Awareness of seasonal changes in mood and behavior dates back to ancient times
(1). Seasonal affective disorder, winter type
(2), is characterized by depression in fall or winter, with complete remission or hypomania in spring or summer. Winter seasonal affective disorder is believed to be caused in vulnerable individuals by the shortening of the day, and it responds to light treatment
(3,
4). In contrast, summer-type seasonal affective disorder consists of recurrent depression in summer and remission of depressive symptoms in fall and winter; it may be caused by exposure to heat and may improve with manipulations of temperature
(5,
6).
The degree to which the change of season influences mood, energy, sleep, appetite, food preference, and the wish to socialize has been called “seasonality”
(7). To study seasonality in the community, the Seasonal Pattern Assessment Questionnaire was designed by Rosenthal et al.
(8). The Seasonal Pattern Assessment Questionnaire was first used by Kasper et al.
(7), who described a less severe but more prevalent form of seasonal affective disorder called subsyndromal seasonal affective disorder. The Seasonal Pattern Assessment Questionnaire does not diagnose seasonal affective disorder but estimates the frequency and pattern (i.e., winter or summer) of seasonal affective disorder and subsyndromal seasonal affective disorder, generally overestimating seasonal affective disorder when compared to assessment by clinical diagnostic interview
(9). The Seasonal Pattern Assessment Questionnaire also estimates the average seasonality through calculation of a global seasonality score.
Since the initial study of Kasper et al.
(7) in a suburban area of Washington, D.C. (Montgomery County, Md.), the Seasonal Pattern Assessment Questionnaire has been used in diverse geographic areas and populations, for example, in North America
(10–
16), Europe
(17–
22), and Asia
(23–
25). Studies of largely Caucasian groups in temperate climates found a clearly more prevalent winter pattern of seasonal affective disorder than summer seasonal affective disorder
(7,
10,
11,
17,
21). In contrast, three studies performed at similar latitudes in Asia
(23–
25) found that summer seasonal affective disorder was more prevalent than winter seasonal affective disorder.
Method
This cross-sectional survey was conducted on a convenience group of undergraduate and graduate African American college students from four colleges and universities in Washington, D.C. The study was approved by the institutional review board of the Department of Mental Health of the District of Columbia. We administered the Seasonal Pattern Assessment Questionnaire in person in a classroom setting; it was previously reported to have a high degree of test-retest reliability in college students
(16). A standard introduction was read, explaining that we intended to study the degree to which mood, energy levels, sleep, and appetite vary with seasons and environmental factors that may be associated with seasonality and that there were numerous prior similar studies performed in the general population and other ethnic groups but not among African American students. The students were told that they could leave blank the spaces that they did not want or did not know how to answer, that their individual answers would be kept confidential, and that their participation was voluntary and would not influence their performance evaluation. After we fully answered the students’ questions, written informed consent was obtained.
To be included in the study, each subject must have identified himself or herself as an African American and must have lived in the study area (latitude 35° north to 45° north) for at least 3 years. There were two separate questionnaire collection intervals: once in the fall (from October to December) and again in the spring (from March to May). To minimize the possibility that different Seasonal Pattern Assessment Questionnaire scores resulting from the questionnaires being completed in different seasons might influence the results, we chose to divide the subjects into two groups according to their birth date. It was determined by chance that students who were born in the first 15 days of any month would be studied in the spring while the others would be studied in the fall.
A global seasonality score was calculated according to Kasper et al.
(7). The Seasonal Pattern Assessment Questionnaire criteria used by Magnusson and Stefansson
(17) were employed to define the summer and winter patterns of seasonal affective disorder and subsyndromal seasonal affective disorder. Three components contribute to the diagnosis of seasonal affective disorder with the Seasonal Pattern Assessment Questionnaire: the global seasonality score, the “problem” rating, and the month in which a subject reports feeling the worst. For a diagnosis of winter seasonal affective disorder, a subject must meet the following criteria: 1) a global seasonality score of 11 or higher; 2) a “problem” rating with seasonal mood changes to at least a moderate degree (2 and above); 3) feeling worst in December and/or January and/or February with any other combination of months except June, July, and August. For the diagnosis of summer seasonal affective disorder, a subject must, in addition to criteria 1 and 2 already mentioned, feel worst in June and/or July and/or August with any other combination of months except December, January, and February. To be categorized as having subsyndromal seasonal affective disorder, the subjects would have to either have a global seasonality score of 11 or more with a “problem” rating of not more than mild (0 or 1), or have a global seasonality score of 9 or 10 with a problem rating of at least mild (1 or above). Identical specifiers for the winter and summer varieties of seasonal affective disorder also apply for subsyndromal seasonal affective disorder.
We used two multinomial probability distribution tests
(33) to compare the winter versus summer frequency of seasonal affective disorder and total seasonal affective disorder (seasonal affective disorder plus subsyndromal seasonal affective disorder)
(7,
11). The level of statistical significance was set at z>1.96 (p<0.05). Simple correlations were used for the association of age with global seasonality score.
We also tested the effects of gender and “having heard of seasonal affective disorder” (“awareness”) by using a two-way analysis of variance (ANOVA), with global seasonality score as a dependent variable. The level of statistical significance was set at p=0.05.
Results
Demographic Characteristics
Of 646 students from whom we received informed consent, 597 returned their questionnaires. The response rate was 92.4%. Of these, only 537 (83.1%) completely filled in all three components (global seasonality score, severity of dysfunction, and month of the year when feeling the worst) needed to generate a diagnosis of winter or summer seasonal affective disorder/subsyndromal seasonal affective disorder. A majority of the subjects (N=435, 81.0%) did not meet the criteria from the Seasonal Pattern Assessment Questionnaire for seasonal affective disorder, syndromal or subsyndromal. We used all available information, including information from subjects with partially missing data. Thus, for the analysis of global seasonality score, we had 546 subjects who responded (response rate=85%).
Of the 597 participants, 591 (99%) responded to the question regarding gender. A total of 382 (64.6%) were women, and 209 (35.4%) were men. Only 581 subjects (97.3%) responded to the question regarding their age. The average age was 29.5 years (SD=10, range=16–67). The average duration of residence in the study area (latitude 35° north to 45° north) was 19.3 years (SD=12.5). Age and average duration of residence did not differ significantly between the men and the women.
Of 559 subjects who responded to the question “Have you ever heard of seasonal affective disorder?” 445 (80%) answered “no,” and 114 (20%) answered “yes.”
Hypothesis Testing
As hypothesized, the frequency of winter seasonal affective disorder was significantly higher than that of summer seasonal affective disorder (5.4% versus 0.6%) (z=4.63, p<0.001). The frequency of total winter seasonal affective disorder (syndromal plus subsyndromal) was significantly higher than the total for summer seasonal affective disorder (14.9% versus 4.1%) (z=5.93, p<0.001).
Pearson’s correlation of age with global seasonality score was 0.03 (N=546, p<0.47).
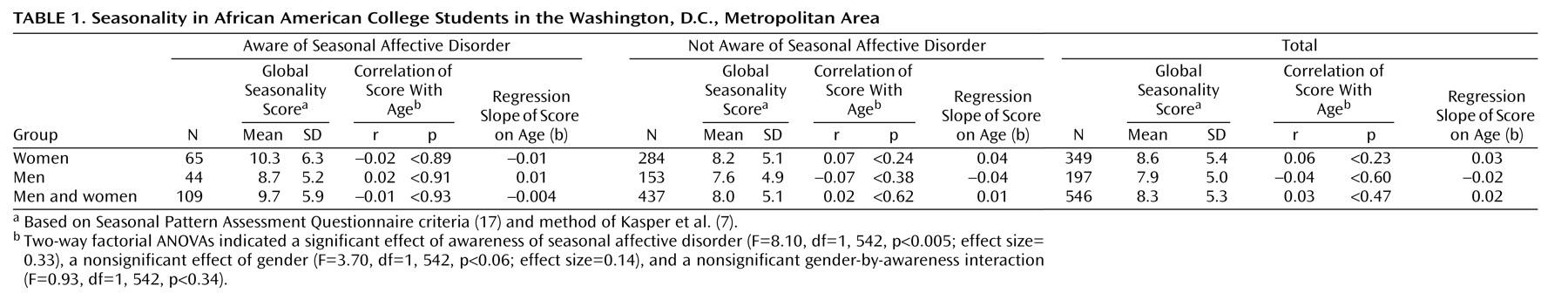
Table 1 shows the correlations for other subgroups as well. Hypothesized negative correlations between age and global seasonality score did not emerge.
For the two-way factorial ANOVA with global seasonality score as the dependent variable and gender and awareness as the two factors, the interaction of gender and awareness was not significant (F=0.93, df=1, 542, p<0.34), but gender was significant (F=3.70, df=1, 542, p<0.06). The mean global seasonality score for women was 8.6, and for men, it was 7.9, with a small gender effect size (0.14). In addition, it is instructive to note that since the global seasonality score did not pass several tests of statistical normality and transformation was not successful in reducing skewness, a nonparametric test was used to report a more realistic gender p value. The Mann-Whitney test’s p value for gender was 0.18 (Mann-Whitney z=1.34, p<0.18). The difference in p value between the parametric ANOVA (gender F=3.70, df=1, 542, p<0.06; effect size=0.14) and the nonparametric Mann-Whitney p value of 0.18 illustrates the effect on the p value of nonnormality and skewness for p values near the classic 0.05 level.
The effect of awareness was significant (F=8.10, df=1, 542, p<0.005), and students who had prior knowledge of seasonal affective disorder (N=109, mean global seasonality score=9.7) had a higher global seasonality score by 1.7 points (effect size=0.33) than those without prior knowledge of seasonal affective disorder (N=437, mean global seasonality score=8.0). The nonparametric p for awareness (Mann-Whitney z=2.88, p<0.004) was 0.004, illustrating the robustness of the 0.005 parametric p (F=8.10, df=1, 542, p<0.005)
Discussion
To our knowledge, this is the first study of the seasonal variation of mood and behavior in African Americans, the study with the largest number of black subjects, and the largest American study of seasonality in college students completed to date. Winter seasonal affective disorder was more prevalent than summer seasonal affective disorder. (We would like to reemphasize, however, that the Seasonal Pattern Assessment Questionnaire, which we used to indicate a history of seasonal affective disorder, is an epidemiological rather than a clinical tool and does not diagnose seasonal affective disorder.)
A higher frequency of winter seasonal affective disorder is consistent with previous reports in the general population at a similar latitude
(7) and other previous studies in general populations with mostly Caucasian subjects
(2,
13,
17,
21). Given the limitations of our study, we recommend caution in interpreting our results. We did not compare seasonality in African American students with a contemporaneous student comparison group, and we will remedy this limitation in future work. In addition, we lacked information on the subjects’ socioeconomic status, a major confounding of ethnicity. Other limitations include uncertainty regarding the validity of the Seasonal Pattern Assessment Questionnaire among African American students and convenience, rather than random, sampling.
Several epidemiological studies using the Seasonal Pattern Assessment Questionnaire in predominantly Caucasian populations did not focus on summer seasonal affective disorder
(13,
20,
34,
35). The only two previous American studies of seasonality in college students also omitted reporting on the summer pattern
(15,
16). Relevant for a decreased interest in summer seasonal affective disorder versus winter seasonal affective disorder, a review of epidemiological surveys of seasonality
(36) equates seasonal affective disorder with its winter subtype. Nevertheless, Morrissey et al.
(37) reported a more prevalent summer than winter pattern of seasonal affective disorder in the general population in a tropical climate in Northern Australia. The authors attributed this increased frequency to a combination of temperature, humidity, and air movement, which exceeds a cutoff point for climatic discomfort. It is thus of particular importance that in our study, as in Kasper et al.
(7), a higher frequency of winter seasonal affective disorder than summer seasonal affective disorder resulted from a survey that took place in a metropolitan area in which summer weather is uncomfortably hot and humid.
Moreover, three studies using the Seasonal Pattern Assessment Questionnaire performed in Asia—one of Japanese civil servants
(23) and two other recent studies of Chinese students
(24,
25)—found summer seasonal affective disorder to be more prevalent than winter seasonal affective disorder. Because the summer pattern of seasonal affective disorder is more prevalent in the Asian population, the largest one in the world
(38), and given current concerns regarding global warming, we expect an increase in interest in studying vulnerability for heat-related depression, including summer seasonal affective disorder.
The 95% confidence intervals (CIs) of the frequency of seasonal affective disorder in the current study (3.39–7.94 for winter seasonal affective disorder and 0.06–1.76 for summer seasonal affective disorder) were similar to those reported in the previous study of Montgomery County, Md., (2%–6% for winter seasonal affective disorder and 0%–0.2% for summer seasonal affective disorder). It is important, however, to exercise caution in comparing seasonality results in students versus the general population. Although studying seasonality in college students
(15,
16,
24,
25) has advantages in terms of some degree of homogeneity in lifestyle, it also has disadvantages. A possible confounding effect of the academic calendar might artificially augment seasonality. Moreover, the stress of final examinations in late spring may also mask a winter pattern of seasonality. Unfortunately, to our knowledge, no study of Western college students has ever been performed at our latitude.
In college students in Maine, at markedly higher latitude, Low and Fleissner
(15) found higher frequency rates for seasonal affective disorder and total seasonal affective disorder (seasonal affective disorder plus subsyndromal seasonal affective disorder) of 13.2% and 32.9%, respectively. These rates are higher than those previously reported in the general population
(11). The authors did not mention the ethnic composition of their study group and only reported on the winter type of seasonal affective disorder. Rohan and Sigmon
(16), in another study in Maine, reported that the frequency of seasonal affective disorder was lower but that the magnitude of the global seasonality score was higher than projected based on adult noncollege subjects residing in states between latitude 45° north and 50° north
(11). Rohan and Sigmon argued that even after taking into consideration academic stress, the seasonality effects were strong. In their study, Caucasian students represented 90% of the total group (N=251), with African American, Asian, Hispanic, and Native American students included together as “other” (10%). No analysis of the effect of ethnicity on global seasonality score or the frequency of summer seasonal affective disorder was reported.
Our results are similar to those of previous studies in college students in Maine
(16) and China
(25) that did not find a negative correlation between global seasonality score and age, as initially reported by Kasper et al.
(7) and confirmed in subsequent studies
(11,
13,
17,
18,
20,
21,
34). Swedo et al.
(14) reported a positive rather than negative relationship between age and seasonality in high school students, suggesting that younger age may reverse a negative relationship between age and seasonality. However, in our study group, because we had a relatively older group of college students and a relatively broad distribution of age (we had a large number of nontraditional students participating), the consideration of a too-narrow age distribution or a too-young age for seasonality to fully manifest itself would not apply. Additional work is required to evaluate the relationship between gender and seasonality in African Americans. Our data showed a less-than-significant association for a higher global seasonality score in female subjects (
Table 1).
Having previously heard of seasonal affective disorder predicted a higher seasonality score, consistent with the previous study in Montgomery County
(7). It is possible that having seasonal depression would increase knowledge about seasonal affective disorder or, alternatively, having prior knowledge of seasonal affective disorder might increase the reporting of seasonal difficulties.
The frequency of African American students in Washington, D.C., who were aware of seasonal affective disorder was 109 of 546 (20.0%, 95% CI=16.7%–23.6%), and for those who were not aware of seasonal affective disorder, it was 437 of 546 (80.0%, 95% CI=76.4%–83.3%). The rate of awareness of seasonal affective disorder in our group was approximately 50% lower than in the study performed in Montgomery County more than 10 years ago
(7). In that study, 170 of 416 subjects (40.9%, 95% CI=36.1%–45.8%) were aware and 246 of 416 (59.1%, 95% CI=54.2%–63.9%) were not aware of seasonal affective disorder. In our group, the smaller percentage of subjects with prior knowledge of seasonal affective disorder (20.0% versus 40.9%) (p<0.00001, Fisher’s exact test) may have lowered the occurrence of seasonal affective disorder. Our results raise the possibility that insufficient education about seasonal affective disorder is contributing to a sizable number of African Americans with seasonal affective disorder to be unaware of their condition and, therefore, to be less likely to seek professional help. Also, a lower awareness of seasonal affective disorder might have reduced the reporting of seasonal difficulties in the current study, thus, spuriously reducing the rate of seasonal affective disorder. Thus, since our results should be considered preliminary, we are planning epidemiological and clinical follow-up studies. If a low awareness of the existence of seasonal affective disorder is replicated, it will become imperative to educate the African American community about seasonal affective disorder because winter depression responds to light treatment
(3,
4), a low-cost and low-risk intervention
(39). Specifically for students with winter seasonal affective disorder, light treatment could reduce lethargy, decrease sleepiness, and improve concentration, resulting in improved academic performance.