Psychotic episodes during the postpartum period are life-threatening psychiatric emergencies, occurring after nearly 0.1% of all deliveries. The strongest predictor for postpartum psychosis is a history of bipolar disorder and/or postpartum psychosis (
1–
3). Consequently, guiding women at high risk for psychosis through pregnancy and the postpartum period is a major challenge for mental health practitioners and obstetricians (
4–
6). Although immediate treatment of affective instability or psychosis is clearly warranted, relapse prevention is widely viewed as the most desirable strategy. Indeed, previous studies in high-risk women provide strong support for the benefits of lithium prophylaxis during pregnancy and the postpartum period (
7–
12). However, the benefits of medication for relapse prevention need to be carefully weighed against risks for the fetus during pregnancy, neonatal complications following delivery, and breast-feeding in the postpartum period (
13).
Previous studies of peripartum relapse have largely focused on women with a history of bipolar disorder. Viguera et al. provided clear evidence that discontinuation of medication leads to high rates of relapse in bipolar women during pregnancy (
7,
8). Further, four studies with smaller study groups have shown that prophylaxis with lithium is protective for the occurrence of relapse postpartum (
9–
12). In all four studies, lithium was continued during pregnancy, started in the last trimester of pregnancy, or started immediately postpartum.
While lithium has been demonstrated to be effective in substantially reducing the risk of peripartum relapse, the precise timing of when to initiate lithium prophylaxis, during pregnancy or immediately postpartum, remains unclear. An urgent need exists for clinical data that can be used to adequately weigh the risks and benefits of prophylaxis throughout the entire peripartum period.
Accordingly, we now describe the clinical outcomes of a peripartum prevention program designed to reduce the incidence and severity of peripartum relapse in women with a history of bipolar disorder, postpartum psychosis, or both. Pregnant women already on a maintenance regimen of lithium were advised to continue this prophylactic treatment during pregnancy and the postpartum period. High-risk women who were clinically stable and medication free at the time of evaluation were advised to start lithium prophylaxis immediately postpartum. These standardized clinical guidelines provided us the opportunity to compare the benefits of lithium prophylaxis during pregnancy and starting it immediately postpartum in women at high risk for perinatal psychosis. It is important to note that although postpartum psychosis is widely considered as a new episode of bipolar disorder, some studies have indicated that postpartum psychosis is distinct from bipolar disorder (
3,
14–
17). Therefore, we investigated the clinical outcomes of women with a history of psychosis limited to the postpartum period and of those with a history of bipolar disorder.
Method
Participants
Between January 2003 and December 2010, a total of 618 referrals to the outpatient clinic of the Peripartum Prevention Program at the Department of Psychiatry, Erasmus Medical Center (Rotterdam, the Netherlands), were evaluated. Requests for evaluation and clinical management during pregnancy and the postpartum period were made by obstetricians, psychiatrists, and general practitioners. This study was approved by the institutional review board of the Erasmus Medical Center.
Psychiatric diagnosis was obtained through a semistructured interview by a psychiatrist and review of clinical records. We included women with bipolar I or bipolar II disorder with only nonpuerperal episodes and those with both puerperal and nonpuerperal episodes. Further, we also included women with a history of postpartum psychosis but without any manic or psychotic symptoms outside the postpartum period. Since “postpartum psychosis” is not described as a separate disease entity in DSM-IV, we defined “postpartum psychosis” as a history of any of the following DSM-IV diagnoses: psychotic disorder not otherwise specified, brief psychotic disorder, or mood disorder (manic, mixed, or major depressive episode) with psychotic features, all requiring the specifier “with postpartum onset” (≤4 weeks after delivery). Women with chronic psychotic disorders such as schizophrenia or schizoaffective disorder were excluded.
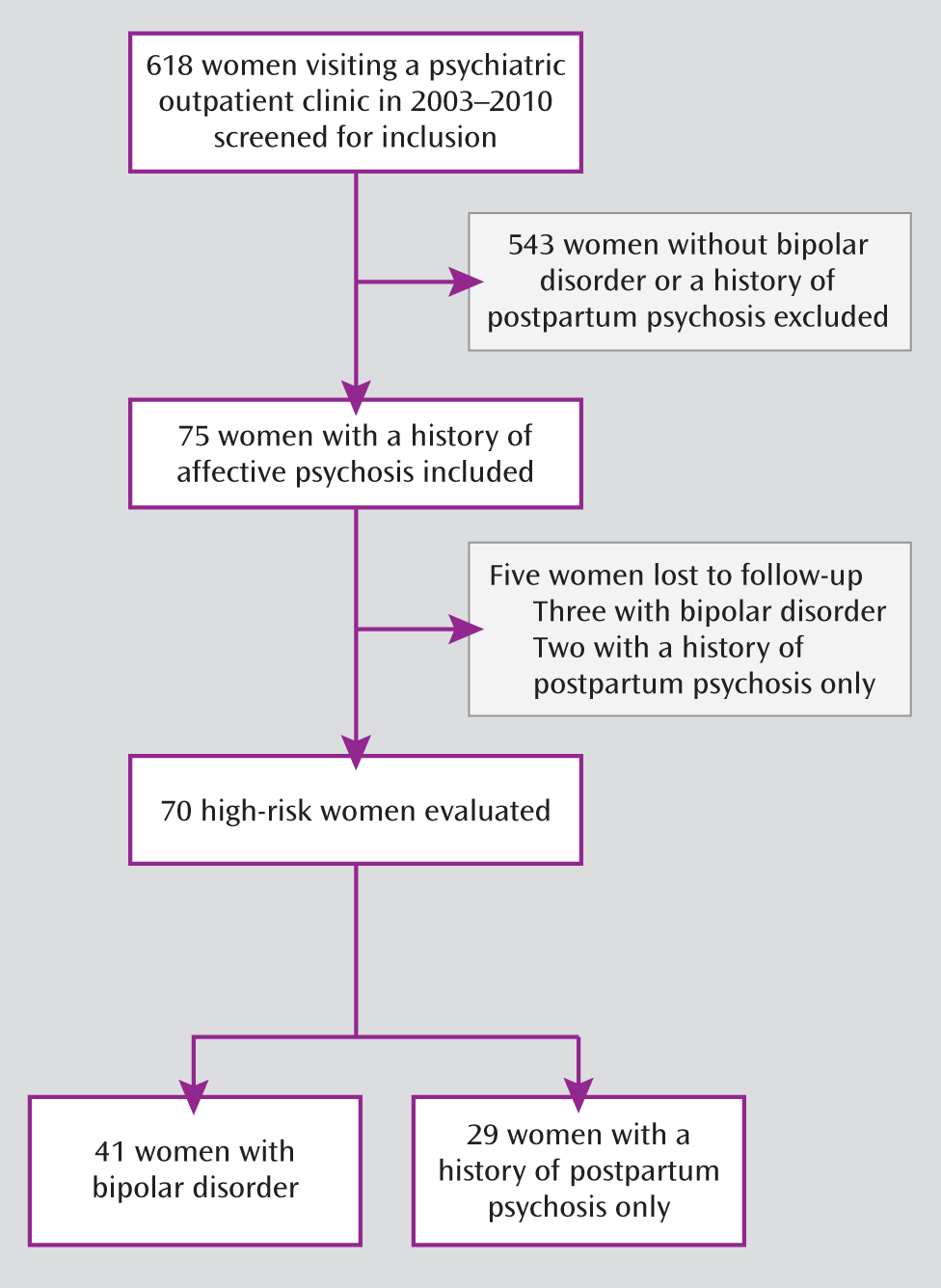
In total, 75 pregnant women fulfilled the inclusion criteria. Five women were lost to follow-up during pregnancy (
Figure 1). Therefore, in total we included 70 pregnant women at high risk for postpartum psychosis. Of this number, 29 had a history of postpartum psychosis but without any manic or psychotic symptoms outside the postpartum period. Conversely, we included 41 women with a diagnosis of bipolar disorder based on a history of nonpuerperal episodes with or without puerperal episodes. For women who had more than one delivery during the study inclusion period, we included only the most recent pregnancy in the main analysis.
Peripartum Prevention Program
The Peripartum Prevention Program was designed to provide standardized evidence-based clinical care for women at high risk for peripartum relapse (
18). Women enrolled in the program received their full obstetric care through the Department of Obstetrics and Gynecology and peripartum psychiatric care through the Department of Psychiatry.
We advised women who were using a mood stabilizer at the time of evaluation to continue pharmacologic treatment during pregnancy. Given that lithium monotherapy has the largest evidence base as an effective mood stabilizer in the peripartum period, this was our primary pharmacological recommendation (
2,
19). We also informed women about teratogenic risks of lithium during early pregnancy and the elevated rate of neonatal complications of lithium (
20,
21).
We attempted to reduce the incidence of polypharmacy by recommending mood stabilization with a single medication. Further, we advised against the use of valproate during the peripartum period because of high teratogenic risks during pregnancy (
22) and the lack of efficacy for postpartum prophylaxis shown in a single study (
23). However, given the potential risks of switching medications, our treatment plan discussion always included carbamazepine, lamotrigine, and antipsychotics as important considerations, if patients were clinically stable while taking these medications and had manageable side effects or if they had a history of a favorable response to these medications. It is important to note that the final decision regarding prophylaxis during pregnancy was always made by the patient, following a collaborative discussion to consider the risks and benefits of each pharmacologic treatment option, including the potential for teratogenicity and the risk of relapse.
In the women receiving maintenance lithium treatment, we prescribed doses three times a day during pregnancy to avoid peak lithium levels. After delivery, we reduced the number of doses to one per day (with a target minimum plasma level postpartum of 0.8 mmol/L). High-risk women who were medication free at the time of evaluation were advised to start lithium prophylaxis immediately postpartum. For these women, lithium was started the first evening after delivery and given once daily according to the plasma level (target minimum, 0.8 mmol/L). Plasma lithium levels were monitored twice weekly during the first week postpartum, once per week during weeks 2 and 3, and thereafter as clinically indicated. Lithium levels were individualized according to clinical symptoms and side effects, incorporating the preferences of each patient and her previous history, if any, of lithium therapy.
We particularly emphasized the importance of sufficient sleep during the peripartum period, as sleep loss has been demonstrated to be a modifiable risk factor in bipolar disorder and postpartum psychosis (
24–
26). Accordingly, all women were advised to spend the first week postpartum in a private room on the inpatient obstetric ward, where nurses performed the overnight newborn feedings to provide mothers with the opportunity to sleep throughout the night. In addition, we recommended standardized treatment with a benzodiazepine (lorazepam, 1 mg at bedtime) during the first week postpartum, during which subjective self-reports of sleep quality were collected daily through clinical interviews. Further, the women were advised against breast-feeding given the current uncertainty regarding breast-feeding during maternal lithium treatment (
21,
27).
In summary, a comprehensive individualized perinatal treatment plan was created on the basis of the choices of each woman in collaboration with her clinician regarding the risks and benefits of each treatment option, including prophylaxis, breast-feeding, sleep hygiene, and postpartum inpatient obstetric care. All women received follow-up evaluations every 4–6 weeks throughout the peripartum period. We defined the postpartum period according to the DSM-IV definition of the first 4 weeks postpartum. Therefore, we followed all women for a minimum of 4 weeks postpartum. The mean period of follow-up was 12.6 weeks postpartum (range=4–52 weeks).
Each patient and her partner were encouraged to immediately contact her psychiatrist in case of affective instability, psychotic symptoms, or refractory insomnia. We defined relapse as the occurrence of any psychiatric episode fulfilling the DSM-IV criteria, including hypomanic episodes. During the first week postpartum, all patients were screened daily for prodromal symptoms by a perinatal psychiatric nurse (J.V.) in order to provide the earliest possible intervention.
Statistical Analysis
All analyses were performed by using SAS, version 9 (SAS Institute, Cary, N.C.). For characteristics of the study group, categorical data were evaluated by means of Fisher's exact test and continuous variables were examined with two-sample t tests. Categorical outcomes related to relapse risk were examined by using both Fisher's exact test and odds ratios with corresponding 95% confidence intervals (CIs). All hypotheses were tested with an alpha of 0.05 (two-sided).
Results
Table 1 shows demographic, obstetric, and psychiatric characteristics for the enrolled patients. No significant differences were found in age, education, marital status, unplanned pregnancy, smoking during pregnancy, or the frequency of cesarean section.
Peripartum Relapse in Bipolar Disorder and Postpartum Psychosis Only
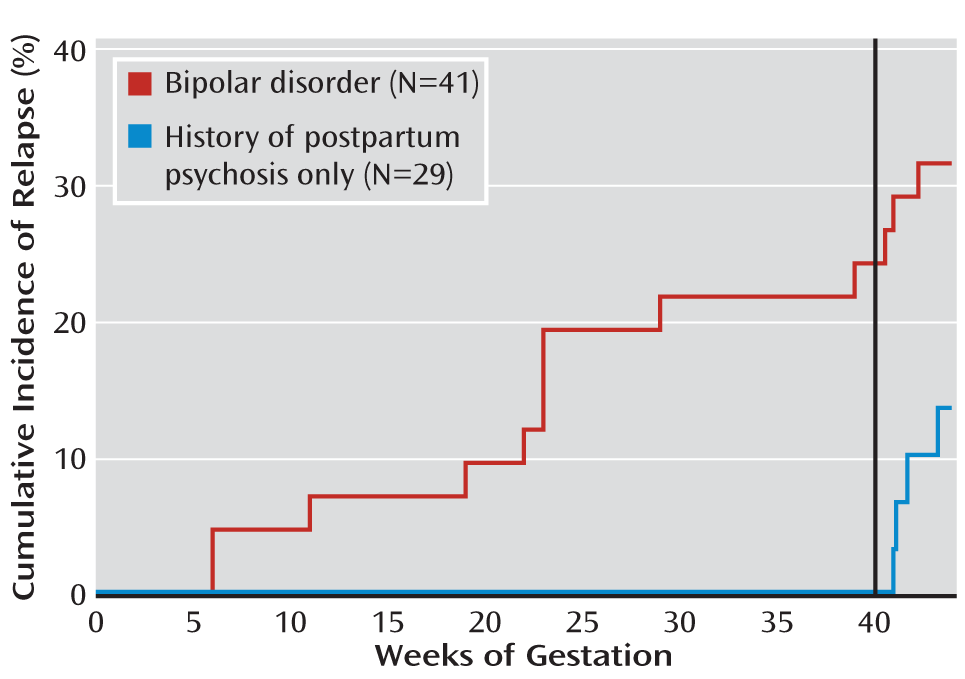
The timing of relapse was substantially different between the women with bipolar disorder and those with postpartum psychosis only (
Figure 2). Remarkably, despite being medication free throughout the entire pregnancy, none of the 29 women with postpartum psychosis relapsed during pregnancy. Postpartum, four of the 29 (13.8%) relapsed (
Table 2). Of these four women with previous postpartum psychosis, the current relapse was manifested as mania for one woman, psychosis for one, a mixed episode for one, and depression for one. Three of these four women required postpartum inpatient admission.
In contrast to the women with a history of postpartum psychosis only, none of whom had a relapse during pregnancy, 24.4% of the women with bipolar disorder (10 of 41) relapsed during pregnancy (p<0.01, Fisher's exact test) (
Table 2). Of these 10 women, five had a manic episode, two had a mixed episode, two had a major depressive episode, and one developed hypomania. Those with a manic or mixed episode all required hospitalization. Relapse postpartum occurred in 22.0% of the women with bipolar disorder (nine of 41), the majority of whom (six of nine) had also previously relapsed during pregnancy. Three out of these six women achieved full remission after the relapse during pregnancy but relapsed again postpartum. The other three women experienced a postpartum worsening of an episode beginning in pregnancy (
Table 2). Consequently, relapse during pregnancy was a significant risk factor for relapse postpartum (p<0.01, Fisher's exact test; odds ratio=14.0, 95% CI=2.5–80.0). Of all nine women with bipolar disorder and postpartum relapse, three had a manic episode, one had a mixed episode, three had depression, and two had hypomania. Overall, six bipolar women required postpartum inpatient admission (
Table 2).
Relapse in the bipolar women, both during pregnancy and postpartum, was especially common in women with a history of puerperal episodes (
Table 2). Eight women with bipolar disorder reported a history of both puerperal and nonpuerperal episodes, of whom 50.0% (four of eight) had a peripartum relapse. In contrast, the peripartum relapse rate was 27.3% in the women with bipolar disorder with a history of only nonpuerperal episodes (nine of 33).
Influence of Prophylactic Medication in Women With Postpartum Psychosis Only
All 29 women with postpartum psychosis only were medication free during pregnancy. During this time, none of these women had symptoms of relapse, including any manic, psychotic, or depressive episodes (
Table 3).
Of the 29 patients with a history of postpartum psychosis only, 20 began prophylactic treatment within 24 hours of delivery. Of these 20, 17 used lithium and three used antipsychotics. Notably, there were no cases of relapse among the women with postpartum psychosis who initiated postpartum prophylaxis upon delivery. Nine of the 29 patients decided against prophylactic medication, with the majority citing their intention to breast-feed. The relapse rate in the women without postpartum prophylaxis and a history of postpartum psychosis was 44.4% (four of nine). The difference in relapse rates between the patients with and without prophylaxis was significant (p<0.01, Fisher's exact test). No differences were found in demographic variables between these two groups.
One woman had two deliveries during the study inclusion period. She was medication free throughout the first of these pregnancies, used lithium for postpartum prophylaxis, and remained clinically stable throughout the entire peripartum period. During the second pregnancy, she was medication free and clinically stable throughout pregnancy. Unfortunately, however, she relapsed without postpartum prophylaxis.
Influence of Prophylactic Medication in Women With Bipolar Disorder
Of the 41 women with bipolar disorder, 31 (75.6%) received maintenance prophylaxis during pregnancy: 27 women used lithium monotherapy for mood stabilization, two women used lithium plus an antidepressant, one woman used lithium plus an antipsychotic, and one woman used haloperidol monotherapy as prophylaxis. Ten (24.4%) of the 41 bipolar women did not use prophylaxis continuously throughout pregnancy: three discontinued prophylaxis during the first trimester and seven were without prophylaxis during the entire pregnancy. No significant differences in demographic or baseline clinical characteristics were observed between the women with bipolar disorder who received prophylaxis and those who did not.
The relapse rate during the pregnancies of the women with bipolar disorder who used prophylaxis was 19.4% (six of 31), compared to 40.0% (four of 10) in women without prophylaxis. Relapse during pregnancy was treated as clinically necessary, after which mood stabilization was continued throughout pregnancy and the postpartum period. However, despite maintenance mood stabilization, 60.0% (six of 10) of the women who relapsed during pregnancy also experienced a postpartum relapse (p<0.01, Fisher's exact test; odds ratio=14.0, 95% CI=2.5–80.0).
Among the women with bipolar disorder who remained stable throughout pregnancy, 83.9% (26 of 31) used prophylaxis postpartum. Of these women, only 7.7% (two of 26) relapsed postpartum. Further, five of the 31 women who were stable throughout pregnancy declined prophylaxis postpartum, of whom one woman (20.0%) relapsed.
Five bipolar women had two deliveries each during the study inclusion period. Three women declined prophylaxis during both of their pregnancies: two of them were stable during both pregnancies, while the third woman relapsed during both pregnancies. Two women used lithium prophylaxis and were stable during both pregnancies: one woman used lithium continuously during both pregnancies, whereas the other woman used lithium prophylaxis postpartum after her first pregnancy and continuous prophylaxis during her second pregnancy.
Discussion
A major goal of peripartum psychiatric care is the development of an effective prophylaxis algorithm that optimally balances the risks and benefits for the mother and fetus (
28–
30). With this goal in mind, we designed a peripartum prevention program using the best available evidence for pregnant women with the two strongest risk factors for postpartum psychosis: a previous postpartum psychosis and/or a history of bipolar disorder. Overall, we confirmed that lithium is highly efficacious for peripartum prophylaxis. However, women with a history of postpartum psychosis only, compared to those with bipolar disorder, had substantial differences in their clinical outcomes and prophylaxis requirements.
First, all women with a history of psychosis limited to the postpartum period were stable throughout their entire pregnancy, despite using no prophylactic medication. In contrast, women with bipolar disorder had high rates of relapse during pregnancy. Second, initiation of prophylaxis with either lithium or an antipsychotic immediately postpartum in women with a history of postpartum psychosis was highly effective for preventing postpartum relapse. In contrast, the efficacy of postpartum prophylaxis in women with bipolar disorder was much lower. Together, our findings suggest that postpartum prophylaxis is highly efficacious in women at high risk for postpartum psychosis who do not have a diagnosis of bipolar disorder. Moreover, these findings suggest that in striking contrast to women with bipolar disorder, women with a history of postpartum psychosis but without manic or psychotic symptoms outside the postpartum period may not require prophylaxis during pregnancy, thereby offering a substantial risk reduction by entirely avoiding fetal exposure to medications.
Our findings support a wide literature demonstrating that women with bipolar disorder have a substantial risk of relapse during pregnancy as well as in the postpartum period (
31–
33). In contrast, women with a history of only postpartum psychosis have a vulnerability for mania or psychosis that is restricted to the postpartum period. Therefore, our data contribute to the emerging consensus that women with a history of psychosis limited to the postpartum period might have a distinct variant of bipolar disorder. Accordingly, we have described elsewhere the postpartum-onset psychosis and distinctive phenomenology in this group (
34). Therefore, it will be interesting to explore the neurobiological mechanisms that are most highly sensitized in the postpartum period and responsible for this restricted window of vulnerability to psychosis.
It is important to note that the bipolar women who were unstable during pregnancy showed the highest rates of postpartum relapse. In particular, we observed that prophylaxis during pregnancy in bipolar women is important not only to maintain mood stability during pregnancy but also to prevent episodes postpartum. However, the benefits of continuous lithium use for affective stability in the mother, both during pregnancy and postpartum, must be carefully weighed against the teratogenic effects of lithium during early pregnancy and the elevated rate of neonatal complications (
4,
20,
21). Further, the benefits of postpartum prophylactic treatment with lithium must be considered in light of the relative risk to infants of breast-feeding exposure versus the loss of the benefits of breast-feeding.
This study has some limitations. We likely missed symptoms associated with transient instability, as our study was principally designed to detect mood episodes fulfilling DSM-IV criteria. Further, our study was naturalistic, leaving open the possibility that some of the outcomes were influenced by patients' preferences. Conversely, a naturalistic study design more likely reflects the scenarios confronting women and their perinatal health care providers.
Our primary pharmacologic treatment recommendation for high-risk women was lithium, based on the literature. In contrast, studies using other prophylactic postpartum treatment strategies in bipolar women either failed to show efficacy, as in the case of estrogen administration (
35,
36) and valproate (
23), or were inconclusive, as in the case of olanzapine (
37). Notably, the relapse rates in the bipolar women receiving lithium prophylaxis in our study were consistent with those in previous reports (
9–
12). To our knowledge, no previous prophylaxis studies have independently examined women with postpartum psychosis limited to the postpartum period. Clearly, more studies are required to compare the efficacy of other potential prophylactic treatment options (e.g., antipsychotics, carbamazepine) with that of lithium, as well as their relative efficacy for prophylaxis in bipolar women and those with a history of psychosis limited to the postpartum period.
In conclusion, our study demonstrates a strong overall benefit of prophylaxis for the prevention of postpartum psychosis in high-risk women. Further, we have identified a clinically relevant algorithm that may prove useful in determining prophylaxis requirements. In bipolar women, prophylaxis during pregnancy appears critically important for maintaining mood stability during pregnancy and for minimizing the high risk of postpartum relapse. In contrast, our findings suggest that women with a history of psychosis limited to the postpartum period should initiate prophylaxis immediately postpartum but remain medication free throughout pregnancy. Accordingly, this treatment algorithm may help reduce the fetal risk that can accompany in utero exposure to medications without compromising the efficacy of postpartum prophylaxis.
Acknowledgments
The authors thank Annemarie van Hulst, M.D., Jean-Luc Klompenhouwer, M.D., Ph.D., Monique Raats, M.D., Mijke Lambregtse-van den Berg, M.D., Ph.D., and Tom Schneider, M.D., for clinical assistance in the Peripartum Prevention Program.