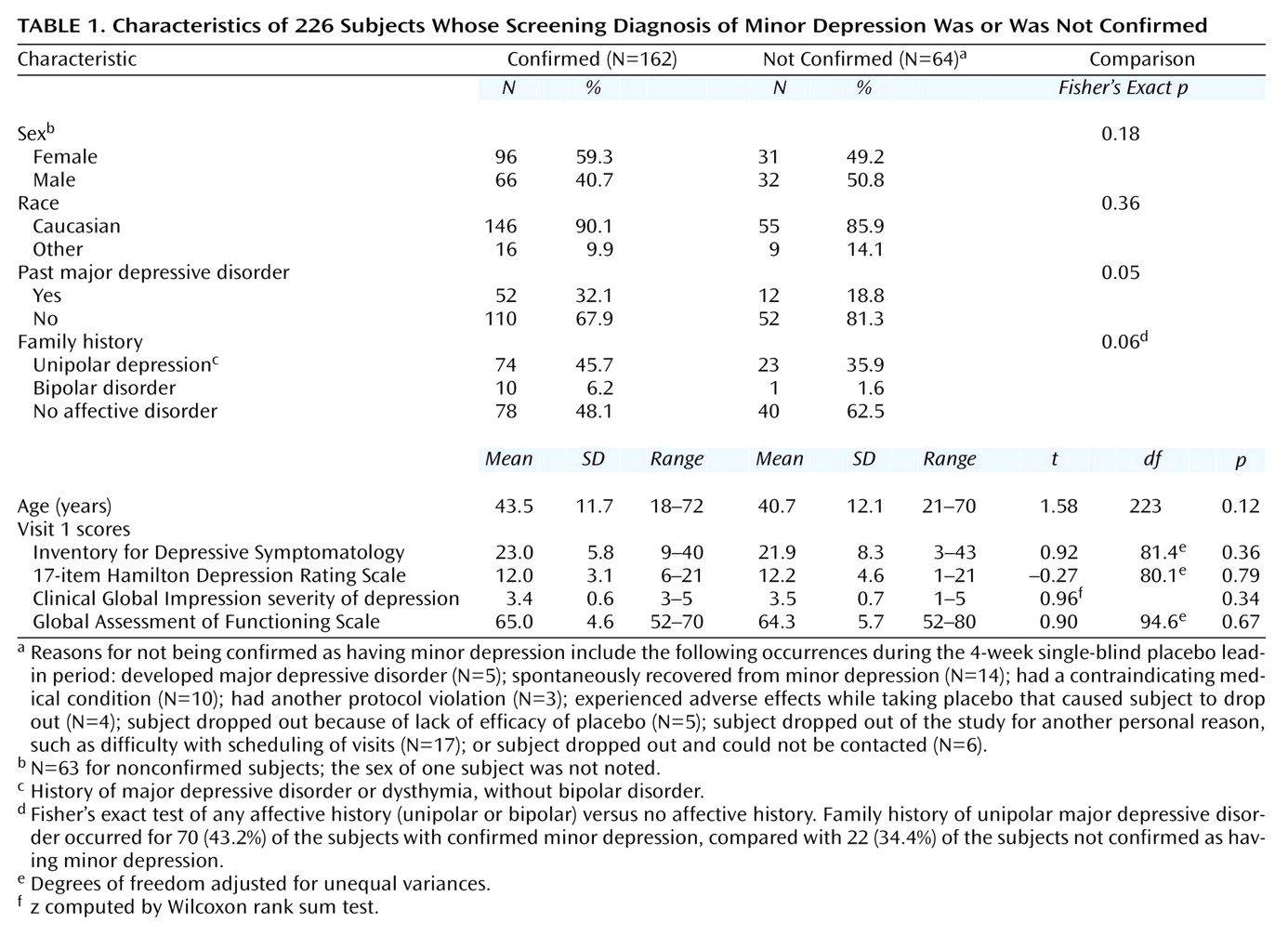
As shown in
Table 1, 59% of subjects with confirmed minor depression were women, 90% were Caucasian, and their mean age was 43.5 years. Overall, the 64 subjects excluded from the analyses did not differ significantly from the 162 patients with confirmed minor depression with respect to sex, race, age, family history of affective disorders, or initial symptom rating scale scores; however, they were significantly less likely to have a past history of major depressive disorder (
Table 1). The subgroups of subjects who withdrew, were excluded, or changed diagnostic status were fairly heterogeneous and too small for meaningful statistical comparison. The 14 subjects who spontaneously recovered from minor depression during the 4-week placebo lead-in phase tended to be the least severely ill on all clinical measures. The five subjects who developed major depressive disorder had clinical ratings similar to the top third of patients with confirmed minor depression. Patients who dropped out (N=17) or were lost to follow-up (N=6) constituted heterogeneous groups encompassing a wide range of depressive severity.
Thirty-two percent of the subjects with minor depression had a past history of major depressive disorder (
Table 1). They did not differ from the subjects without a past history of major depressive disorder on any demographic characteristic, family history variable, or clinical rating of severity or dysfunction.
Forty-six percent of the subjects with minor depression had a first-degree relative who had suffered from unipolar depression (major depressive disorder or dysthymia), and 6% had a first-degree relative with bipolar disorder (
Table 1). A positive family history of depression was associated with a higher total 17-item Hamilton depression scale score (mean=12.5, SD=3.0, versus mean=11.4, SD=3.1) (t=2.16, df=150, p=0.03). (A difference of 1.1 on the 17-item Hamilton depression scale usually is not clinically significant.)
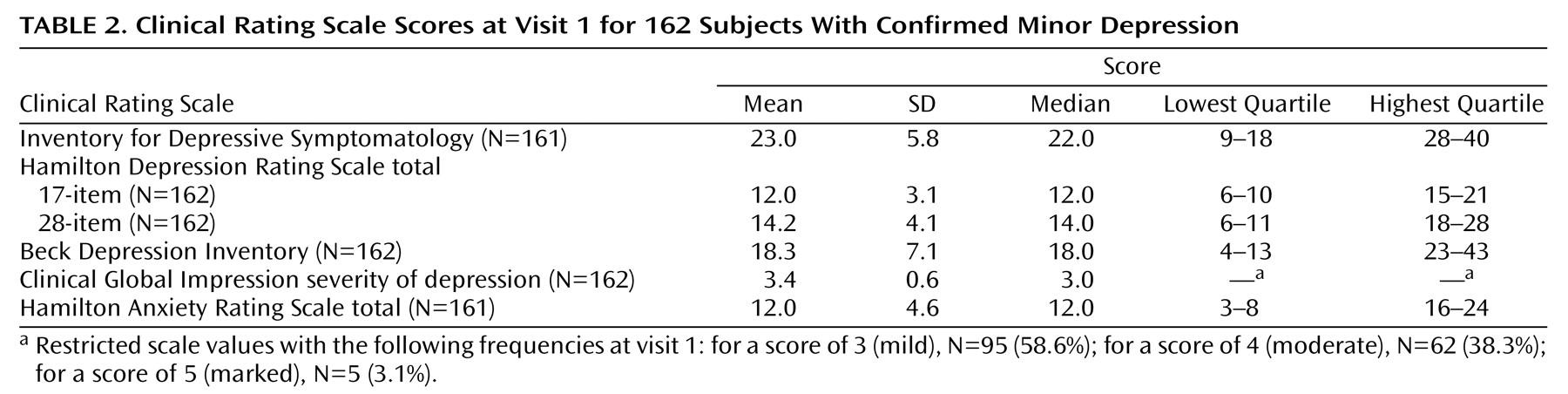
Table 2 demonstrates that baseline clinical ratings for the subjects with confirmed minor depression encompass a broad range of depressive severity, from mild symptoms to moderately severe symptoms, which overlap with scores observed in outpatients with major depressive disorder.
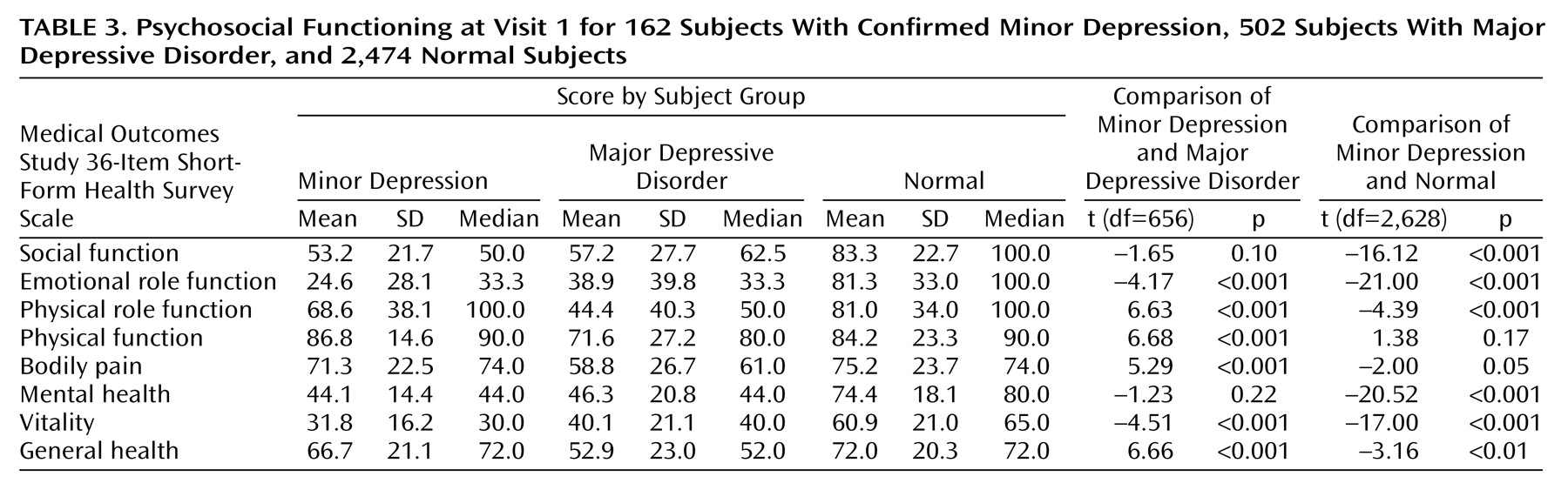
Table 3 presents the scores on the Short-Form Health Survey subscales for our subjects with minor depression, compared with data reported in previous studies of patients with major depressive disorder and normal subjects
(14). Our subjects with minor depression were more impaired than normal subjects on most measures and were at least as impaired as patients with major depressive disorder on many measures.
Seven DIS symptoms were frequently endorsed at the initial evaluation of our study group: feeling sad or depressed nearly every day (an inclusion criterion) (N=179 [79%]), fatigue (N=163 [72%]), trouble thinking or concentrating (N=145 [64%]), sleep disturbance (N=140 [62%]), feelings of worthlessness (N=118 [52%]), loss of interest in things usually enjoyed (N=108 [48%]), and loss of interest in sex and/or other people (N=99 [44%]). Between 60% and 71% of the subjects endorsing those symptoms at entry into the study continued to report them at all of the next four visits, while they were taking placebo (single-blind). By contrast, those symptoms with low rates of initial endorsement—appetite disturbance (16% [N=36]), slow or restless/fidgety (9% [N=20]), and thoughts of death/suicide (9% [N=20])—were highly unstable over the next four visits.
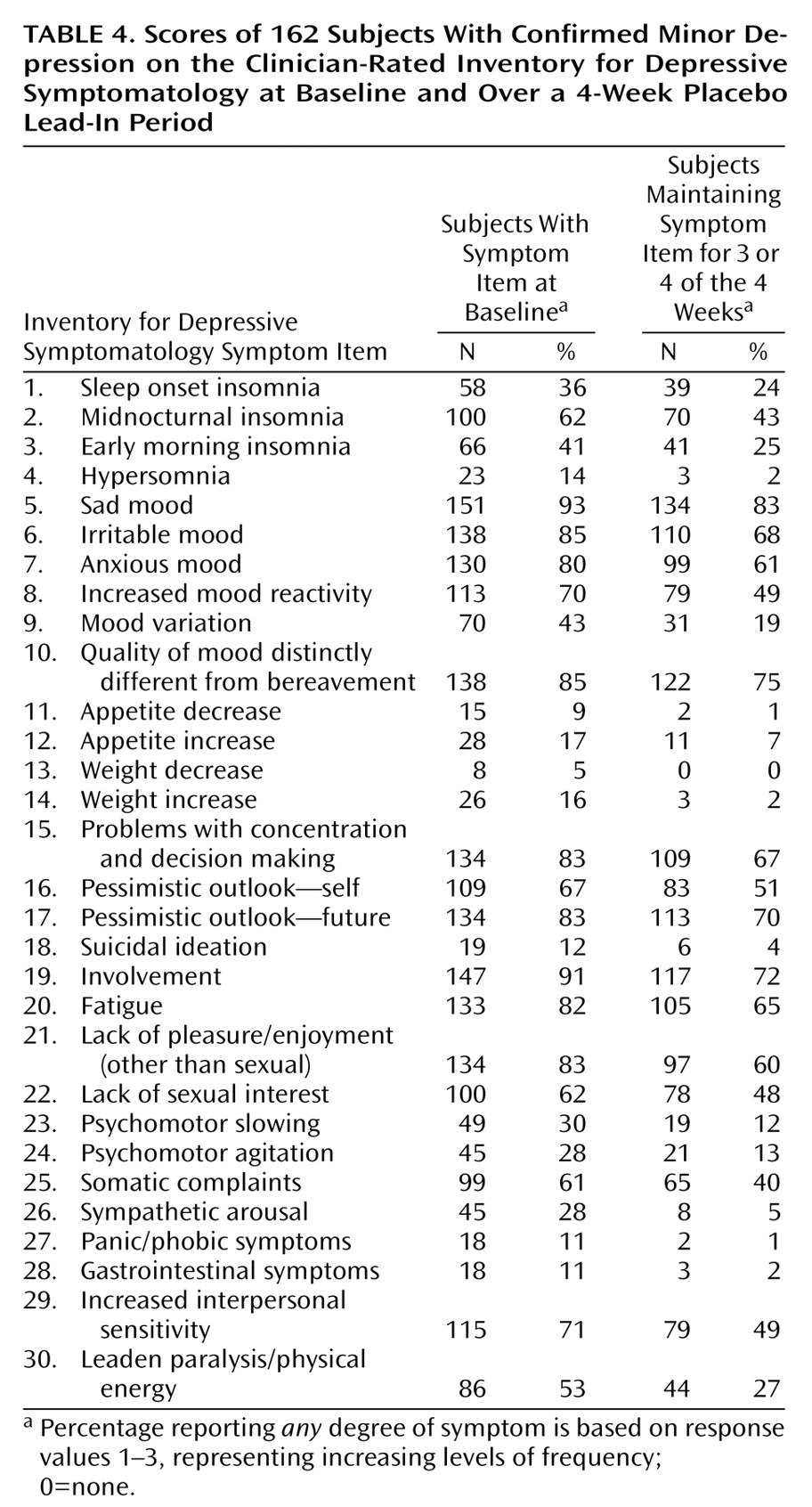
Table 4 reports the frequency of endorsements of individual items of the clinician-rated Inventory for Depressive Symptomatology in our study group. The 11 most frequently endorsed items at the initial visit were sad mood (93%), lack of involvement (91%), quality of mood distinctly different from bereavement (85%), irritable mood (85%), lack of pleasure and enjoyment (an inclusion criterion) (83%), problems concentrating and making decisions (83%), having a pessimistic outlook for the future (83%), fatigue (82%), anxious mood (80%), increased interpersonal sensitivity (71%), and increased mood reactivity (70%).
Table 4 also shows the persistence of symptoms during weekly evaluations, again demonstrating considerable stability among the frequently endorsed symptoms.
Discussion
We believe that the data from this study support four conclusions, each with important implications for the conceptualization and clinical management of minor depression.
First, minor depression with functional disability is not evanescent. The majority of individuals initially meeting our rigorous criteria for minor depression had persistent depressive symptoms and disability throughout a subsequent 4-week period. Of the 226 individuals who met criteria at intake, only five (2.2%) developed major depressive disorder and 14 (6.2%) spontaneously recovered during the 4-week placebo period.
Our second conclusion is that minor depression is characterized by affective and cognitive symptoms: sadness, loss of pleasure/enjoyment, irritable mood, anxious mood, pessimism, difficulty concentrating, lack of involvement, and fatigue. It is distinguished from more severe forms of depression by the infrequent occurrence of the classical neurovegetative and reverse neurovegetative signs and symptoms of depression. In contrast, individuals with minor depression in the ECA database endorsed more of the classic neurovegetative signs of depression. (The ECA is an epidemiological survey and may have included subjects with mild major depressive disorder in the minor depression group.) An additional important finding is that highly endorsed symptoms of depression at the initial interview continued to be endorsed consistently throughout 4 weeks of observation.
Our third conclusion from this study is that minor depression may occur either 1) independently of a history of major depressive disorder, 2) as a less severe but stable episode of major depressive disorder for individuals who have experienced past episodes, or 3) as a transitional state for individuals traversing between euthymia and more severe forms of depression. In our study group of 162 subjects with stable minor depression, 52 (32%) had a history of past major depression, which suggests that it may not be appropriate to use a past history of major depressive disorder as an exclusion criterion for minor depression. In our study, individuals with and without past major depression were nearly identical in age, which argues against the conceptualization of minor depression as simply a stage in the lifetime emergence of major depressive disorder. Patients with and without past major depressive disorder also did not differ in clinical measures of depressive severity or functional disability. Only 2.2% of subjects initially meeting criteria for minor depression in this study went on to develop episodes of major depressive disorder during the next 4 weeks, suggesting that minor depression may be a transitional state for a minority of individuals.
The fourth and broadest conclusion from our study is that minor depression and major depressive disorder should be considered part of a spectrum of severity rather than as two discrete disorders. Several lines of evidence support this conceptualization. First, subjects meeting our rigorous criteria for minor depression over a 4-week period had scores on clinical rating scales for depression indicating a broad spectrum of severity from a mild level to a level approaching the threshold for major depressive disorder. Second, individuals with and without a previous history of major depressive disorder had similar rates of family history of mood disorders, suggesting that minor depression, in some instances, may be part of a spectrum of mood disorders inherited within a family. In our clinical study group, 47 (43%) of the 110 subjects with minor depression who did not have a previous history of major depressive disorder and 27 (52%) of the 52 subjects who did have such a history had a first-degree relative with unipolar mood disorder. This is consistent with findings from epidemiologic studies indicating that the presence of minor depression carries a greater vulnerability for depression in family members, similar to that seen in major depressive disorder
(2,
4,
8,
16). Further support for the spectrum concept of depressive disorders comes from our finding that five out of 226 subjects with minor depression developed major depressive disorder and 14 fell below the threshold for minor depression during a 1-month period. Epidemiologic and clinical studies
(6,
12,
15) clearly demonstrate fluidity among major depressive disorder, minor depression, recurrent brief depression, and depressive symptoms, with many patients traversing a variety of states of severity of depression over time.
There are limitations to this analysis that need to be acknowledged. First, this study group is derived from respondents to advertisements and from clinician referrals for subjects to participate in a pharmacological treatment trial of minor depression. Second, raters were not blind to randomization criteria, creating a potential bias to keep people in the study. Third, our requirement that subjects maintain functional disability throughout the 4-week lead-in phase may mean that we have identified a subset of subjects who are less likely to have an evanescent condition. We believe that substantial dysfunction or disability is a necessary requirement for defining a physical or mental condition that merits treatment. Despite these limitations, we believe that the data presented here provide important information about a group of subjects with nontransient and disabling depressive symptoms.
In conclusion, using a very rigorous set of criteria for minor depression, we have presented evidence that minor depression is stable, is characterized by mood and cognitive symptoms of depression, occurs independently of a previous personal or familial history of major depressive disorder, is disabling, and should be conceptualized as part of the continuum of severity of depressive disorders. This research suggests that we need to evaluate minor depression in other types of clinical settings and investigate the impact that treatment might have on the course of minor depression.