High rates of clinical depression are found among individuals who engage in HIV risk behaviors
(1). Symptoms of depression are associated with unprotected sexual intercourse, multiple sex partners, trading sex for money or drugs, and contracting sexually transmitted diseases (STD)
(2–
4). Depression may increase the likelihood of engaging in these behaviors to mitigate distress, and depression can compromise motivation to change these behaviors
(5). STD clinic patients are at high risk for HIV
(6) and have high rates of depressive symptoms
(7). We investigated whether depressed patients were more likely to report engaging in HIV risk behaviors than nondepressed patients on admission to an urban STD clinic.
Method
The institutional review boards of Johns Hopkins University of Medicine and the Baltimore City Health Department approved the study. Study participants were men and women who were evaluated at the Baltimore City Health Department STD clinic. Between July 2000 and August 2001, a clinic assistant recruited individuals who were consecutively evaluated by a clinic nurse practitioner. After the study had been described to potential participants, written informed consent was obtained. Using audio computer-assisted self-interview, participants answered questions about sex and drug abuse behaviors (Risk Behavior Assessment
[8]), symptoms of depression (Beck Depression Inventory), and overall health status (General Health Questionnaire
[9]). The utility of the Beck Depression Inventory and General Health Questionnaire were compared in screening for major depressive disorder.
A subset of participants was consecutively recruited each week for evaluation with the nonpatient edition of the Structured Clinical Interview for DSM-IV (SCID). Psychologists trained in SCID administration assessed axis I psychiatric disorders. To distinguish major depressive disorder from transient substance-induced mood disorders, the SCID substance abuse comorbidity module was included. A SCID diagnosis of current major depressive disorder was used as the criterion standard to calibrate Beck Depression Inventory and General Health Questionnaire cutoff scores; separate cutoff scores were calculated for women and men.
Statistical analyses were performed with STATA 7.0 (Stata Corp, College Station, Tex.). To determine a valid estimate of depression for our setting, logit models and receiver operator characteristic curves were used to establish optimum Beck Depression Inventory and General Health Questionnaire cutoff scores for current major depressive disorder. To check for nonlinearity, the probability of engaging in risk behaviors was plotted against Beck Depression Inventory and General Health Questionnaire scores. Logistic regression and linear regression were used to investigate the association between HIV risk behaviors and Beck Depression Inventory and General Health Questionnaire cutoff scores or Beck Depression Inventory scores as a continuous measure. Since substance abuse is known to be associated with both depression and HIV risk behaviors, we adjusted for substance abuse (any occasion of consuming five or more alcoholic drinks and abuse of any drug in the last month) in multivariate models.
Results
Of 795 patients invited to participate, 671 (84%) consented. Male patients (81/401) were more likely than female patients (43/394) to refuse study participation (p<0.01); there were no differences in age or race between those who did or did not consent (p>0.05). Study participants were 351 women and 320 men. Their mean age was 30 years (SD=8.7, range=18–58); 647 (96%) were African American; 494 (74%) were single or never married; 502 (75%) had some high school education or had graduated from high school; and 556 (83%) were heterosexual.
A subset of 99 women and 102 men completed the SCID. For this subset, estimates of current major depressive disorder among the women (N=14 [14%]) and men (N=10 [10%]) were well above general population estimates
(10).
For the entire group, the optimum cutoff score for major depressive disorder on the Beck Depression Inventory was 18 for women (receiver operating characteristic curve=0.75; sensitivity=64.3%; specificity=89.4%) and 9 for men (receiver operating characteristic curve=0.80; sensitivity=70.0%; specificity=78.0%). Beck Depression Inventory cutoff scores classified 50 (14%) of the 351 women and 73 (23%) of the 320 men as being depressed.
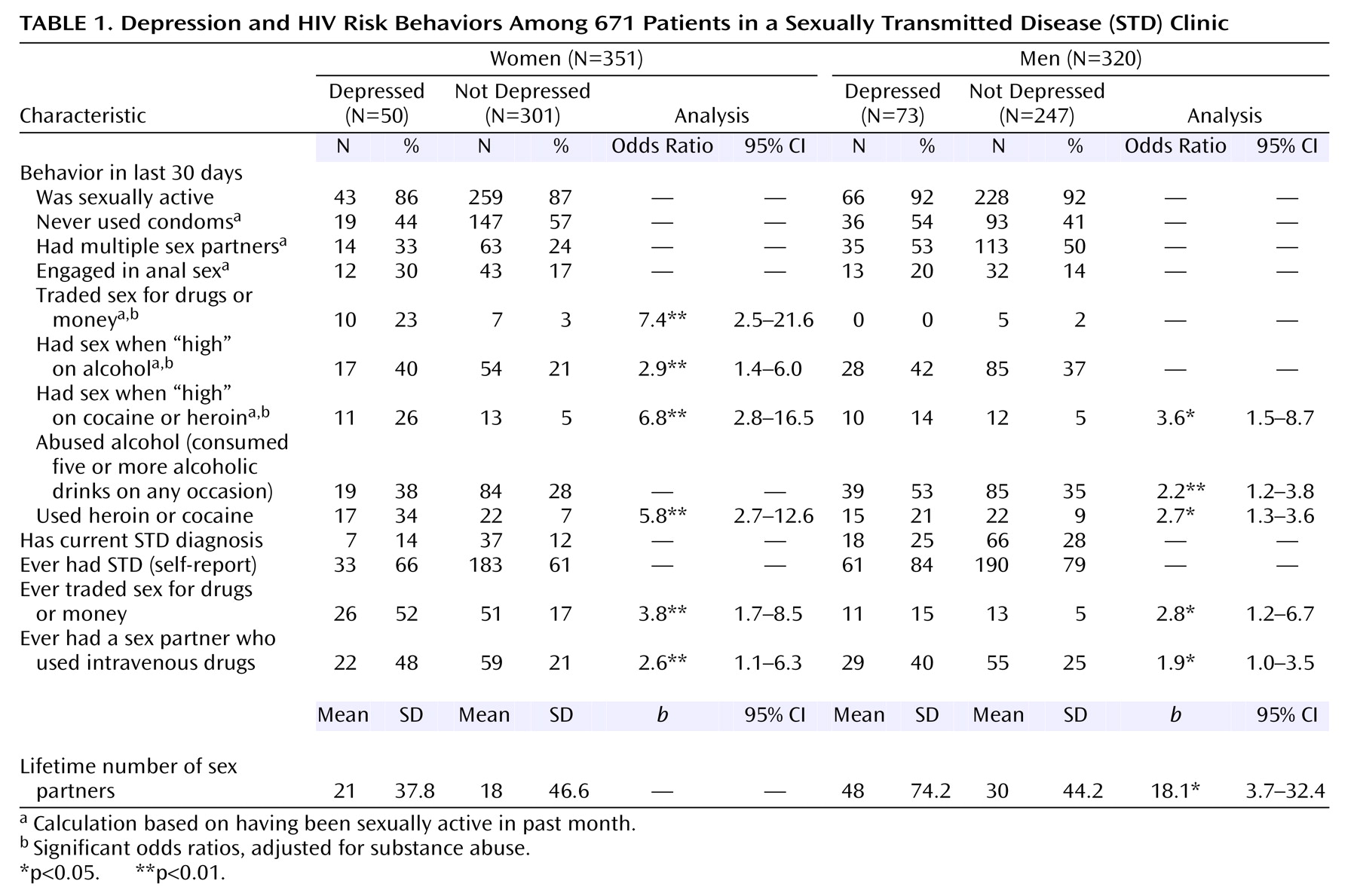
The rate of depression (defined by Beck Depression Inventory cutoff scores) among women and men and the association with HIV risk behaviors are shown in
Table 1. Significant odds ratios were adjusted for substance abuse. In the preceding 30 days, depressed women were much more likely (2.9–7.4 times) than nondepressed women to have traded sex for drugs or money, have had sex when “high” on alcohol, cocaine, or heroin, and have used cocaine or heroin. Depressed women were also much more likely (2.6–3.8 times) than nondepressed women to report a history of trading sex for drugs or money and having had a sex partner who used intravenous drugs. In the preceding 30 days, depressed men were much more likely (2.2–3.6 times) than nondepressed men to have had sex when “high” on cocaine or heroin and to have abused alcohol or drugs. Depressed men were also much more likely (1.9–2.8 times) than nondepressed men to have had a greater number of lifetime sex partners, a history of trading sex for drugs or money, and a history of having had a sex partner who used intravenous drugs. Contrary to expectation, depression was not independently related to unprotected sexual intercourse, multiple sex partners, anal sex, or STD diagnosis. General Health Questionnaire cutoff scores and Beck Depression Inventory scores used as a continuous measure of depression showed the same pattern of associations (data not presented). Scatterplots did not reveal nonlinear associations between depression scores and risk behaviors.
Discussion
Depression found in STD clinic patients was associated with certain HIV risk behaviors. Compared with nondepressed patients, depressed patients were more likely to have sex for money or drugs, have sex when “high” on alcohol or drugs, and to have had a sex partner who used intravenous drugs. Depressed patients were also more likely to have a greater number of lifetime sex partners and to abuse alcohol or drugs. Depression may contribute to the probability of acquiring HIV disease in this high-risk population and could also complicate treatment. Since depression impairs both physical and cognitive functioning, it hinders adherence to treatment and can interfere with the management of most diseases. Moreover, depression is a barrier to behavior change, currently the most successful strategy to effectively reduce the risk of acquiring and spreading HIV.
Contrary to expectation, depression alone was not associated with having unprotected sexual intercourse, multiple sex partners, or an STD diagnosis. The time frames used to measure depressive symptoms (previous week) and risk behaviors (previous month and lifetime) were partially concordant, possibly attenuating the association between depression and some sexual risk behaviors. The Beck Depression Inventory cutoff score of 9 for men identified a higher percentage of them as depressed than the SCID did. This cutoff score may have overestimated the effect of depression, however; the pattern of associations between Beck Depression Inventory and HIV risk behaviors held at higher Beck Depression Inventory cutoff scores and when the Beck Depression Inventory was used as a continuous measure. Furthermore, a score of 10 is the generally accepted threshold for identifying cases of possible depression in samples without a criterion standard assessment. Finally, the study’s cross-sectional design precludes causal interpretation of the association between depression and risk behaviors.
To our knowledge, this is one of the first studies to document an association between depression and HIV risk behaviors among STD clinic patients. Identifying depression and developing strategies to intervene effectively with these patients may reduce HIV risk behaviors, support behavior change, and improve health outcomes.