For years, investigators have expressed concern about the validity of assessments of personality traits and personality disorder made within the context of a depressive episode. These concerns resulted from studies demonstrating that successful treatments of major depressive disorder can lead to changes in measures of personality and personality disorder (
1–
4). For example, a seminal study by Hirschfeld et al. (
1) found that certain personality traits, such as emotional strength, dependency, and extraversion, changed significantly more at 1-year follow-up in treated depressed patients who had recovered than in depressed patients who had not recovered. Such results have led some investigators to conclude that personality assessments of symptomatic depressed patients may not accurately reflect their trait characteristics before, between, or after depressive episodes (
5,
6). Thus, assessing personality traits and related problems during a depressive episode could lead to overdiagnosis of personality disorder and perhaps to unwarranted conclusions about prognosis, given that comorbid personality disorder is generally considered a risk factor for poorer outcome (
7–
10, but see also reference 11). As a result, some have recommended considering adjusting for current mood when assessing personality (
6).
However, a number of research findings temper the conclusion that a depressive episode necessarily leads to overdiagnosis of personality disorder. First, instructional sets that focus on differentiating long-term characteristics from current state during the assessment may reduce or eliminate emotional state effects in self-report and interview assessments (
12,
13). Second, some studies that have demonstrated marked state effects on personality measures used instruments saturated with psychopathology as opposed to personality traits, such as the MMPI or the Millon Clinical Multiaxial Inventory (
1–
3). Third, most studies suggesting mood effects on personality have done so in the context of demonstrating changes in personality associated with the treatment of depression (
2,
4,
14). However, as Fava et al. (
15) have observed, it is also possible that antidepressant treatments affect a range of characteristics beyond depression and that some of these nonspecific treatment effects lead to changes in personality problems.
Fourth, evidence suggests that the personality self-descriptions offered by depressed patients typically converge with descriptions provided by family informants (
16), whose judgments are presumably unaffected by the patient's mood state. Fifth, the duration of many studies was limited to that of a brief clinical trial, which may be too short to distinguish enduring from transitory personality change. Finally, many studies focus exclusively on personality changes in depressed patients (
14) without using a nondepressed comparison group to gauge whether any observed changes in personality reflect variability beyond changes that might be expected in individuals without mood disorders.
In this study, we tested the hypothesis that the presence of a major depressive episode will lead to overidentification of problematic personality traits that fail to persist over the long term and lower stability in normative personality traits over the long term. To do so, we examined personality changes in patients experiencing a major depressive episode who lacked significant personality pathology; patients experiencing a major depressive episode who had significant comorbid personality pathology; and patients not experiencing a depressive episode who had significant personality pathology. This study is unique in examining long-term outcome in patients presenting with depression who differ markedly in their initial presentation of personality pathology. If indeed a major depressive episode seriously confounds assessment of personality and personality disorder, then patients who present with comorbid depression and personality disorder might be expected to have long-term outcomes more similar to those of "pure" depressed patients than to those of "pure" personality disorder patients. Furthermore, one would expect that long-term personality trait stability should be appreciably lower in both groups with depression than in those with personality disorders only. However, if these predictions do not hold and comorbid patients resemble "pure" personality disorder patients more than "pure" depression over the long term, these results would indicate that personality and personality disorder can be successfully identified during a major depressive episode.
Method
Participants
Participants for this study were drawn from the Collaborative Longitudinal Personality Disorders Study (CLPS;
17), a multisite prospective, naturalistic longitudinal study. Recruitment aimed to obtain a diverse, representative sample from inpatient and outpatient clinical programs affiliated with four recruitment sites (Brown, Columbia, Harvard, and Yale Universities). CLPS enrolled 668 participants 18 to 45 years of age who had either at least one of four personality disorders or current depression without any personality disorder. CLPS focused on four specific personality diagnoses—schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders—which were selected because of their prevalence and research base in clinical samples and to span the three DSM-IV clusters. Of the 668 participants in CLPS, 573 met criteria for the personality disorder study group and 95 for the major depressive disorder (without personality disorder) group. Detailed descriptions of the CLPS methods and characteristics of the overall study group have been previously reported (
17), including specific co-occurrence patterns among the axis I and axis II diagnoses in this study (
18). There was extensive comorbidity of major depression and personality disorder, a finding that echoes those reported for other clinical samples (
19), and most participants received a variety of treatments over the course of the study (
20).
The present study focused on membership in one of three study groups. Patients were assigned to the "depression only" group if they met criteria for a major depressive episode, were at least two criteria below the diagnostic threshold for all specific personality disorders, and met a total of fewer than 15 personality disorder criteria at the baseline assessment. Thus, in contrast to most previous studies of this issue, this group constitutes a "pure" depressed group with respect to personality pathology. Participants were assigned to the "personality disorder only" group if they met criteria for a DSM-IV personality disorder at the baseline assessment but did not meet criteria for a major depressive episode. Finally, patients were assigned to the "personality disorder plus major depression" group if they met criteria for both a personality disorder and a major depressive episode at baseline assessment. Patients who met criteria for a personality disorder and who had a lifetime diagnosis of major depression but were in remission at baseline were not included in the study to control for any artifacts associated with depression relapse.
Assessment Protocol
At baseline, an interviewer administered the Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Version (SCID;
21) and the Diagnostic Interview for DSM-IV Personality Disorders (
22). Participants were reinterviewed after 6 and 12 months and then yearly thereafter for 5 more years. At 6 years, a comprehensive evaluation was conducted that included the Diagnostic Interview for DSM-IV Personality Disorders as well as the self-report measures described below. A total of 522 (78%) of the original 668 study participants participated in the year 6 follow-up evaluation, of whom 433 had complete interview and self-report data: 119 were assigned to the personality disorder only group, 73 to the depression only group, and 241 to the personality disorder plus major depression group. The proportion of those who completed the study relative to those who did not complete the study did not differ among the three study groups.
As noted in a previous report (
23), the four personality disorders targeted in this study demonstrated comparable stability across the 6-year interval studied here (year 6 estimated stability, in men: schizotypal=0.57, borderline=0.53, avoidant=0.57, obsessive-compulsive=0.37; in women: schizotypal=0.61, borderline=0.46, avoidant=0.59, obsessive-compulsive=0.52). Also, among patients diagnosed with personality disorders, there were no differences in comorbid depression status among the four study personality disorder diagnoses; for schizotypal personality disorder, 63.2% presented with concurrent depression, and the numbers were comparable for borderline (65.5%), avoidant (69.4%), and obsessive-compulsive (68.7%) personality disorders.
Measures
The SCID was administered only at baseline. Kappa coefficients (
24) for interrater reliability for psychiatric diagnoses ranged from 0.57 to 1.0; the kappa value was 0.80 for major depression and 0.76 for dysthymic disorder (
25).
The Diagnostic Interview for DSM-IV Personality Disorders is a semistructured interview to assess DSM-IV personality disorders. It requires that criteria be pervasive for at least 2 years and characteristic of the person for most of his or her adult life. Interrater reliability kappa coefficients for diagnoses ranged from 0.58 to 1.0 (
25). Test-retest reliability kappa coefficients ranged from 0.69 to 0.74 (
25). In this study, the total number of DSM-IV personality disorder criteria coded as present and clinically significant was used as an indicator of global personality pathology. Reliability for the total personality disorder criteria count as estimated by coefficient alpha was 0.95 at baseline and 0.95 at 6-year follow-up.
The NEO Personality Inventory–Revised (
26) was designed to comprehensively assess the five dimensions of the five-factor model (
27) of personality. Extensive research has suggested that these factors—neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness—can be universally identified and explain much of the variation in normal personality. The NEO Personality Inventory–Revised scales are normed using T scores, where 50T represents the average of a community sample and 10T represents the standard deviation in that sample. Internal consistency reliabilities for the five domains in this sample at the baseline assessment ranged from 0.87 to 0.92.
The Longitudinal Interval Follow-Up Evaluation (
28) is a structured interview that measures, among other variables, the Global Assessment of Functioning (GAF) scale that constitutes axis V of DSM-IV. The GAF scale is a commonly used clinician-rated single item ranging from 1 to 100, with higher scores indicating better overall adjustment and higher levels of functioning.
Depressive symptoms were measured with the depression scale of the Personality Assessment Inventory (
29). The Personality Assessment Inventory is a broad-ranging clinical assessment that contains 11 clinical scales, one of which is the 24-item depression scale, a dimensional measure of depressive symptoms divided into three subscales reflecting different aspects of depressive symptoms: cognitive, affective, and physiological. As with the NEO Personality Inventory–Revised, the depression scale and subscales are normed using T scores. The reliability and validity of the depression scale and subscales with respect to other commonly used markers of depressive symptoms have been extensively documented (
29). In this study, reliability at 6-year follow-up as estimated by coefficient alpha was 0.94 for the depression full scale and 0.87, 0.92, and 0.77 for the cognitive, affective, and physiological subscales, respectively. The depression scale was not administered at baseline.
Data Analysis
One-way analyses of variance, followed by Bonferroni post hoc tests, were used to compare differences at 6-year follow-up among the three study groups with respect to degree of personality pathology and depressive symptoms, extremity of personality traits, and absolute value of changes observed on personality trait measures between baseline and year 6 assessments. Pearson correlations were computed to compare the three study groups on the stability of personality trait and pathology measures over the 6-year study interval, with significance of differences among these stability estimates tested using a z test of comparisons between independent correlations.
Results
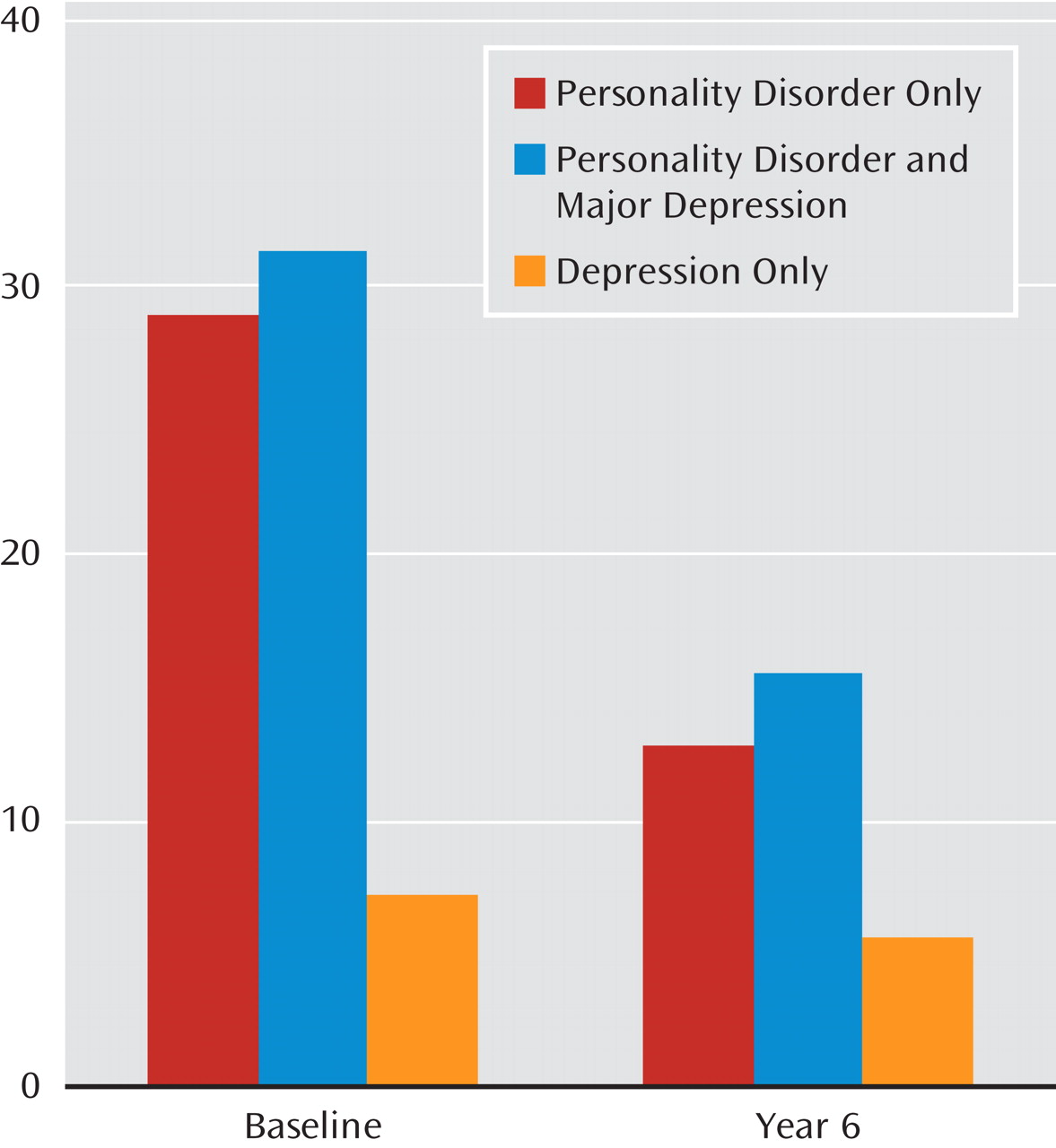
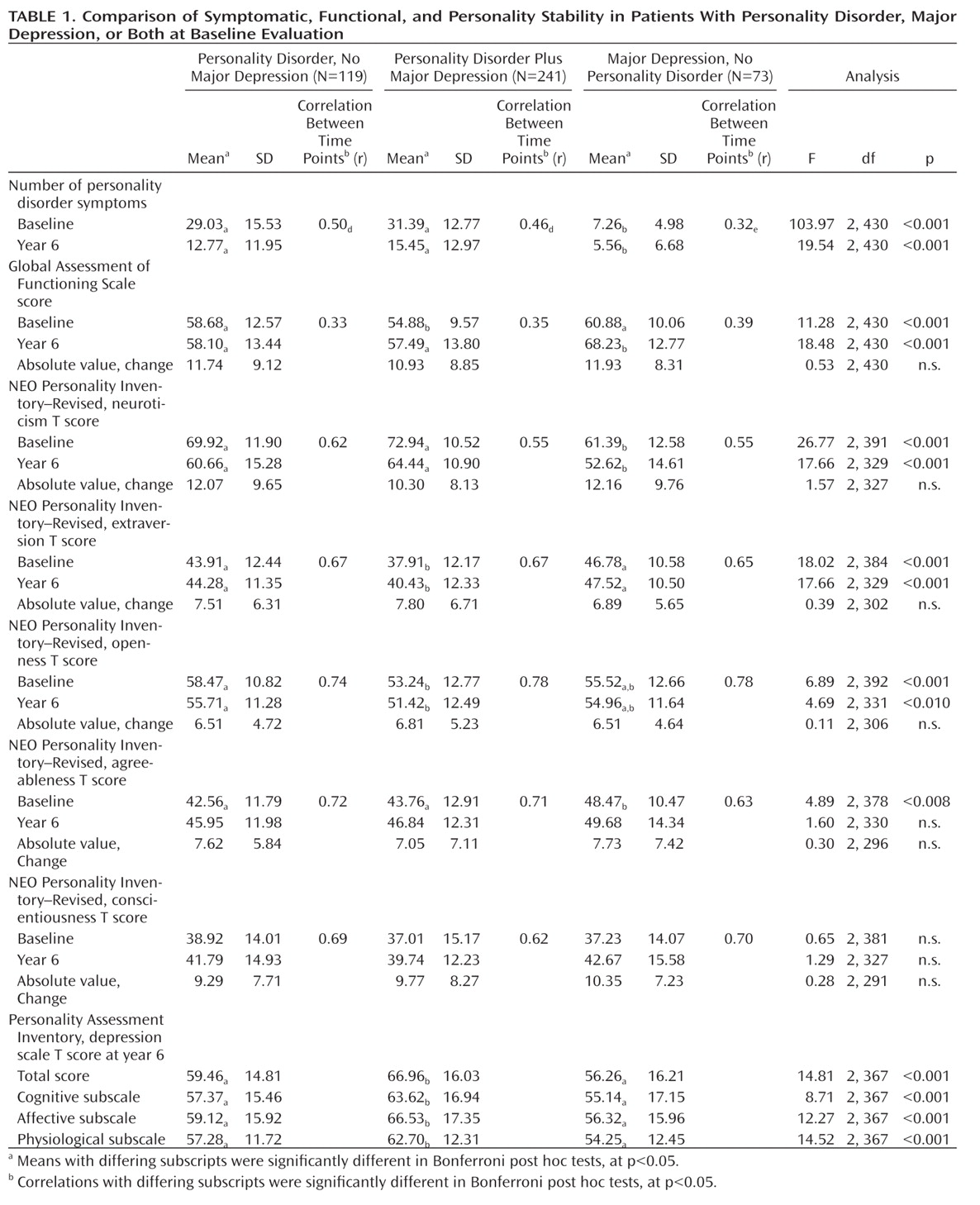
Table 1 summarizes differences among the three study groups over the course of the study. As expected given the construction of the study groups, there were large differences at baseline in the number of personality disorder symptoms present between the depression only group and the two personality disorder groups. There were no differences at baseline between the personality disorder plus major depression group and the personality disorder only group in degree of expressed personality pathology, with virtually identical criterion counts. Although both personality disorder groups demonstrated significantly more features of personality disorder than the depression only group at 6-year follow-up (
Figure 1), the difference between personality disorder only and personality disorder plus major depression groups was not statistically significant. This persistence of considerable personality pathology in the personality disorder plus major depression group contradicts the prediction that the presence of the depressive diagnosis would lead to overidentification of personality issues that would not endure. Indeed, the personality problems of the personality disorder plus major depression group were slightly more marked than those of the pure personality disorder group at follow-up.
A further analysis examined the stability of the personality disorder criterion count to determine whether the presence of a depressive episode resulted in less stable presentations of general personality pathology over time. Moderate stability was observed in the personality disorder plus major depression (r=0.51) group and the personality disorder only (r=0.46) group, with lower stability in the depression only group (r=0.32). The limited range of personality disorder criteria observed in the depression only group as a function of their selection criteria made lower stability correlations in this group expectable. Of greater interest, there was no significant difference in the stability correlations for personality disorder patients with and without depression.
Table 1 also indicates mean GAF scores at baseline and at year 6, the mean absolute value of observed GAF changes during this interval, and GAF stability correlations for the three groups. At year 6, the depression only group demonstrated significantly higher functioning levels than either the personality disorder plus major depression group or the personality disorder only group, while GAF differences at baseline in the depression only group were comparable to those of the personality disorder only group. Once again, the persistence of functional impairment in the personality disorder plus major depression group runs counter to the hypothesis that the diagnosis of personality disorder in these depressed patients was an artifact of the baseline depression.
Table 1 also presents mean scores, mean absolute value of observed changes, and stability correlations for the three groups on the normal trait domains of the NEO Personality Inventory–Revised. The largest changes were observed on neuroticism, with mean scores declining over time for all three study groups. Differences between groups were observed at baseline for some traits, as expected from the theoretical and empirical link between five factor traits and personality disorders (
27). Of particular interest for the present study is the stability of observed differences between groups over time. Across all five trait domains, the personality disorder plus major depression and personality disorder only groups either did not differ at baseline and at follow-up or differed in a consistent manner at both baseline and follow-up. In other words, although the personality disorder plus major depression group and the personality disorder group proved to be similar on some traits and different on others, these similarities and differences proved to be persistent over 6 years. This finding supports the conclusion that the observed personality pattern of the personality disorder plus major depression group at baseline was not the result of a transient mood state.
While the mean scores for groups are informative, group averages can mask instability in personality presentation when some individuals increase on a trait while others decrease on the same trait, resulting in a small average change that obscures large changes at the individual level. Thus, Table 1 also presents the mean absolute value of T score change on the NEO Personality Inventory–Revised trait domains for each study participant in the three groups. For all five traits, none of the three groups appeared to differ in magnitude of observed personality changes. Finally, examination of 6-year trait stability estimates for the five trait domains yielded moderate to large stability estimates for all study groups, ranging from 0.55 to 0.78. Tests of the difference between pairs of stability correlations from the different samples across the five traits measured by the NEO Personality Inventory–Revised revealed no differences in stability as a function of group membership over the 6-year period studied.
To further examine the distinct issues of state versus trait effects and mood, the status of depressive symptoms was ascertained at the 6-year follow-up. Table 1 summarizes scores on the depression scale of the Personality Assessment Inventory for the three groups. For the full depression scale as well as for the cognitive, affective, and physiological subscales, the personality disorder plus major depression group demonstrated higher levels of depressive symptoms than the depression only group at 6-year follow-up. In fact, on every depression marker, the personality disorder plus major depression group obtained a score at least one standard deviation above community norms at follow-up, while mean scores for the depression only group were consistently below this threshold. Along similar lines, follow-up diagnostic evaluation revealed that 29.2% of the personality disorder plus major depression group met criteria for major depression at 6-year follow-up, whereas only 8.0% of the depressed only group still met depression criteria at follow-up (χ
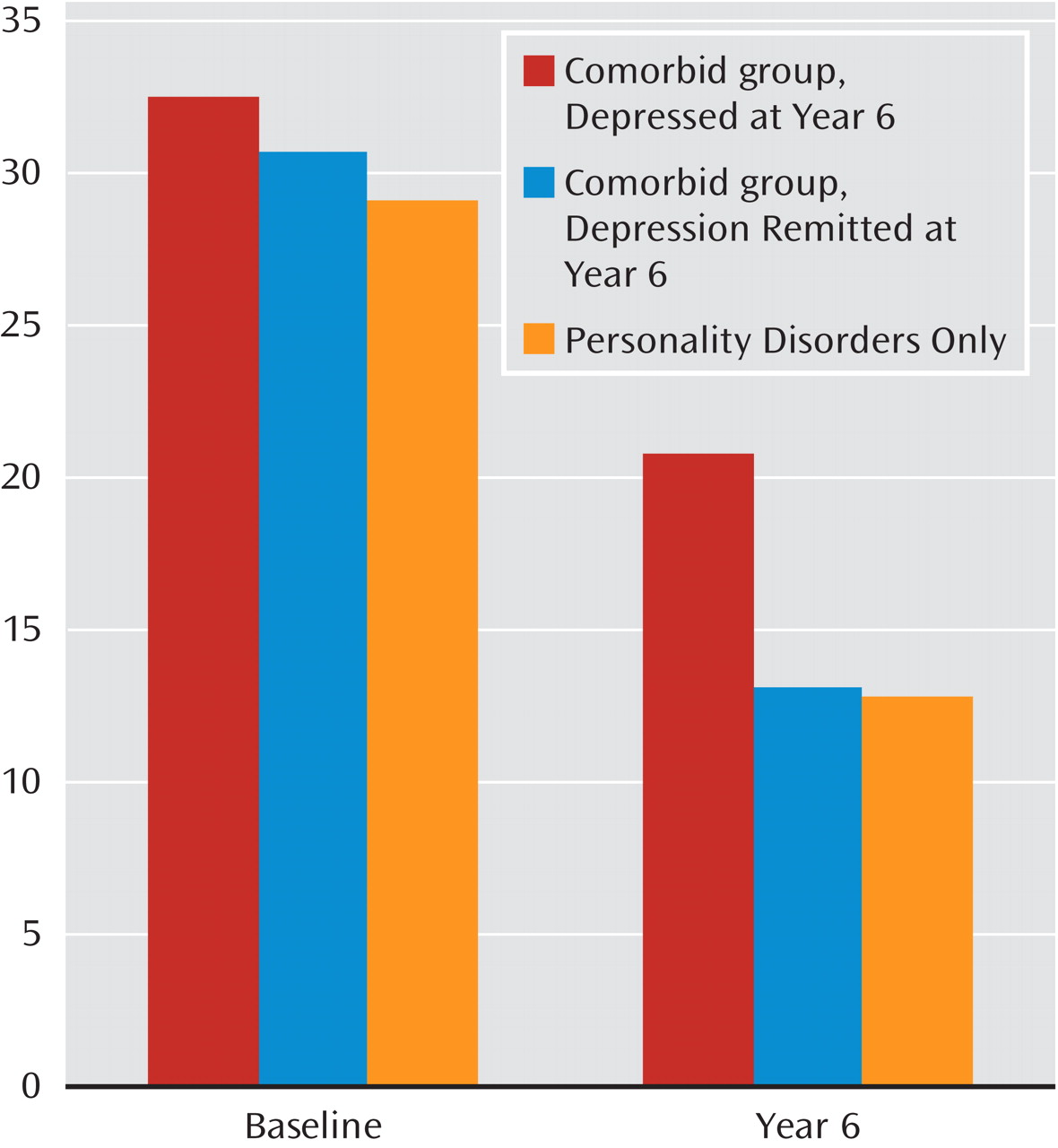
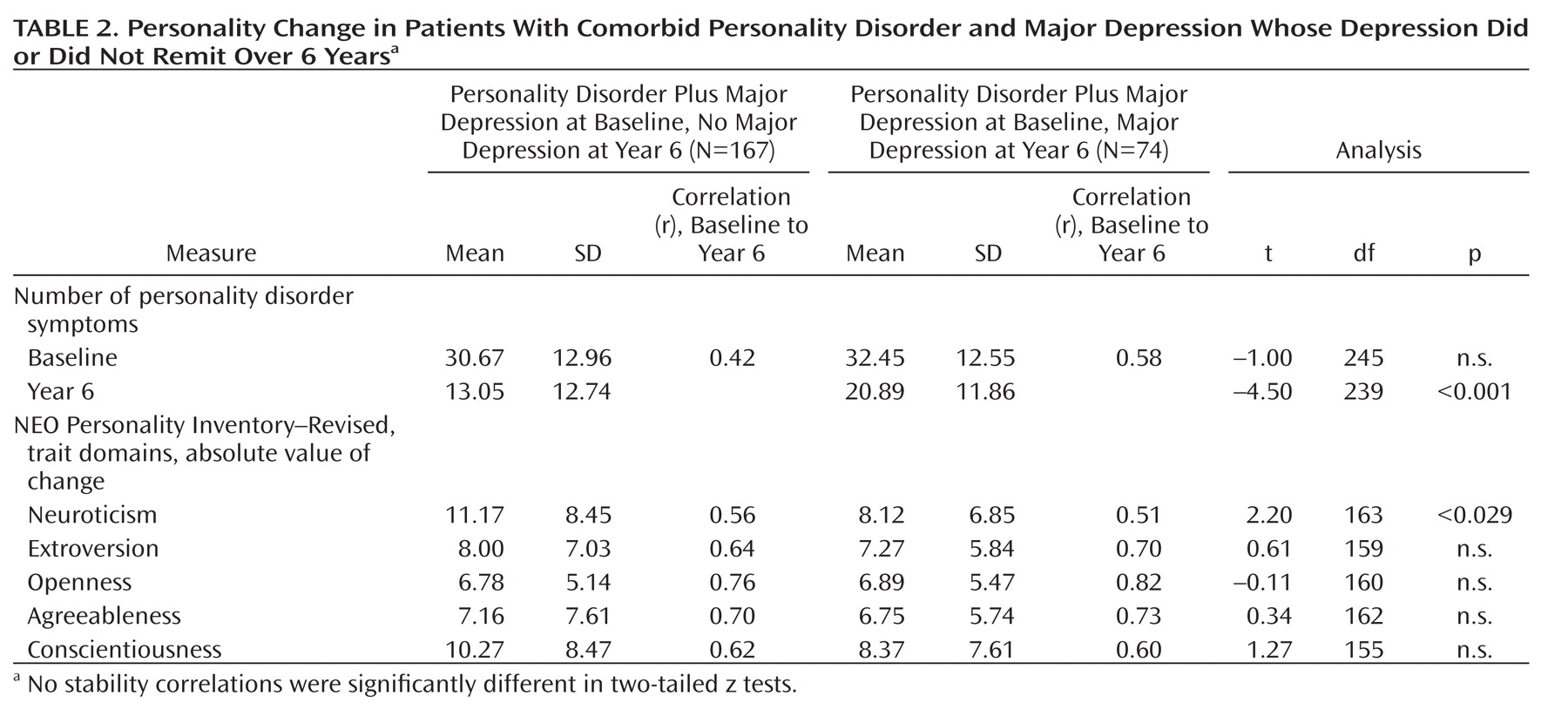
2=14.44, df=1, p<0.001). Thus, relative to the depression only group, the depressive symptoms of the personality disorder plus major depression group appeared to persist over the 6-year follow-up interval, which suggests that the depressive symptoms observed in this group at baseline reflected persistent mood problems (consistent with personality disorder) rather than a transient mood state that resulted in an inaccurate diagnosis of personality disorder. To more closely examine this issue, we compared personality changes in patients in personality disorder plus major depression group who continued to meet criteria for major depression at the 6-year evaluation (N=74) with those in patients in the personality disorder plus major depression group who no longer met criteria at follow-up (N=167) (patients in the depression only group were not included in these analyses because nearly all had remitted). These comparisons (
Table 2) demonstrate that patients in the personality disorder plus major depression group whose depression had remitted by the 6-year follow-up showed comparable stability in personality traits but greater changes in total personality disorder symptoms and neuroticism scores. However, comparing the mean scores of these patients with those of patients in the personality disorder only group (
Figure 2) reveals no difference between the two groups—in other words, the personality problems in personality disorder patients whose depression had remitted (an average of 13.05 personality disorder criteria met) were directly comparable at 6-year follow-up to those observed in personality disorder patients who did not have a baseline depression diagnosis (an average of 12.77 criteria met). Thus, even the personality disorder plus major depression patients whose depression remitted during the study demonstrated personality outcomes that resembled those of typical personality disorder patients.
Discussion
Because the presence of comorbid personality pathology can complicate the course and treatment of depression (
8), clinicians and researchers need to evaluate prominent personality traits and problems in any patient presenting during a depressive episode. However, concerns about the validity of personality assessment in the context of depressed mood (
5) have led to suggestions that state-related cognitive distortions or perceptual biases may render it difficult if not impossible to distinguish enduring personality characteristics from more transient phenomena. We sought in this study to determine whether a comorbid personality disorder diagnosis assigned in the midst of a major depressive episode did in fact reflect personality traits or problems that were transient and unstable or whether the comorbid personality disorder accurately identified long-standing problems and patterns that were likely to persist. Our results consistently supported the latter proposition: at 6-year follow-up, patients who were initially diagnosed with both major depression and personality disorder resembled other personality disorder patients in their personality pathology as well as in the stability and change in their normative personality traits. Furthermore, the depressive symptoms initially observed in the personality disorder plus major depression patients appeared to persist more than those of depression only patients, at levels well above community norms, which supports the hypothesis that the mood issues identified in these patients were related to trait rather than state phenomena—traits that may adversely affect recovery from depression. Even when the depressive features did not persist in the personality disorder plus major depression patients, these patients continued to demonstrate levels and stability of personality features comparable to those observed in the personality disorder only group. Moreover, these findings were not a result of any one particular variant of personality disorder; the four personality disorders studies demonstrated similar stability over the study interval and also had similar rates of comorbid depression.
The relative persistence of personality traits and issues does not mean that they are immutable phenomena. Indeed, as previous studies from our group and others (
30–
32) have shown, appreciable changes in personality pathology are observable, even over intervals as brief as 6 months (
33,
34). Thus, although previous studies have interpreted personality changes observed during treatment of depression as indicative of state influences on personality assessment, such changes may instead reflect valid alterations of personality characteristics. This interpretation is supported by the findings in this study that personality problems, while diminishing over time, continue to persist over years in patients with personality disorders to a degree well in excess of that in patients who do not manifest a personality disorder at the index evaluation. Furthermore, the presence of comorbid major depression in a patient with a personality disorder appears to have little impact either on the persistence of observed personality problems or on the stability of normative personality traits. In either case, the personality problems tend to persist, the normative traits demonstrate moderate to high stability, and depressive features observed in these patients are likely to endure over the long term rather than ameliorate over time.
In previous reports (
35,
36), we suggested that personality problems tend to reflect a hybrid of dynamic and enduring elements that each contribute to an understanding of personality disorder. As noted earlier, an increasing body of evidence suggests that the frequent observation of personality disorders among depressed patients is not an artifact of mood state on personality but more likely reflects the markedly increased risk for the development of depression among patients with problematic personality traits (
10,
37). At the same time, studies documenting personality shifts associated with the treatment of depression, rather than calling into question the validity of personality disorder diagnoses, may instead provide intriguing clues to the mechanisms that underlie the more dynamic elements of personality pathology. The interplay between state and trait in the assessment and diagnosis of personality, psychopathology, and their interface is more than one of simply bias or confound. Achieving a greater understanding of this interplay may serve to clarify core processes that lie at the heart of some of the most commonly encountered clinical conditions.