Impaired sleep is a common complaint among people who suffer from posttraumatic stress disorder (PTSD) and has even been referred to as the “hallmark” of PTSD
(1). Even though sleep complaints are prominent features of PTSD, little prospective research has been conducted to assess their natural course after a traumatic event or to determine the ability of early sleep complaints to predict later development of PTSD. The lack of prospective studies on longitudinal changes in sleep pattern after the trauma make it practically impossible to determine the causal relationship between prolonged sleep disturbances and development of PTSD. For example, it was found that the risk of developing new major depression was much higher in subjects who had prior unremitting insomnia
(2). Thus, the main goal of the present study was to further explore the longitudinal course of sleep disturbances in recently traumatized individuals.
Method
The participants in this study were 102 survivors of motor vehicle accidents who were followed up prospectively for 1 year as part of a longitudinal study on the course of PTSD development. The inclusion and exclusion criteria for the study group were described in a previous report
(3). In brief, all subjects were between the ages of 18 and 65 years and had been hospitalized for limb injuries or fractures. The exclusion criteria were head injury or brain damage, loss of consciousness exceeding 10 minutes, and active treatment for psychiatric or sleep disorder at the time of the accident.
A demographically matched comparison group of 19 patients hospitalized in the same orthopedic units for elective surgery was used to control for potential effects on sleep of hospitalization per se.
The overall design and measures in the original study have been described in detail in a previous report
(3). In brief, subjects who consented to participate in the study were given an extensive battery of self-report questionnaires, covering PTSD (DSM-III-R questionnaire
[4], Impact of Event Scale
[5]) and general psychopathology. This battery was repeated 1 week and 1, 3, 6, and 12 months after the accident, when a structured clinical interview (the Structured Clinical Interview for DSM-III-R) was administered to determine DSM-III-R diagnoses of PTSD. Subjective quality of sleep was evaluated by using the Mini Sleep Questionnaire
(6). The questionnaire comprises 10 items tapping both insomnia and excessive daytime sleepiness. Each item is scored on a 7-point Likert scale ranging from 1 (never) to 7 (always), and the total score for each subscale (i.e., insomnia and daytime sleepiness) is defined as the arithmetic sum of the scores for its items.
Results
Of the 102 survivors of motor vehicle accidents, 26 (25.5%) met the diagnostic criteria for PTSD at 12 months, but none of the 19 comparison subjects did.
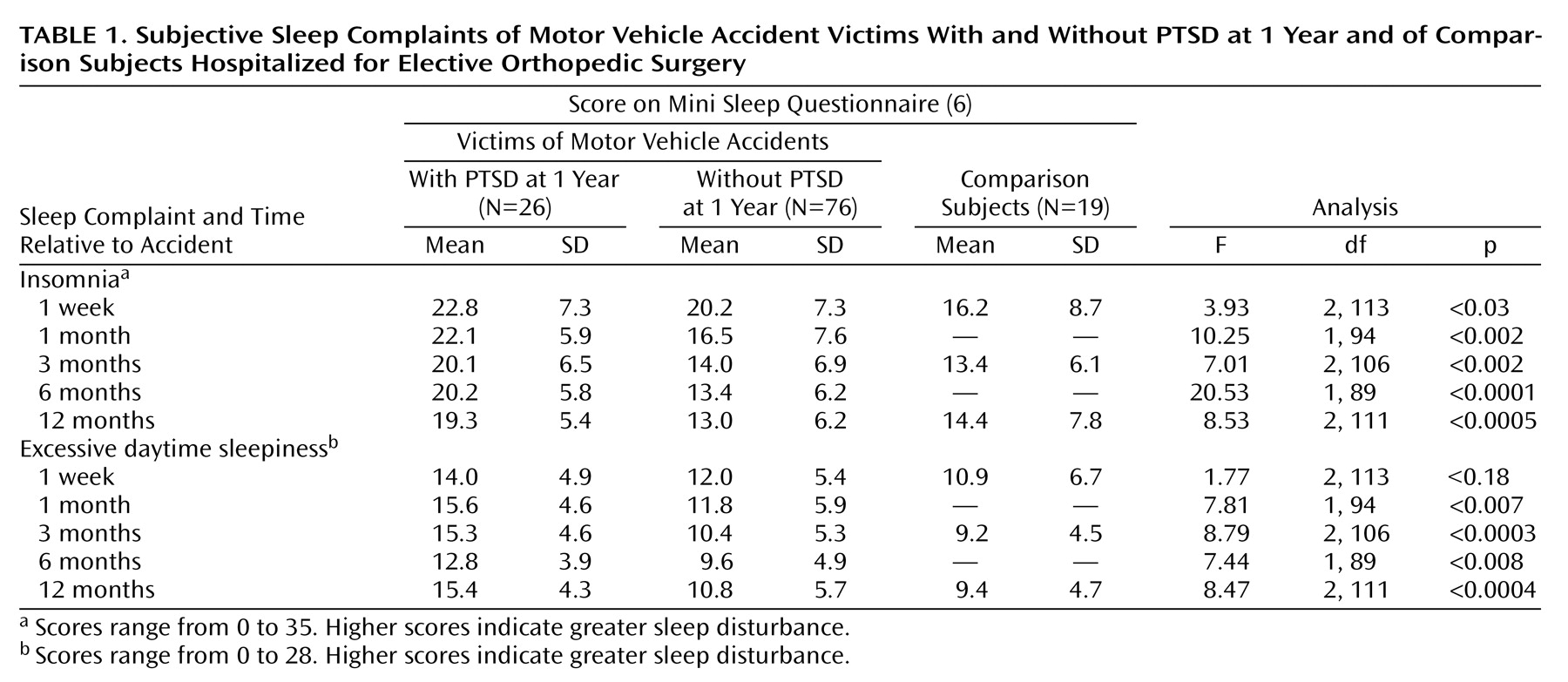
Table 1 presents mean scores on the subscales for self-reported insomnia and excessive daytime sleepiness over time. One week after the trauma, the accident survivors with PTSD had higher scores on both subscales than did the accident survivors without PTSD and the comparison subjects; the difference was significant for insomnia but not for daytime sleepiness. Both accident groups had significantly higher scores on the insomnia subscale than the comparison group, but they did not significantly differ from each other (Tukey’s test, p<0.05). At 1 month the difference between the accident survivors with and without PTSD became significant for both insomnia and excessive daytime sleepiness (F tests, p<0.05). From 3 to 12 months these differences were sustained, and the self-rated sleep quality of the accident group without PTSD improved to the level of the comparison group (Tukey’s test, p<0.05).
A set of repeated measures analyses of variance with all subjects (17 PTSD, 64 non-PTSD, 18 comparison subjects) who had data at 0, 3, and 12 months revealed a significant group-by-time interaction for insomnia (Wilks’s lambda=0.90, F=2.52, df=4, 190, p<0.05) and a nearly significant interaction for excessive daytime sleepiness (Wilks’s lambda=0.91, F=2.41, df=4, 190, p<0.06).
In accordance, significant correlations (r=0.41–0.64, p≤0.001) were found at all time points between the total score on the Mini Sleep Questionnaire and the total scores on the DSM-III-R questionnaire and Impact of Event Scale.
Finally, to assess the usefulness of early sleep complaints in discriminating individuals who developed PTSD 1 year after the accident from those who did not, a set of logistic regression models was used. The logistic regression model for baseline values was not statistically significant (χ2=3.80, df=2, N=108, p=0.15). However, from the 1-month evaluation on they were all highly significant (at 1 month: χ2=15.73, df=2, N=106, p<0.0005; at 3 months: χ2=20.44, df=2, N=101, p<0.0001; at 6 months: χ2=25.10, df=2, N=101, p<0.0001). The fitted values from our logistic regression models show how likely a person is to develop PTSD. At week 1 and at a sensitivity of 90%, this method yielded a poor specificity, 17%. At 1 month and at the same level of sensitivity, the specificity improved to 46%. However, with only a slight reduction in sensitivity (80%) the specificity considerably improved to 65% (68% accuracy). At 3 and 6 months, these levels of specificity improved only slightly (71% accuracy at 6 months).
Discussion
The main finding of the present study is a clear divergence of sleep quality profiles between motor vehicle accident survivors with and without PTSD. Three key features characterize these divergent trends. First, even though most subjects reported sleep difficulties immediately after the accident, the severity was slightly greater in those who developed PTSD. Second, this initial difference appeared to widen over the first 3 months and stabilize over the next 9 months.
With respect to the predictive value of early sleep complaints for PTSD at 1 year, our results showed relatively high sensitivity but only modest specificity for the two domains of sleep complaints. While firm conclusions regarding absolute levels of diagnostic efficiency require cross-validation in an independent group of subjects, these results suggest that on the basis of sleep complaints it is possible to detect subjects who will later develop PTSD as early as 1 month after the trauma. These findings are consistent with our previous findings (3), showing that chronic PTSD can be predicted rather soon after the traumatic event on the basis of early symptoms.
The main limitation of the current study is that sleep disturbances were assessed by using only subjective reports of sleep quality. It is thus impossible to decide whether the current findings reflect a real alteration in sleep quality or a misperception of it. In fact, in another investigation, using data from a subgroup from this study, we failed to detect significant differences between PTSD and non-PTSD subjects in a variety of actigraphic measures of sleep (unpublished data).
The current results do not provide a definite answer to the question of whether persistent sleep disturbances are a risk factor for PTSD or an early manifestation of it. However, they highlight the need to assess whether early treatment of sleep disturbances following a traumatic event reduces the risk for subsequent development of PTSD.