Schizophrenia is a complex disorder with a genetic contribution, variable psychopathological expression, and neurocognitive impairment. The view that dopamine plays a role in schizophrenia is long-standing, although the hypothesis of hyperdopaminergia to explain psychotic symptoms seems too simplistic
(1).
Recently, electrophysiological, animal, and neuroimaging studies have pointed out that dopamine levels could enhance prefrontal cortex function
(2). These data suggest that many of the cognitive impairments detected in schizophrenia patients could be related to reduced dopamine activity in this area.
The COMT gene codes for the enzyme catechol
O-methyltransferase, which plays an important role in the degradative pathways of catecholaminergic neurotransmitters. The COMT gene, mapped to chromosome 22q11, contains a functional polymorphism (
Val158Met) that consists of a transition at codon 158 of the gene that results in two common variants of the enzyme (
Val and
Met) corresponding to high and low activity, respectively
(3).
It has been claimed that the variability of this gene could constitute a risk factor for schizophrenia. However, family-based association studies and case-control studies have produced a large but inconsistent bulk of results
(4).
Egan and colleagues
(5) examined the COMT
Val158Met polymorphism in relation to brain physiology and cognitive function. They reported an association between the low-activity allele of the COMT gene (
Met) and better performance on the Wisconsin Card Sorting Test (fewer number of perseverative errors)
(6) in schizophrenia patients, their unaffected siblings, and healthy comparison subjects. According to these results, the high levels of dopamine in individuals with the
Met/Met genotype enhance prefrontal function.
Recently, these results have been replicated in healthy individuals
(7) and schizophrenia patients
(8).
Our aims were 1) to investigate the association between COMT genotype and performance on the Wisconsin Card Sorting Test in a sample of sibling pairs discordant for schizophrenia spectrum disorders and 2) to explore the genetic association between the COMT gene and schizophrenia.
Method
The subjects participating in the study were 356 individuals from 89 nuclear families, which consisted of 89 patients affected by DSM-IV schizophrenia spectrum disorders and their fathers, mothers, and healthy siblings (sample described elsewhere
[9]). Written informed consent was obtained from all participants.
The categorical breakdown of patient diagnoses was as follows: schizophrenia (53.9%, N=48), psychotic mood disorder (15.7%, N=14), schizoaffective disorder (12.4%, N=11), schizophreniform disorder (9%, N=8), brief psychotic disorder (5.6%, N=5), delusional disorder (2.2%, N=2), and atypical psychosis (1.1%, N=1). They were receiving antipsychotic drugs, mostly atypical antipsychotics (69.7%)
Schizophrenia patients and their healthy siblings were assessed with the Wisconsin Card Sorting Test. The number of perseverative errors was the index used because it seems to best reflect prefrontal function. All patients were assessed after clinical stabilization.
COMT
Val158Met genotypes were analyzed as described by Daniels and colleagues
(10).
The effect of COMT genotype on Wisconsin Card Sorting Test performance was analyzed for each group separately (patients and healthy siblings) by using analysis of variance (ANOVA) and multiple regression. The multiple regression analysis was conducted to examine the association between the prefrontal function reflected in the Wisconsin Card Sorting Test and the number of Met alleles. All the associations were adjusted for possible confounding factors such as age, sex, and educational level.
The linkage of COMT alleles on risk to psychiatric phenotype was analyzed in a family-based association study using the transmission disequilibrium test
(11).
Results
The genotype frequencies of the high-activity homozygote (Val/Val), heterozygote (Val/Met), and low-activity homozygote (Met/Met) in patients and in healthy siblings was not statistically different (χ2=0.77, df=2, p=0.86). No significant differences were observed between the type of treatment that patients were receiving and COMT genotype (χ2=2.1, df=2, p=0.30).
As expected, patients showed a higher number of perseverative errors on the Wisconsin Card Sorting Test compared with their unaffected siblings (t=3.2, df=88, p=0.001). No significant difference was found in perseverative errors on the Wisconsin Card Sorting Test between patients receiving atypical and typical antipsychotics (F=1.3, df=1, 84, p=0.30).
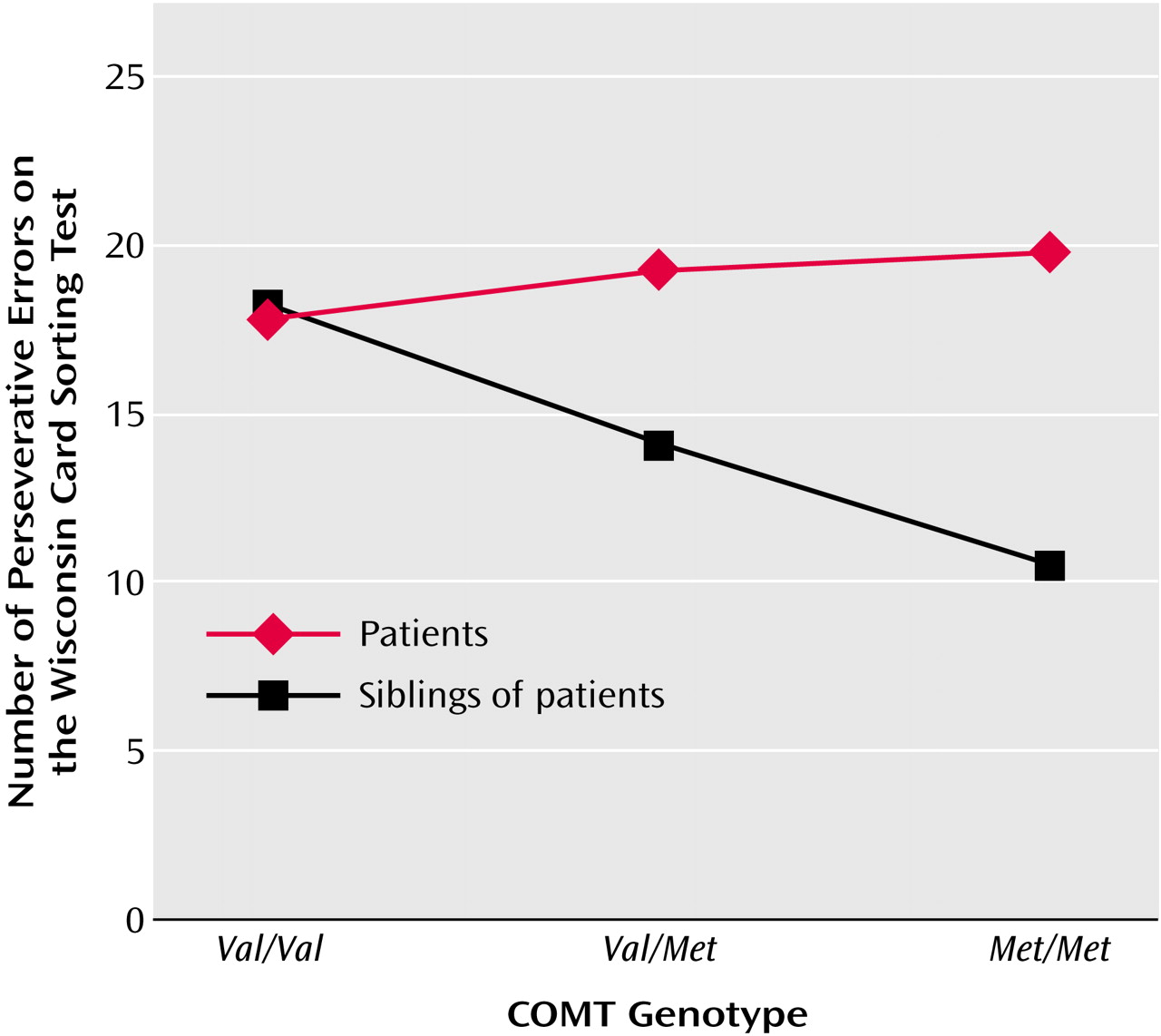
In the group of patients with psychosis, the ANOVA did not detect a significant effect of genotype on the number of perseverative errors (F=0.9, df=2, 84, p=0.40) (
Figure 1). These findings remained essentially unchanged when the analysis was restricted to the subgroup of patients that met DSM-IV criteria for schizophrenia and schizoaffective disorder (N=67) (F=0.37, df=2, 63, p=0.70).
In the healthy siblings, individuals with the
Val/Val genotype made more Wisconsin Card Sorting Test perseverative errors than those with other genotypes (F=5.5, df=2, 75, p=0.007) (
Figure 1). Using multiple regression, the number of
Met alleles was related to the number of perseverative errors (β=4.4, p=0.005). Furthermore, there was evidence of monotonic linear decrease in the number of perseverative errors with higher number of Methionine alleles (β
0Met=8.4, β
1Met=3.2, β
2Met=1.0).
In the 89 families, the transmission disequilibrium test did not show a preferential transmission of alleles from the heterozygous parents to the affected and nonaffected siblings (allele-wise transmission disequilibrium test for patients: χ2=1.5, p=0.20; allele-wise transmission disequilibrium test for healthy siblings: χ2=0.5, p=0.40).
Discussion
Our results do not seem to support the role of the Val158Met polymorphism in the risk for schizophrenia spectrum disorders.
Concerning the analysis of the association between performance on the Wisconsin Card Sorting Test and the functional polymorphism
Val158Met in the COMT gene, our results confirm an effect of COMT
Val158Met genotype on prefrontal cortical function in healthy siblings. These findings are consistent with previous studies conducted in healthy individuals
(5,
7). The strong association between the COMT genotype and the neuropsychological test of executive function (Wisconsin Card Sorting Test) was detected in an allele dosage fashion. This linear trend is consistent with the fact that heterozygous individuals (
Val/Met) have an enzyme activity that is midway between homozygote
(
Val/Val) individuals, who display high COMT activity, and
Met/Met individuals, who have four to five times lower COMT activity
(3). However, in the group of patients we failed to find an association between COMT genotype and perseverative errors on the Wisconsin Card Sorting Test, unlike previous studies
(6,
8). One possible explanation could be that other dopaminergic alterations could mask the COMT effect that we have studied. Several lines of evidence suggest that dopamine innervation of the prefrontal cortex may be abnormal in psychosis
(12). In this sense, a decreased density/hyposensitivity or blockage of some dopamine receptors in the prefrontal cortex could also be responsible for the deficits in the cognitive tasks.
A possible confounding factor in the interpretation of these results is the heterogeneity of diagnoses in our sample, which included several schizophrenia spectrum disorders. However, the analyses with a more homogenous sample of patients (schizophrenia and schizoaffective diagnosis) revealed the same pattern described in the larger sample of patients.
On the other hand, according to our analyses, the lack of association is unlikely to be due to the type of medication that patients received.
Further studies are necessary in order to clarify the specific risk of this polymorphism in the etiology or pathophysiology of schizophrenia and in the cognitive deficits described in these patients.