The stress of combat is notoriously pathogenic. Soldiers are at risk for both short- and long-term psychopathology. Acute combat stress reaction, previously termed battle shock or battle fatigue, encompasses an array of reversible psychiatric and somatic symptoms and impaired functioning. Although persons with combat stress reaction may recover, combat stress reaction often crystallizes into chronic posttraumatic stress disorder (PTSD) and places casualties at risk for chronic PTSD
(1).
The development of PTSD is often an evolving process and extends over time through a series of stages ranging from relatively contained distress to severe disability. In its acute phase, combat stress reaction entails considerable distress and shame, yet its damage is limited to military functioning. In its chronic phase, PTSD may be likened to cancer; it metastasizes and is associated with higher rates of psychiatric and somatic comorbidities, substance abuse, impaired functioning, and higher mortality risk
(2).
As the disease evolves over time, pathological changes and debilitating comorbidity may become fixed and irreversible. Therefore, the aim in addressing the disorder is to push back the intervention to emphasize preventive rather than curative medicine. Prevention means thwarting the development of the disorder and/or taking measures to halt or slow its progress. The acute phase of combat stress reaction is often seen as a window of opportunity. Since World War I, many armies have adopted frontline treatment as the preferred intervention for combat stress reaction. This treatment was conceptualized by Salmon
(3) and later rephrased by Artiss
(4) in terms of three principles: 1) proximity—treatment is administered close to the front line, 2) immediacy—treatment is administered close in time to the symptoms’ onset, and 3) expectancy—the expectation is that the soldier will recover rapidly and resume functioning. This psychiatric first aid is time-limited, lasting between 48 and 72 hours. The aim is to meet the casualty’s physiological needs (e.g., food, drink, and sleep), provide temporary relief from harsh battle stressors, enable the exhausted and distressed soldier to regain some control, and decrease hyperarousal. In frontline treatment, human contact is used to reassure the soldier, encourage clarification and sharing of emotions, and humanize and legitimize fears. Frontline treatment allows expression of grief, guilt, and shame but challenges self-depreciation. It conveys to the distressed soldier the expectation of recovery and resumption of functioning.
Frontline treatment is guided by the notion that the soldier’s response is not evidence of an underlying disorder but a natural, appropriate response to the extreme stress of war. The soldier’s symptoms are viewed as stemming from the stress of combat. The intervention includes well-documented stress buffers, such as physical activity, curtailment of avoidant coping strategies (e.g., reference
5), and enhanced social support (e.g., reference
6), and has the further benefit of reducing the well-documented detrimental consequences of psychiatric labeling and the adoption of the sick role.
For the most part, the effectiveness of frontline treatment has been assessed on or near the battlefield in terms of return to duty and, to a lesser degree, recurrence of psychological breakdown. The rate of return to unit after frontline treatment seems impressive. Reports from World War I (e.g., reference
3), World War II (e.g., reference
7), the Korean War (e.g., reference
4), the Vietnam War (e.g., reference
8), and the Gulf War (reference
9) indicate high rates of restored functioning and return to duty. Furthermore, follow-up studies reveal that the vast majority of men who returned to combat duty after treatment performed satisfactorily or better. Although opponents of frontline treatment argue that it is used by the military in the attempt to conserve manpower even at the cost of retraumatizing soldiers (e.g., reference
10), surveys conducted in various war zones consistently report a decline in rates of psychiatric hospitalization and very low rates of recurrence
(7,
9,
11) in those who returned to their units.
Yet, despite the extensive use of frontline treatment and its apparent effectiveness on the battlefield, very little systematic research has been conducted
(12). War is clearly not an ideal time to conduct evaluation research. In the heat of battle, systemic clinical trials, with random allocation of patients and adherence to double-blind protocols, are hardly feasible.
The unique circumstances in the 1982 Lebanon War allowed for an empirical assessment of the effectiveness of frontline treatment. Although frontline treatment was the intervention endorsed by the Israeli Defense Forces during the war, combat stress reaction casualties were treated either by frontline treatment or in civilian facilities inside Israel. The fact that the location and type of treatment were determined largely by logistic constraints, such as battle conditions, the nature of the terrain, and the availability of transport, provided a quasi-experimental situation. In addition, the combat stress reaction cases that reached mental health personnel in the battle zone were documented, and the records were subsequently computerized. This combination of circumstances allowed a systematic evaluation of the effectiveness of frontline treatment
(13). This evaluation, carried out in 1983, revealed the effectiveness of frontline treatment in terms of relatively high rates of return to duty and relatively low rates of PTSD 1 year after the war. Use of each of the frontline treatment principles (proximity, immediacy, expectancy) was associated with better outcomes. Furthermore, rates of PTSD decreased linearly with the application of more treatment principles.
These findings showed the short-term benefits of frontline treatment. The question of whether the benefits are enduring has not been addressed, however. The current study revisits the combat stress reaction casualties of the Lebanon War 20 years later and examines the long-term effects of frontline treatment on their mental state and functioning.
Method
Subjects
This study examined a total of 429 Israeli veterans of the 1982 Lebanon War, including the following three groups: 1) frontline treatment group (N=79, or 88% of the frontline treatment group in the 1983 evaluation), consisting of veterans who received a diagnosis of combat stress reaction and received treatment on the front line in Lebanon; 2) rear echelon treatment group (N=156, or 67% of the 1983 rear echelon treatment group), consisting of combat stress reaction casualties who received their initial treatment in military clinics in Israel; and 3) comparison group (N=194, or 75% of the 1983 comparison group), consisting of soldiers who fought in Lebanon in units that had combat stress reaction casualties but who did not themselves receive a diagnosis of any physical or mental problems during the war. The participants in the 1983 evaluation who did and did not participate in the 20-year follow-up did not differ in sociodemographic background, posttraumatic or psychiatric symptoms, health status, or social functioning, as assessed in 1983.
The mean age of the study subjects was 47.25 years (SD=5.54). Asked to rank their family income, 13% ranked their family income below the national average, 62% as average, and 25% as higher than average. With regard to family status, 92.6% of all respondents were married, 2.1% were single, 5.1% were divorced, and 0.2% were widowers.
When the original study was designed in 1982, the subjects with combat stress reaction and the comparison subjects without combat stress reaction were matched for pre-military, military, and sociodemographic characteristics. It is unlikely that casualties were preselected for mode of treatment on the basis of the severity of their breakdown or any other feature that could bias the findings. A series of statistical analyses carried out for the present study showed no significant difference between the two treatment groups in age, education, economic status, living conditions, or country of origin. Nor did the groups differ in pre-military ratings of intelligence, motivation, rank, corps membership, or prewar adjustment problems or psychiatric symptoms. It is noteworthy that in operational debriefings conducted immediately after the ceasefire in 1983, the mental health officers who first examined the casualties consistently reported that allocation to treatment mode was determined by logistic constraints (see earlier discussion) rather than by any systematic screening.
Measures
Assessment of intervention
In the frontline treatment group, we assessed the application of the frontline treatment principles. Proximity was assessed on the basis of the place of treatment recorded in the soldiers’ medical files. Immediacy was assessed on the basis of subjects’ reports in 1983 about whether they received initial treatment within a day after onset of combat stress reaction symptoms. Expectancy was assessed on the basis of subjects’ reports in 1983 about whether the goal of their initial treatment had been to return them to their units.
For the frontline group, we also assessed whether subjects returned to their units after frontline treatment. Subjects were asked two questions in 1983. They were first asked, “Following treatment, did you return to your unit during the war?” (yes/no). Subjects who answered affirmatively were then asked whether they remained in their units, were assigned their old duties or new ones, or were discharged soon after they returned. Subjects who reported having gone back to their units were defined as “returned to unit,” whether they resumed their former duties or were assigned new ones. Subjects who reported not having gone back to their units or having gone back to their units only to be discharged on arrival were defined as “not returned to unit.”
We also assessed frontline subjects’ perceptions of the timing of their return to their units. In 1983, subjects were asked: “If you were returned to your unit during the war, was it 1) after you completely recovered, 2) before you completely recovered, or 3) when you were still feeling unfit?”
Outcome measures
To enable comparison with findings from the 1983 assessment, we used the same measures that were used then, including the PTSD Inventory, the Impact of Event Scale, the SCL-90-R, the Social Network Inventory, the Problems in Social Functioning questionnaire, and the UCLA Loneliness Scale.
The PTSD Inventory
(14), a self-report scale based on DSM criteria, was used to assess posttraumatic symptoms. The questionnaire consists of statements tapping both DSM-III and DSM-IV symptom criteria. Subjects are asked to indicate on a 4-point scale ranging from “never” to “often” the frequency with which they experienced each of the described symptoms. The scale has good psychometric properties
(13). In the current study, Cronbach alphas were 0.96 for symptom intensity, 0.93 for the intrusion scale, 0.90 for the avoidance scale, 0.91 for the arousal scale, and 0.94 for the number of symptoms. Concurrent validity of the scale was also high
(13) when it was compared both with widely accepted self-report measures
(15,
16) and with clinical diagnoses of PTSD
(13,
17).
The Impact of Event Scale
(15) is a 15-item scale tapping intrusion and avoidance tendencies. Subjects are asked to indicate on a 4-point scale from “not at all” to “often” how frequently they experienced each reaction during the previous week. Two total scores—intrusion and avoidance—were computed by summing the items corresponding to each scale. This is a widely used measure in trauma studies, with proven psychometric qualities
(16,
17). Cronbach alphas in the current study were 0.95 for intrusion and 0.88 for avoidance.
The SCL-90-R
(18) is a self-report measure that taps psychiatric symptoms during the 2 weeks before the assessment. It enables assessment of both the overall severity of psychiatric symptoms and the severity of each of nine symptom categories: somatization, obsessive-compulsive problems, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism, as well as additional symptoms. General distress is rated on three indices: 1) the global severity index, which is the mean intensity of the 90 symptoms; 2) the positive symptom total, which is the total number of positively endorsed symptoms; and 3) the positive symptom distress index, which is the mean intensity of the positively endorsed symptoms. In the current study, Cronbach alphas for the subscales ranged from 0.87 to 0.99.
Social support was measured by the 8-item revised Social Network Inventory (unpublished 1978 paper by D. Mueller), which taps expressive and instrumental support. Consistent with previous studies
(19), Cronbach alpha in the current study was high at 0.91.
The Problems in Social Functioning questionnaire
(20) is a 33-item self-report questionnaire examining problems in different areas of social and occupational functioning in the previous year. In the current study, reliability coefficients for social and occupational functioning were acceptable (alpha=0.76 and alpha=0.82, respectively).
Feelings of loneliness were assessed with the revised UCLA Loneliness Scale
(21). This scale consists of 20 items, 10 of which reflect satisfaction with social relationships and 10 of which reflect dissatisfaction. The original scale was found to have good psychometric qualities
(21). Similar results were obtained in the current study (alpha=0.87).
Stressful life events were assessed by a checklist of 20 life events experienced since the war, including family (e.g., bereavement), work (e.g., unemployment), and personal (e.g., severe illness) life events.
Procedure
The names and addresses of the participants in the 1983 study were obtained from updated Army records, and the persons were contacted by phone. Their participation in the present study was requested after the study aims were explained. Those who agreed to participate were offered the choice of meeting in their homes or at another location of their choice to complete the questionnaire. Before administration of the questionnaire, subjects signed an informed consent form. Data were collected in 2002.
Results
Long-Term Effects of Frontline Treatment
First, we examined the differences in PTSD rates in the three groups. Results revealed a significant group difference (χ2=33.01, df=2, p≤0.01). The rate of PTSD in the comparison group (13.9% [N=27]) was significantly lower than in both the frontline treatment group (30.4% [N=24]) (χ2=10.15, df=1, p≤0.01) and the rear echelon treatment group (41.0% [N=64]) (χ2=33.34, df=1, p≤0.001). However, although combat stress reaction casualties who received frontline treatment had a lower PTSD rate (30.4% [N=24]) than combat stress reaction casualties referred to rear echelon treatment (41.0% [N=64]), this difference was not significant.
In addition, we calculated the relevant odds (risk) ratios for development of PTSD in the three groups. For the frontline treatment group versus the comparison group, the odds ratio was 2.70 (95% confidence interval [CI]=1.44–5.06; Wald χ2=9.58, df=1, p<0.01). For the rear echelon treatment group versus the comparison group, the odds ratio was 4.30 (95% CI=2.57–7.21; Wald χ2=30.63, df=1, p<0.001). For the frontline treatment group versus the rear echelon treatment group, the odds ratio was 1.59 (95% CI=0.90–2.84; Wald χ2=2.52, df=1, p>0.05).
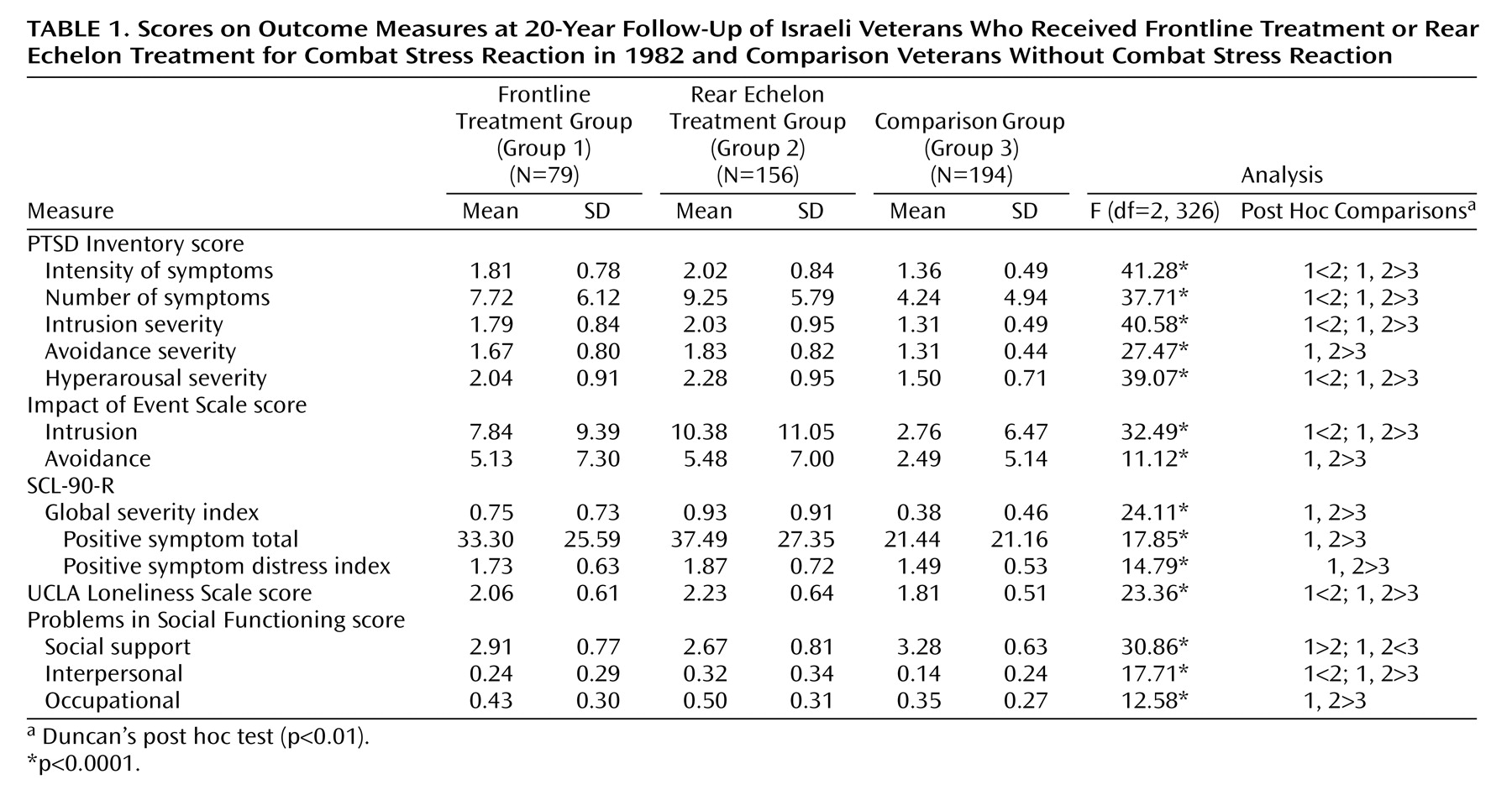
Second, we examined differences in the three groups’ levels of current psychopathology and social functioning. For this purpose, we conducted one-way multivariate and univariate analyses of variance (ANOVAs). The dependent variables were intensity and number of posttraumatic symptoms, severity of the three clusters of posttraumatic symptoms, the Impact of Event Scale intrusion and avoidance subscale scores, the three global distress scores (global severity index, positive symptom total, and positive symptom distress index), loneliness score, perceived level of social support, level of interpersonal functioning, and level of occupational functioning.
Table 1 presents the means, standard deviations, and F ratios from the analyses. The multivariate ANOVA of scores for the posttraumatic symptom clusters of the PTSD Inventory revealed a significant difference among study groups (F=15.38, df=6, 846, p≤0.01). As
Table 1 shows, univariate ANOVAs and Duncan’s post hoc tests indicated that the intensity and number of posttraumatic symptoms and the severity of intrusion and hyperarousal were significantly lower in combat stress reaction casualties who received frontline treatment than in those referred to the rear for treatment. As for the avoidance cluster, a similar although nonsignificant difference was observed. The two combat stress reaction groups reported significantly more PTSD symptoms and more severe PTSD symptoms than the comparison group.
The multivariate ANOVAs of the Impact of Event Scale scores also revealed a significant difference among study groups (F=16.57, df=4, 848, p≤0.01). Univariate ANOVAs and Duncan’s post hoc tests indicated that combat stress reaction casualties who received frontline treatment had a significantly lower Impact of Event Scale intrusion score than those in the rear echelon group, as well as a lower, although not significantly lower, avoidance score. The comparison group had significantly lower scores than the two combat stress reaction groups on both Impact of Event Scale subscales.
A significant multivariate effect of study group was also found in the three global SCL-90-R scores (F=8.10, df=6, 760, p≤0.01). Univariate ANOVAs and Duncan’s post hoc tests indicated that combat stress reaction casualties who received frontline treatment reported lower levels of global distress than combat stress reaction casualties who did not receive this intervention, but these differences were not significant. The two combat stress reaction groups endorsed significantly more distress on all three measures than the comparison group (
Table 1).
Similar results were noted for the four social functioning measures (loneliness, perceived social support, interpersonal functioning, occupational functioning) (F=8.41, df=8, 832, p<0.01). Univariate ANOVAs and Duncan’s post hoc tests indicated that combat stress reaction casualties who received frontline treatment reported significantly lower levels of loneliness, higher levels of perceived social support, and better interpersonal functioning than combat stress reaction casualties who did not receive this intervention. With regard to occupational functioning, the frontline treatment group reported better functioning than the other combat stress reaction group, but the difference was not statistically significant. Again, the two combat stress reaction groups were found to be significantly more impaired on all social functioning measures than the comparison group.
The Long-Term Effects of Frontline Treatment
To assess the cumulative effect of the application of the various principles of frontline treatment, we examined the relationships between the application of the treatment principles and each outcome measure. The findings showed that when all three treatment principles were applied, the PTSD rate was 25%; when two principles were applied, the rate was 32.6%; and when one principle was applied, the rate was 38.5%. The highest PTSD rate, 47.9%, was found among soldiers who had received none of the treatment principles. Although the differences did not reach significance, the percentages suggest a clear trend. One-way multivariate and univariate ANOVAs revealed a significant relationship between loneliness and the number of treatment principles applied (F=3.21, df=2, 76, p<0.05).
Return to Unit
We also assessed the relationships between return to unit and the other outcome measures. No significant differences were found in any of the outcome measures between combat stress reaction casualties who returned to duty and those who did not.
Perceived Timeliness of Return to Unit
The relationship between perception of the time of return to unit as appropriate and present mental state was also assessed. The results indicated that combat stress reaction casualties who received frontline treatment and who returned to duty before they felt entirely recovered currently had significantly more posttraumatic symptoms (50%) than those who returned after they felt fit (15%) (χ2=4.08, df=1, p<0.05). Those who returned to duty before they felt fit also reported more problems in occupational functioning than those who were returned after they felt fit (mean=0.61, SD=0.36, versus mean=0.26, SD=0.26) (t=2.98, df=29, p<0.01) and reported more problems in social functioning than those who returned to duty after they felt fit (mean=0.40, SD=0.30, versus mean=0.15, SD=0.30) (t=2.29, df=29, p<0.05).
Contribution of Type of Treatment and Postwar Stressful Life Events
Since 20 years elapsed between the Lebanon War and the current evaluation, we also assessed the relationship between treatment mode and life events that occurred in the interval. A one-way ANOVA revealed a significant group difference in the number of life events experienced (F=6.05, df=2, 425, p<0.01). Duncan’s post hoc tests (p<0.01) showed that the comparison group reported significantly fewer life events (mean=4.12, SD=2.41) than both the frontline treatment group (mean=4.90, SD=2.75) and the rear echelon treatment group (mean=5.04, SD=2.79) but that the two treatment groups did not differ significantly in the number of life events they reported.
Multiple regression analysis was used to assess the unique contribution of study group (frontline treatment group versus rear echelon treatment group and frontline treatment group versus comparison group) and number of life events since the war to the severity of current PTSD (number of PTSD symptoms endorsed). These variables explained 31.4% of the variance in number of PTSD symptoms (F=62.44, df=3, 424, p<0.001). Each of the three predictors made a significant unique contribution: life events (beta=0.40, p<0.001), frontline treatment versus rear echelon treatment (beta=–0.12, p<0.05), and frontline treatment versus comparison group (beta=–0.23, p<0.001). Participants who reported a higher number of life events also endorsed a higher number of posttraumatic symptoms. More PTSD symptoms were endorsed by combat stress reaction casualties who did not receive frontline treatment than by the other participants.
Discussion
This study assessed the long-term effectiveness of frontline treatment 20 years after its application in the 1982 Lebanon War. The results reveal that traumatized soldiers who received frontline treatment had lower rates of posttraumatic and psychiatric symptoms, experienced less loneliness, and reported better interpersonal functioning than similarly traumatized soldiers who did not receive frontline treatment. In addition, the findings point to a cumulative effect of the application of frontline treatment principles. We found that when more principles of frontline treatment were applied, psychiatric outcomes were better, although this result did not reach statistical significance. On the other hand, no differences were found in the symptoms or functioning of soldiers with combat stress reaction who returned to their units after receiving frontline treatment and those who did not return to their units. Time of return to unit, however, was related to outcome. Combat stress reaction casualties who received frontline treatment and who felt, in 1983, that they had been returned to their units after they had completely recovered fared significantly better than similarly traumatized men who felt that they had been returned to their units before they had completely recovered.
Several explanations may be offered for the effectiveness of frontline treatment. First, frontline treatment may provide the distressed soldier with temporary relief in relative safety and may thus reduce hyperarousal, which has been found to be associated with risk for chronic PTSD
(22,
23), and may help the soldier regain a measure of control
(24). Together these effects may reduce the risk for maladaptive behavior and possibly limit the generalization of emotional reactivity.
A second explanation may be anchored in the communication of the view that combat stress reaction casualties are essentially healthy individuals experiencing a temporary crisis and that they can be expected to have a rapid recovery. These messages, whose absorption may be facilitated by the high level of suggestibility of persons in an acute stress reaction, may help the soldier to see his breakdown as a normal reaction to the pressure of combat and as one that he can overcome. These messages might also help to restore his sense of self-efficacy after the breakdown, as would the demands for activity (e.g., keeping clean, participation in sports, etc.) that are an integral part of frontline treatment.
Frontline treatment may also further recovery by enabling the casualty to continue to enjoy the social support of his comrades and commanders, who can readily visit him during his treatment. This element may help to restore the sense of affiliation that was disrupted by the combat stress reaction
(25). Furthermore, social support has consistently been shown to aid recovery from psychiatric crisis (e.g., references
6,
20,
26).
Another possibility is that frontline treatment discourages avoidant coping, which has been shown to predict PTSD among soldiers with combat stress reaction (e.g., reference
5). Unlike soldiers in the rear echelon treatment group, soldiers treated on or near the front remain exposed to combat stimuli similar to those that brought about their breakdown. Their gradual reexposure in a supportive and reassuring situation may lead to desensitization, which enables them to cope with the stimuli and reduces their need to avoid them.
Finally, frontline treatment may help to stem the cascading loss of resources that occurs with combat stress reaction
(27). Just as traditional first aid stops hemorrhage and saves the wounded soldier’s life, frontline treatment can be seen as psychological first aid that promotes coping and self-efficacy and minimizes deterioration into the sick role and incapacity.
The main methodological limitation of this study is its quasi-experimental design, which did not meet the strict criteria for controlled clinical trials, such as random allocation of subjects and double-blind protocols. However, such procedures are impossible in combat, and allocation to treatment mode was based on logistic considerations, not severity of the acute reaction.
Nevertheless, the study findings demonstrate the effectiveness of frontline treatment for combat stress reaction even 20 years after combat. Most of the short-term benefits of frontline treatment that were documented two decades ago endured the passage of time. Although frontline treatment did not prevent the development of PTSD in all cases, it did seem to have reduced the risk. In light of the psychological and economic toll of PTSD
(2), this finding is potentially of considerable clinical significance.
Our findings support the view that the acute phase of traumatization is a critical period and that early intervention should occur during this window of opportunity to prevent the crystallization of combat stress reaction into entrenched PTSD
(28). They also suggest that frontline treatment principles, especially immediacy and expectation, might be adopted to the treatment of acute stress reaction stemming from nonmilitary traumatogenic events, such as rape, severe illness, accidents, or natural disasters. Such interventions should be accompanied by systematic evaluation research.