Over the past quarter century, studies have reported racial disparities in the psychopharmacological treatment of schizophrenia
(1,
2). Although the prevalence of schizophrenia seems to be independent of race, its treatment is not
(3,
4).
In preliminary data from the 1980–1982 Epidemiologic Catchment Area program, Robins et al.
(5) reported a similar lifetime prevalence of schizophrenia among African Americans as among other groups, a finding echoed for Hispanic Americans by other researchers
(6,
7). More recently, in a national probability sample of noninstitutionalized 15–54-year-olds, the National Comorbidity Survey
(8) found no mental disorder for which there was a higher prevalence among minorities than among whites. African American patients, however, are more likely to receive a clinical diagnosis of psychosis than are white patients
(9–
11). Neighbors and colleagues have pointed out that diagnostic instruments tend to be formulated among white patient groups, then they are applied to nonwhite populations
(12) without regard to possible cultural differences in the symptom presentations of depression and schizophrenia. African American and white patients may exhibit different symptoms of the same disease, or clinicians may interpret the same symptoms differently in the two races
(13). A recent Department of Veterans Affairs (VA) study
(14) confirmed a lingering problem regarding the diagnostic rates of serious mental illness by race for both Hispanic and African American veterans.
Given a diagnosis of mental illness, differential treatment may ensue, including variability in types of medications prescribed, the amount of medication prescribed, and the amount of provider time devoted to patient visits. As early as 1975, Davidson et al.
(2) reported that African American patients admitted to a teaching hospital were less likely to be given psychotropic drugs than were white patients. Rossiter
(15) reported a similar disparity in the use of prescription drugs affecting the CNS (including agents for the treatment of acute and chronic psychoses) in a nationally representative household survey of 40,000 individuals in 1977. These patterns of treatment change over time. Ten years later, among community-dwelling outpatients in New Haven, Price and colleagues
(16) found that African American men were more likely to be taking depot fluphenazine (49%), more so than African American women (29%), white men (21%), and white women (11%).
Depot medications are long-acting conventional antipsychotic agents that are often given to patients perceived to be less compliant about taking their medications
(17). This might lead to a greater rate of prescription of depot antipsychotics for nonwhite patients. Valenstein et al.
(18), using data from the early to mid-1990s, found that severely ill veterans with psychosis who were taking depot antipsychotics were more likely to be African American.
Lehman and Steinwachs, with the Schizophrenia Patient Outcomes Research Team
(19), found that nonwhite patients with schizophrenia were less likely to be treated in conformance with their guidelines than white patients. They were also given prescriptions for antipsychotic medications more often and antidepressants less often, in spite of appropriate symptoms and diagnosis. Segal et al.
(20) reported that African Americans evaluated in an emergency psychiatric unit generally received more antipsychotics but less provider time; they emphasized the need to establish a relationship with African American patients and to engage them in their evaluation. Hispanic patients with schizophrenia, on the other hand, tended to receive lower doses of antipsychotic medications
(21).
Atypical antipsychotic agents have been the focus of much research into differential treatment by race. Atypical agents are more expensive, but patients using them reported better quality of life
(22). Valenstein et al.
(18) reported that African American veterans in the early 1990s were less likely to receive atypical medications. In 1995, Kuno and Rothbard
(1) found this still to be true in a study of 2,515 Medicaid recipients (the atypical antipsychotics studied were risperidone and clozapine; olanzapine and quetiapine were not yet on the market); more recently, Mark et al.
(23) reported similar findings. Of these last three studies, only Mark et al. analyzed Hispanic patients separately, finding no significant differences in their group of fewer than 70 Hispanic patients.
Specific atypical antipsychotics have unique characteristics that may be more or less appropriate in specific cases. The atypical antipsychotic clozapine is uniquely effective in treating refractory schizophrenia
(24), for example. Olanzapine, on the other hand, was recommended by Tran et al.
(25) in their discussion of atypical antipsychotic agents and African American patients. Olanzapine was associated with a good response and a low incidence of extrapyramidal symptoms, without the risk of agranulocytosis that accompanies clozapine.
Moeller and colleagues
(26) studied the discontinuance of medication among veterans receiving clozapine. Only African American race was significantly associated with discontinuation, possibly related to lower WBC counts among these patients.
The reasons suggested for racial disparity in the treatment of schizophrenia include cultural misunderstanding of the symptoms of nonwhite patients and a failure to develop good patient-provider rapport during brief intake encounters
(27). Clinicians may perceive nonwhite patients as less cooperative and more belligerent, while these patients may feel distrust in a system that is dominated by white providers. On the other hand, research has shown that Hispanic and African American veterans may prefer to use VA outpatient services
(28,
29), making the VA health care system a good place to study this issue.
The purpose of this study was to assess the current state of antipsychotic prescription practices by race in a large national sample of veterans receiving care for schizophrenia in the VA health care system. VA databases offer a unique opportunity to study large samples of patients with specific diagnoses. In addition, the veteran population using VA health care services includes a large proportion of African American and Hispanic individuals. Insufficient income is not a barrier to federally mandated treatment, and access has improved in recent years as a large number of community-based outpatient clinics have been established. This study complements and builds upon that of Kuno and Rothbard
(1), updating the list of atypical medications available while extending exploration of this issue to a large population of veterans with schizophrenia.
Method
Sample
We examined race and the outpatient pharmacy records of veterans with a diagnosis of schizophrenia in fiscal year 1999 (Oct. 1, 1998, through Sept. 30, 1999). The study period was the 12 months after each veteran’s first antipsychotic prescription in fiscal year 1999. The data were from the 1999 and 2000 National VA Psychoses Registries
(30,
31). The registry incorporates outpatient pharmacy data from the VA Pharmacy Benefits Management Group in Hines, Ill. All data were derived from VA administrative databases. Records were merged by means of personal identifiers at the patient level.
Patients were included in the study if they had been diagnosed with schizophrenia, if they were given prescriptions for antipsychotic medication as outpatients in fiscal year 1999 (N=69,787), and if valid data regarding race and age (age ≥18) were available. The sample included 5,955 Hispanic veterans (8.5%), 21,032 African American veterans (30.1%), and 42,800 white veterans (61.3%). There were 3,328 women (4.8%) in the sample. The average age was 52.2 years (SD=12.0, range=19–100).
Measures
The measure of race was obtained from VA national databases; it is described as “observed” race. As such, it provides a fair estimation of race as a proxy for social experiences related to apparent ethnicity. The data had 8.7% missing values. Less than 1% of the veterans were Asian (0.9%) or Native American (0.3%); therefore, these groups were excluded from study analysis. The category “Hispanic black” (0.6%), too small in number to be analyzed separately, was combined with “Hispanic white” (7.9%).
The antipsychotic medications prescribed were either atypical agents (clozapine, olanzapine, quetiapine, and risperidone) or conventional/typical agents (chlorpromazine, fluphenazine, haloperidol, loxapine, mesoridazine, molindone, perphenazine, pimozide, thioridazine, thiothixene, and trifluoperazine). The number of different antipsychotics of all types was summed for each patient.
The diagnosis of schizophrenia was taken from administrative data for outpatient visits and inpatient stays. In cases in which more than one type of psychosis was diagnosed, the one given most frequently was chosen as the primary diagnosis. When a patient with schizophrenia also had another psychosis diagnosed, two indicator variables denoted the additional disorders (bipolar disorder or other psychosis). At least two occasions on which the second psychosis was diagnosed were required to code the indicator as positive. Similarly, a dichotomous variable indicated the presence or absence of a comorbid substance abuse diagnosis.
Analysis
Chi-square analyses assessed associations between categorical variables. Logistic regression analyzed the relationship between race and medication, with control for gender, age, diagnosis of substance use disorders, and bipolar disorder or other psychosis. One analysis modeled receipt of any atypical antipsychotic on these predictors; a second analysis examined all atypical antipsychotics except clozapine. In addition, four separate models analyzed the receipt of olanzapine, risperidone, quetiapine, or clozapine, respectively.
Results
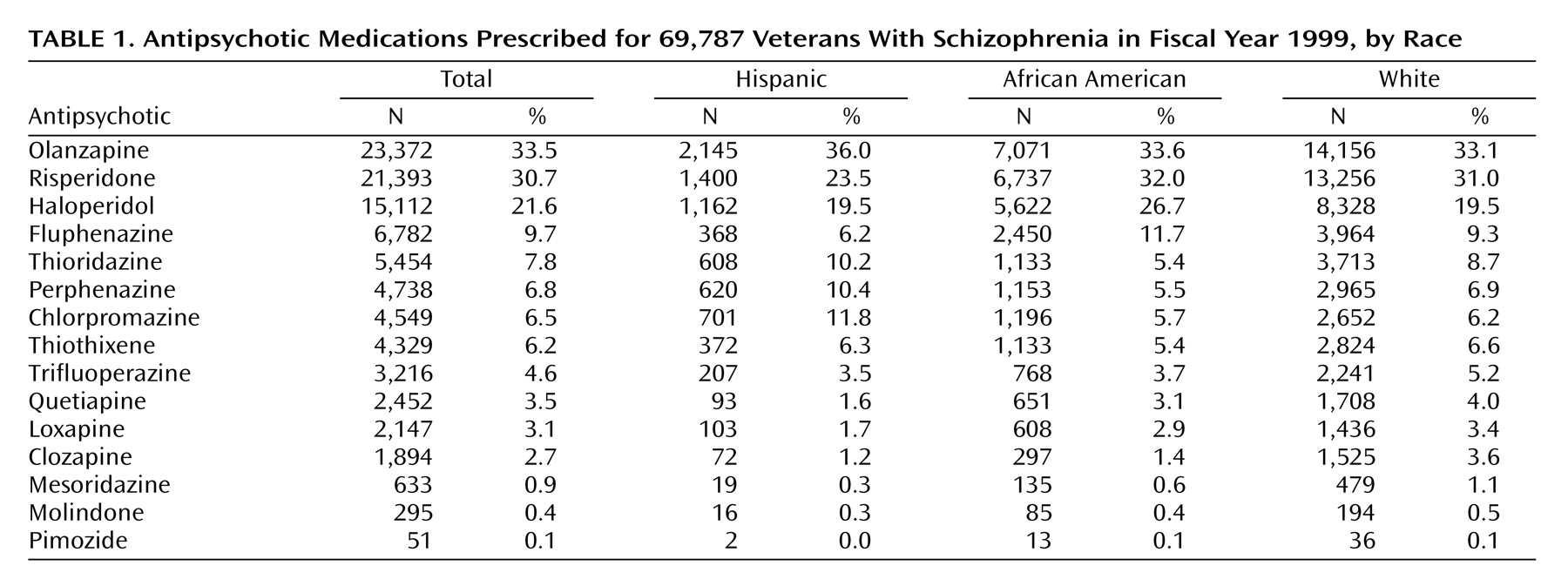
Among 69,787 veterans with schizophrenia and prescription records for antipsychotic medications, 26,000 (37%) had prescriptions for atypical antipsychotics, 27,491 (39%) for conventional antipsychotics, and 16,296 (23%) for both atypical and conventional antipsychotics. The most commonly prescribed antipsychotics were olanzapine (33%), risperidone (31%), and haloperidol (22%). The atypical antipsychotic quetiapine was used by 3.5% and clozapine by 2.7% of the patients (
Table 1). Most of the patients (69%) were taking one antipsychotic during the 12-month period, 24% used two agents, 5% used three, and a handful (1%) were exposed to four to seven different antipsychotics.
Approximately 27% of the patients with schizophrenia had also been diagnosed with substance use or dependence during the study period; 6% had been diagnosed with bipolar disorder in addition to schizophrenia and 7% with other psychosis in addition to schizophrenia. Substance use disorder was more common among African American patients (38%) than among Hispanic (23%) or white patients (22%) (χ2=2001.6; df=2, p<0.0001).
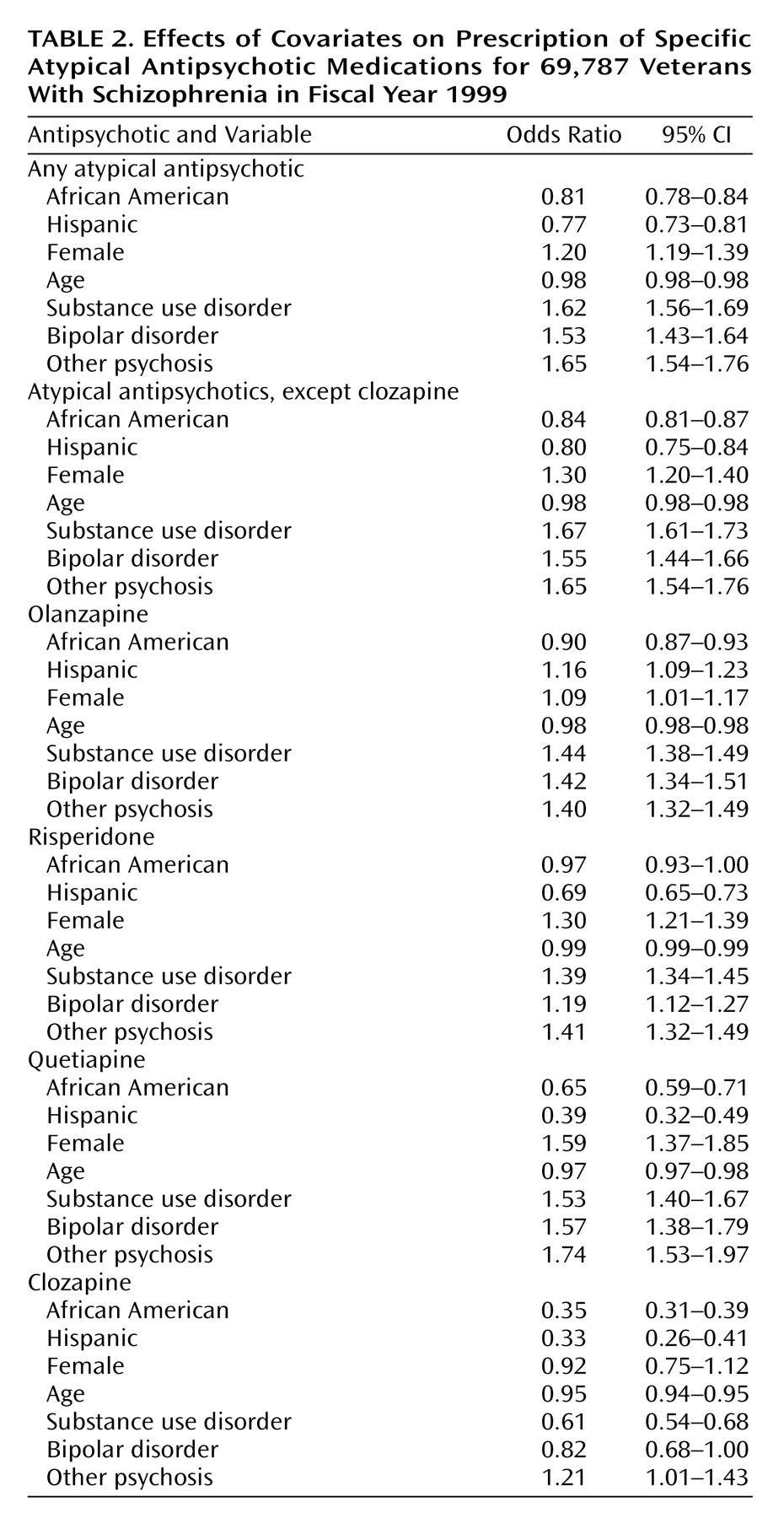
In our multivariate analysis of receipt of any atypical antipsychotic, both Hispanic (odds ratio=0.77, 95% CI [confidence interval]=0.73–0.81; Wald χ
2=86.8, df=1, p<0.0001) and African American (odds ratio=0.81, 95% CI=0.78–0.84; Wald χ
2=132.0, df=1, p<0.0001) patients had somewhat lower odds of receiving an atypical antipsychotic during the year than white patients with schizophrenia. Younger patients, female patients, patients with comorbid substance use disorders, and patients with a comorbid diagnosis of bipolar disorder or other psychosis were more likely to be given prescriptions for atypical agents. For specific results, see
Table 2.
Because of concern that the effect seen for any atypical antipsychotic might have been caused by the large discrepancy regarding clozapine use, we repeated the analysis for receipt of any atypical antipsychotic, omitting the patients taking clozapine. Nonwhite race was still associated with lower odds of treatment with atypical antipsychotics; the odds ratio was 0.84 (95% CI=0.81–0.87; χ2=87.0, df=1 p<0.0001) for African American patients and 0.80 (95% CI=0.75–0.84; χ2=62.5, df=1, p<0.0001) for Hispanic patients, in comparison with white patients.
When examining specific medications, we found diverse results. In the multivariate model, the Hispanic veterans had slightly higher odds of receiving olanzapine (odds ratio=1.16, 95% CI=1.09–1.23; χ2=25.0, df=1, p<0.0001), whereas those who were African American had slightly lower odds (odds ratio=0.90, 95% CI=0.87–0.93; χ2=32.4, df=1, p<0.0001) than the white patients. A diagnosis of substance abuse increased the odds of receiving olanzapine, as did bipolar disorder or other psychosis.
Hispanic patients were less likely to receive risperidone than were white patients (odds ratio=0.69, 95% CI=0.65–0.74; χ2=127.4, df=1, p<0.0001), whereas the odds ratio for African American race was not significantly different from 1 (95% CI=0.93–1.00). The patients with indicators for substance abuse were more likely to receive risperidone than were those without this indicator.
Again, for quetiapine, a marked effect of race was found; both African American (odds ratio=0.65, 95% CI=0.59–0.71; χ2=81.8, df=1, p<0.0001) and Hispanic (odds ratio=0.39, 95% CI=0.32–0.49; χ2=75.0, df=1, p<0.0001) patients were less likely to receive this atypical antipsychotic than white patients. Women were more likely to be given quetiapine. A diagnosis of substance use disorders, bipolar disorder, or other psychosis increased the odds of being given quetiapine.
The results were quite different for clozapine, with adjusted odds ratios well below 0.5 for both minority groups. The veterans who were African American (odds ratio=0.35, 95% CI=0.31–0.39; χ2=266.3, df=1, p<0.0001) or Hispanic (odds ratio=0.33, 95% CI=0.26–0.41; χ2=85.2, df=1, p<0.0001) had a smaller chance of receiving clozapine than the white veterans, as did those with indicators for substance abuse (odds ratio=0.61, 95% CI=0.54–0.68; χ2=70.1, df=1, p<0.0001).
Typical, or conventional, antipsychotic medications also showed significant variations in use by race. For example, the African American veterans were more likely to be given haloperidol (odds ratio=1.53, 95% CI=1.47–1.59; χ2=433.4, df=1, p<0.0001) or fluphenazine (odds ratio=1.21, 95% CI=1.14–1.28; χ2=45.8, df=1, p<0.0001) and less likely to be taking thioridazine (odds ratio=0.70, 95% CI=0.65–0.75; χ2=100.0, df=1, p<0.0001) than the white patients. The Hispanic veterans were less likely to be receiving fluphenazine (odds ratio=0.64, 95% CI=0.58–0.72; χ2=61.1, df=1, p<0.0001) and more likely to be taking thioridazine (odds ratio=1.22, 95% CI=1.11–1.33; χ2=17.5, df=1, p<0.0001) than the white patients.
Discussion
Overall, the African American and Hispanic veterans with schizophrenia were nearly as likely as their white counterparts to receive atypical antipsychotic medications in our multivariate model, as shown by adjusted odds ratios that were somewhat less than 1. Large discrepancies in the use of these medications as a group were not evident. In this respect, the VA is serving these African American and Hispanic clients well, patients who are more likely to use VA mental health services than white patients
(32). In contrast, persistent disparity is apparent in the use of clozapine and quetiapine.
African American and Hispanic veterans are still not given perscriptions for certain atypical medications to treat their schizophrenia with equal frequency, in comparison with white patients. Reasons for this potential disparity need to be determined. One possibility might be patient preference: African American and Hispanic patients may refuse to take newer drugs and may be fearful of being test cases. Another possibility could be concern regarding diabetes. Clozapine and olanzapine are associated with diabetes
(33–
35), and veterans of African American or Hispanic heritage are at greater risk for diabetes than are white Americans
(36,
37). This could explain the disparity in the use of clozapine although not the equivalent use of olanzapine. Some African American and Hispanic veterans in this study may have had a brief exposure to these atypical agents before the study period; if they showed signs of blood glucose elevation or sudden weight gain, their use of atypical antipsychotics might have been discontinued. This might lead to a lower rate of use during the study period.
The Hispanic and African American veterans in this study were less likely to receive clozapine. Clozapine is the first choice for the treatment of refractory cases of schizophrenia
(24) and is singularly effective in treating patients with comorbid substance use disorders
(38,
39). When a patient’s psychosis is treated without treating comorbid substance abuse, the patient is less likely to respond well because a significant part of his or her problem is not being addressed
(40). Under such circumstances, adherence to a regimen of antipsychotic treatment is less likely. Such patients may be given depot medication, although a trial of clozapine might well be more effective. Given the elevated rate of substance use disorders, it is possible that clozapine is being underused among these African American and Hispanic patients. It also seems counterintuitive that patients who were diagnosed with substance use disorders were, independent of race, less likely to be given clozapine.
Concern about weight gain, diabetes, and agranulocytosis may be inhibiting the prescription of clozapine to African American and Hispanic patients. Lawson
(27) noted that the minimal leukocyte count required for treatment with clozapine might exclude African Americans, although they “tend to show a relative and benign leukopenia” (p. 303). That is, the observed leukopenia is not necessarily likely to increase the risk of agranulocytosis. Lawson’s comment suggests the need for research on the relationship between agranulocytosis and leukopenia in African Americans with schizophrenia. Strickland et al.
(41) concluded from their review of race and psychopharmacology that differences in both administration and metabolism/response to psychoactive agents exist and are poorly understood. Certainly, precise hereditary information is needed to study pharmacokinetics properly, as well as details regarding the blood levels achieved and the metabolites produced from treatment with antipsychotic agents. Although it is beyond the scope of this study, these areas include potentially significant factors in determining appropriate use of atypical antipsychotics, warranting further attention and research.
African American and Hispanic veterans with schizophrenia were also less likely to receive the atypical antipsychotic quetiapine, whereas women were more likely to receive this medication. Quetiapine has been in the VA formulary since 1997 and is less expensive than clozapine and olanzapine, costing approximately the same as risperidone
(42). Quetiapine tempers both positive and negative symptoms but does not alter prolactin hormone levels, as do some antipsychotics (so it will not cause breast enlargement or irregular periods), and it is less likely to cause weight gain
(43). It may be these features of the medication that appeal to women. Its lower use among Hispanic and African American patients may reflect slower dissemination of new medications to nonwhite patient populations.
A limitation of this study is that the outpatient pharmacy database we used does not provide a comprehensive record of depot medications, most of which are dispensed through medication clinics. Because approximately 18% of the veterans with schizophrenia are likely to be taking depot medications
(18) and depot drugs are conventional antipsychotics, the proportion of veterans taking typical antipsychotic agents may have been underreported in this sample. There is evidence that veterans diagnosed with schizophrenia may be more likely to receive depot medications if they are African American. To the extent that this is true, the findings in this study regarding race and atypical antipsychotics are biased. The proportion of African Americans taking typical agents should be greater; therefore, the proportion receiving atypical antipsychotics should be even smaller than reported here. Mitigating this possibility is the fact that many patients taking depot medication also receive some oral antipsychotic, usually the same medication. This would cause them to appear in this study among patients taking conventional antipsychotics.
Although overall use of atypical antipsychotics appears to be approaching even distribution among patients of different racial backgrounds, disparity issues persist regarding specific antipsychotic agents among African American and Hispanic patients. Clinical concerns or patient preference may explain some of this disparity, but further research into why there is differential use of these antipsychotic agents is needed. In particular, the differential use of clozapine, an antipsychotic with unique value for refractory and dually diagnosed patients, is troubling.