A well-replicated finding in developmental psychopathology is that early-starting, chronic conduct-problem young children are at high risk to grow into antisocial adults (
1), variously labeled as suffering from externalizing psychopathology (
2), chronic criminals (
3), having antisocial personality disorder (
4), “psychopaths” (
5), or “super-predators” (
6). They are also at risk for internalizing psychopathology, substance abuse, risky sexual behavior (
7), harsh parenting of offspring (
7), and poor health and well-being (
1,
3,
4). These individuals cost society between $2.6 and $5.3 million in each of the following areas: incarceration, adjudication, treatment, and victims’ costs (
8). Although intervention evaluations document short-term positive effects on reducing children’s antisocial behavior, no intervention program, to our knowledge, has ever reported effects for kindergarten-age children with early conduct problems (“early starters”) that last into adulthood, leading some to doubt whether prevention is possible (
9) and to advocate for incarceration (
10) and defunding of prevention programs (
11). In contrast, we hypothesized that, and examined whether, adult maladjustment outcomes can be prevented with concerted intervention, in the largest National Institutes of Health-funded randomized controlled trial to date to prevent adult psychopathology and crime and improve well-being by intervening among 6-year-old early-starter children.
Developmental science models (
7,
12) identify factors in home and school environments that deter antisocial development. Technologies have been developed to improve single components associated with antisocial development outcome, including consistent and nonharsh parenting (
13), social-cognitive skills (
14), positive peer relationships (
15), academic skills (
16), and a nondeviant-peer social ecology (
17). These single-component interventions have shown short-term efficacy in reducing aggressive behaviors; however, effects typically fade, possibly because the syndrome is multifactorially determined and cascades across development if all facets are not addressed (
18). Because these interventions aim to build general skills that children can carry with them throughout life, they have also been employed to prevent substance abuse, internalizing, crime, and risky sexual behavior outcomes and improve general well-being (
7,
9,
15,
17), all of which are correlated with externalizing problems.
The Fast Track prevention program began in 1991 to test the hypothesis that comprehensive intervention that addresses multiple components of antisocial development and is implemented continuously with early starters and their families across 10 years of childhood (1st grade through 10th grade) will have an enduring impact on adult psychopathology. The program blended parent behavior-management training, child social-cognitive skills training, peer coaching and mentoring, academic skills tutoring, and classroom social-ecology change, at a cost of $58,000 per child over 10 years. Program impact was tested in a randomized controlled trial that included 12 “mini-replications” in four geographic sites across three cohorts of children screened at age 5 to be early starters in conduct problems.
Intent-to-treat analyses to date indicate that the intervention was successful in promoting its proximal goals of improving parenting behavior, social-cognitive skills, peer relationships, academic skills, and classroom social ecology (
19–
21). It reduced 1) aggressive behavior throughout elementary school as reported by parents, teachers, peers, and blinded observers (
19–
21), 2) self-reported delinquent behaviors in high school (
22), and 3) juvenile (
23) and adult (unpublished data, Conduct Problems Prevention Research Group, 2012) arrests as indicated by administrative records through age 21. Impact at grade 8 was negligible (
24), and some outcomes yielded impact only for subgroups (
22).
The present study assessed outcomes at age 25—a full 8 years after the program had ended—through administrative record review and psychiatric interviews with participants and peer reporters who provided independent perspectives unbiased by program participation. We focused on eight domains that index adult functioning: externalizing psychopathology, internalizing psychopathology, substance abuse, criminal conviction, risky sexual behavior, aggression toward partners and offspring, education/employment, and general well-being. We hypothesized that, compared with control subjects, early starters who had been randomly assigned to intervention at age 6 would display a lower prevalence rate of problems in any of the three psychopathology domains (externalizing, substance abuse, and internalizing problems), fewer criminal convictions, less risky sexual behavior, less aggressive romantic and offspring relationships, better education and employment, and higher general well-being scores.
We also tested intervention efficacy in subgroups of early starters. Some models suggest that psychosocial intervention might be efficacious with moderately high-risk children but will not penetrate the highest-risk subgroup, which, presumably, is impervious to external control. Contrary to that notion, in the Fast Track trial thus far, intervention effects have been stronger among the highest-risk group than the moderate-risk group at ages 9, 12, 15, and 18 (
22,
25). However, by age 21, adult arrest records revealed similar positive impact for both the highest- and moderate-risk groups. Finally, we hypothesized robust intervention efficacy across gender, ethnicity, and urbanicity groups.
Method
Participants
Children were selected from each of three kindergarten cohorts (from 1991–1993) at each of four geographic sites: Durham, N.C.; Nashville, Tenn.; rural Pennsylvania; and Seattle. Elementary schools (N=55) in neighborhoods with high rates of crime and economic disadvantage were divided into paired sets (one to three sets per site) matched for demographic characteristics, and one set was randomly assigned to intervention and one to a control.
A multiple-gating screening procedure (
26) that combined teacher and parent ratings of aggressive, disruptive behavior was applied to all 9,594 kindergarteners (the CONSORT diagram is presented in the
data supplement accompanying the online version of this article). The first gate employed teacher-reported classroom conduct problems, using the Teacher Observation of Child Adjustment-Revised Authority Acceptance score (
27). Children scoring in the highest 40% within cohort and site were solicited for the second gate of screening: parent-rated home behavior problems, using a 22-item instrument based on the Child Behavior Checklist (
28). Teacher and parent scores were standardized within site and summed to yield a severity-of-risk screen score.
Children were selected based on this risk score, moving from the highest down until desired sample sizes were reached within sites, cohorts, and conditions. A total of 979 children (10% of the total) were solicited to yield a sample of 891 participating children (91% consent; intervention group, N=445; control group, N=446). At the time of selection, the participant mean age was 6.58 years (SD=0.48). Ethnicity varied (African American, 51%; European American, 47%; other ethnicity, 2%), and 69% were boys. The mean externalizing problem score for the teacher-reported Child Behavior Checklist (
29) was 1.6 standard deviations above the national mean. Fifty-eight percent of children had single parents; 29% of parents had not completed high school; and 35% of families were in the lowest socioeconomic class.
Written, informed consent from parents and oral assent from children were obtained. Parents were paid for completing interviews, and intervention group parents were paid for group attendance. All procedures were approved by the institutional review boards of participating universities.
To improve the precision of model estimates, 22 variables were measured prior to intervention and included as covariates in outcome analyses (plus cohort and site). These variables are presented in
Table 1 and described elsewhere (
www.fasttrackproject.org). Previous analyses confirm no robust statistical differences in these scores between intervention and control groups (
19,
21,
22).
At the age-25 follow-up, participants were solicited for interview and asked to nominate a peer who knew them well and could complete a confidential interview about them. A total of 702 participants (81% of those living) and 535 peers (for 76% of participants; net, 62% of the total) provided data. Participation did not differ significantly by condition (control group, N=352 [78.9%]; intervention group, N=350 [78.7%]). As indicated in
Table 1, two of the 22 preintervention variables differed significantly (p<0.05) between interviewed and noninterviewed participants. One variable significantly differentiated participants with a peer reporter from those without a peer reporter. Among interviewed participants, the intervention and control groups differed significantly on three variables. Among participants with peer reporters, the intervention and control groups differed significantly on one variable. Given that there were only seven significant differences among 88 tests, we concluded that attrition did not systematically alter the representativeness of the samples.
Intervention Procedures
Elementary school phase (grades 1–5).
During grades 1–5, intervention families were offered group intervention during a 2-hour “enrichment program” that included children’s social skill “friendship groups” (
30), parent training groups (
31), guided parent-child interaction sessions (
31), and paraprofessional tutoring in reading (
30). Tutors provided three additional 30-minute sessions per week in reading and peer pairing to improve friendships with classmates. Teacher consultation and the teacher-implemented social-cognitive skill development Fast Track PATHS (Promoting Alternative Thinking Strategies) curriculum (
32) were implemented universally in grade 1–5 classrooms in intervention schools (except in Durham, N.C., where it was prohibited) to promote social-emotional competence. Enrichment programs were held weekly during grade 1, biweekly during grade 2, and monthly during grades 3–5. In addition, home visiting (unpublished data, Dodge KA, 1993) helped parents generalize their skill learning and address individual needs. After grade 1, criterion-referenced assessments adjusted the prescribed dosage to match need.
Middle and early high school phase (grades 6–10).
During grades 5 and 6, children received a middle school transition program, and there were four parent-youth groups on topics of adolescent development; alcohol, tobacco, and drugs; and decision making. In grades 7 and 8, eight youth forums (
33) addressed vocational opportunities, life skills, and summer employment opportunities. In grades 7–10, individualized interventions (
33) addressed parent monitoring, peer affiliation, academic achievement, and social cognition. All children received Oyserman’s School-to-Jobs possible-selves intervention (
33) aimed at examining emerging identity.
Intervention participation.
Ninety-six percent of parents and 98% of children attended at least one group session during grade 1. Of these families, 79% of parents and 90% of children attended at least 50% of prescribed group sessions (
34). Participation decreased modestly across years, primarily because of residential moves. In grades 7–10, intervention continued with at least 80% of all children.
High intervention fidelity was ensured by manualization, regular cross-site training, and weekly clinical supervision. Outside interventions were neither encouraged nor discouraged.
Age-25 Administrative Records
Court records were collected locally and supplemented using a national database that included all arrests, adjudications, diversions, and magistrate appearances, based on full name, birthdate, and social security number (N=817, 92%). We limited offenses to convictions and diversions. Following previous coding systems (
23,
35), we created severity-weighted indices, multiplying frequencies by severity across all lifetime convictions. For violent crimes, severity levels range from 1 to 3 (severity 3 includes aggravated/armed robbery, murder, rape, kidnapping, sex offenses, and first-degree assault; severity 2 includes robbery and first-degree burglary; and severity 1 includes DUI and carrying a concealed weapon). Severity levels for substance crimes range from 1 to 2 (severity 2 includes manufacturing and possession with intent to sell; severity 1 includes possession). Severity levels for property/public order crimes range from 1 to 3.
Age-25 Interviews
Condition-blinded adults were trained to interview participants in person (with telephone backup). Each participant was invited to nominate a peer for an independent interview about him- or herself, conducted in person in a private session. Participants were paid $100 for the interview and $25 for nominating a peer, and peers were paid $50.
The Adult Self-Report (
36) is a 132-item instrument of psychiatric symptoms with response options of “not true,” “somewhat or sometimes true,” and “often true.” The instrument author’s aggregate externalizing t score and internalizing t score (based on national norms within gender; mean score=50 [SD=10]) were computed. Using criteria recommended by an international panel of judges that were consistent with DSM-IV criteria (
4), indicators (0=no, 1=yes) were computed for antisocial personality, attention deficit hyperactivity disorder (ADHD), avoidant personality, somatic problems, anxiety, and depression disorders. Two measures of well-being were computed: personal strength from the instrument author’s scoring algorithms and a new 16-item score capturing happiness (alpha=0.85).
The Adult Behavior Checklist–Friend (
36), a 132-item peer version of the Adult Self-Report, was administered to the peer respondent, yielding the same scores.
The Tobacco, Alcohol, and Drugs survey–version 3, is a 57-item open-ended and forced-choice instrument based on measures from the National Longitudinal Study of Adolescent Health (
37) to assess frequency and problem level for tobacco, alcohol, and illegal drug use. We created three dichotomous indicators: 1) binge drinking problem (defined as five or more drinks on one or more occasion in the last month and five or more drinks on 12 or more occasions in the last year); 2) heavy marijuana use (defined as 27 or more days of use in the past month); and 3) serious substance use (defined as use of cocaine, crack, inhalants, heroin, LSD, phencyclidine, ecstasy, mushrooms, speed, or other pills not prescribed by a physician in the past month). An alcohol and drug module, adapted from the National Institute of Mental Health Diagnostic Interview Schedule (
38), was administered. DSM-IV diagnostic criteria for alcohol abuse were applied to create a diagnostic indicator. We also created an any substance use problem indicator, scored 1 if any of the four substance use problems were met, or 0 otherwise. The Tobacco, Alcohol, and Drugs survey (Friend) and Alcohol and Drug Module (Friend) are identical peer-report instruments, yielding the same scores.
We created an any externalizing, internalizing, or substance use problem indicator, scored 1 if criteria for any of the following problems were present, or 0 otherwise: antisocial personality, ADHD, avoidant personality, somatic problems, anxiety, depression, alcohol abuse, binge drinking problem, heavy marijuana use, or serious substance use.
The 36-item Short-Form Health Survey (
39) was administered to participants and peers. A general health index averaged four items capturing overall health status, presence of chronic conditions, magnitude of bodily pain, and presence of physical health issues that infringed upon work. For self- and peer-reported data, we constructed an overall well-being score by averaging across the standardized general health index, personal strength, and happiness scores.
Two scores (0=no, 1=yes) were created from the 8-item Education Information and the 46-item Employment History measures from the National Longitudinal Surveys (
40) to ascertain whether the respondent graduated from high school or received a GED and was currently employed full-time or enrolled in higher education.
Respondents completed the 37-item Overview of Sexual Experiences (
41). The number of lifetime partners item captured risky sexual behavior over the respondent’s lifetime (categories ranged from 0 to 7 capturing 0, 1–2, 3–5, 6–10, 11–15, 16–20, 21–50, and 50 or more partners). For risky sexual behavior in the past 12 months, the number of partners in the last year was multiplied by the sum of two scales: new-partner condom nonuse and regular-partner condom nonuse. New-partner condom nonuse ranged from 0 to 5 (no new partner, always use condom, most times use condom, about half the time, sometimes nonuse, and never use, respectively); condom nonuse with the respondent’s regular partner ranged from 1 to 5 (never nonuse, most times use condom, about half the time, sometimes nonuse, and never use, respectively).
The 47-item General Violence Questionnaire (
42) measured violence between the respondent and his or her romantic partners. The violent acts against romantic partners item summed the number of times in the past 12 months (coded 0, 1, 2, or 3 [indicating three or more times]) the respondent did the following to any romantic partner: threatened with a knife or gun; pushed, shoved, grabbed, slapped, or threw something; punched, hit, kicked, bit, or slammed against a wall; beat up or choked, strangled, burned, or scalded on purpose; or used a knife or gun. Peers completed the same instrument.
The 24-item parenting measure was completed only for participants with offspring and included items from the Being a Parent Scale and Conflict Tactics Scales (
43), completed for the oldest child. Spanking was coded as 1=never, 2=1–3 times, 3=monthly, 4=weekly, and 5=most days. Coercive parenting was averaged across the following five items, each coded as above: threatened; yelled, insulted, or swore at; hit or tried to hit with something; pushed, grabbed, or slapped; and beat up. Parenting efficacy was averaged across six items (1=strongly disagree to 7=strongly agree) capturing the respondent’s belief that he or she possessed the skills to be a good parent. Parenting satisfaction was averaged across six reverse-coded items (1=strongly agree to 7=strongly disagree) capturing the respondent’s belief that being a parent is fulfilling. Peers received an identical version.
Statistical Model and Treatment of Missing Data
For each indicator, a combined score across self- and peer-interviewees equaled 1 if either the respondent or the peer reported that the problem was present, or 0 otherwise. For each continuous scale, we averaged across the self- and peer-reported scales. If the peer-reported scale was not collected or missing, the self-reported scale was used. If more than 20% of the individual scores were missing for any variable, the score was declared missing.
We estimated the impact of intervention on each outcome using full information maximum likelihood to account for data missing at random, with standard linear regression models for continuous outcomes, logit models for dichotomous outcomes, and negative binomial models for count and crime variables. We clustered standard errors by kindergarten school to account for sampling at the school level. Analyses were based on an intent-to-treat design that included all children without regard to intervention participation. We controlled for cohort, site, and 22 preintervention covariates and tested for moderation by gender, race, cohort, site, and initial screen score. For continuous outcomes, we report standardized coefficients indicating the standard deviation change in the outcome associated with assignment to intervention. We report odds ratios and the number needed to treat (
44) for dichotomous outcomes and the percentage change in expected counts for count outcomes (
45).
Power analyses indicated sufficient power (0.80) to detect group differences with an odds ratio ≤0.65, based on a two-tailed test (p<0.05, N=729), and a control group rate of 0.69.
Results
Intervention and control prevalence rates (or group means and standard deviations) for all outcomes are presented in
Table 2, with model findings for intervention effects summarized in
Table 3. All moderation test results are reported in
Table 4 but described here only when effects reversed direction across groups.
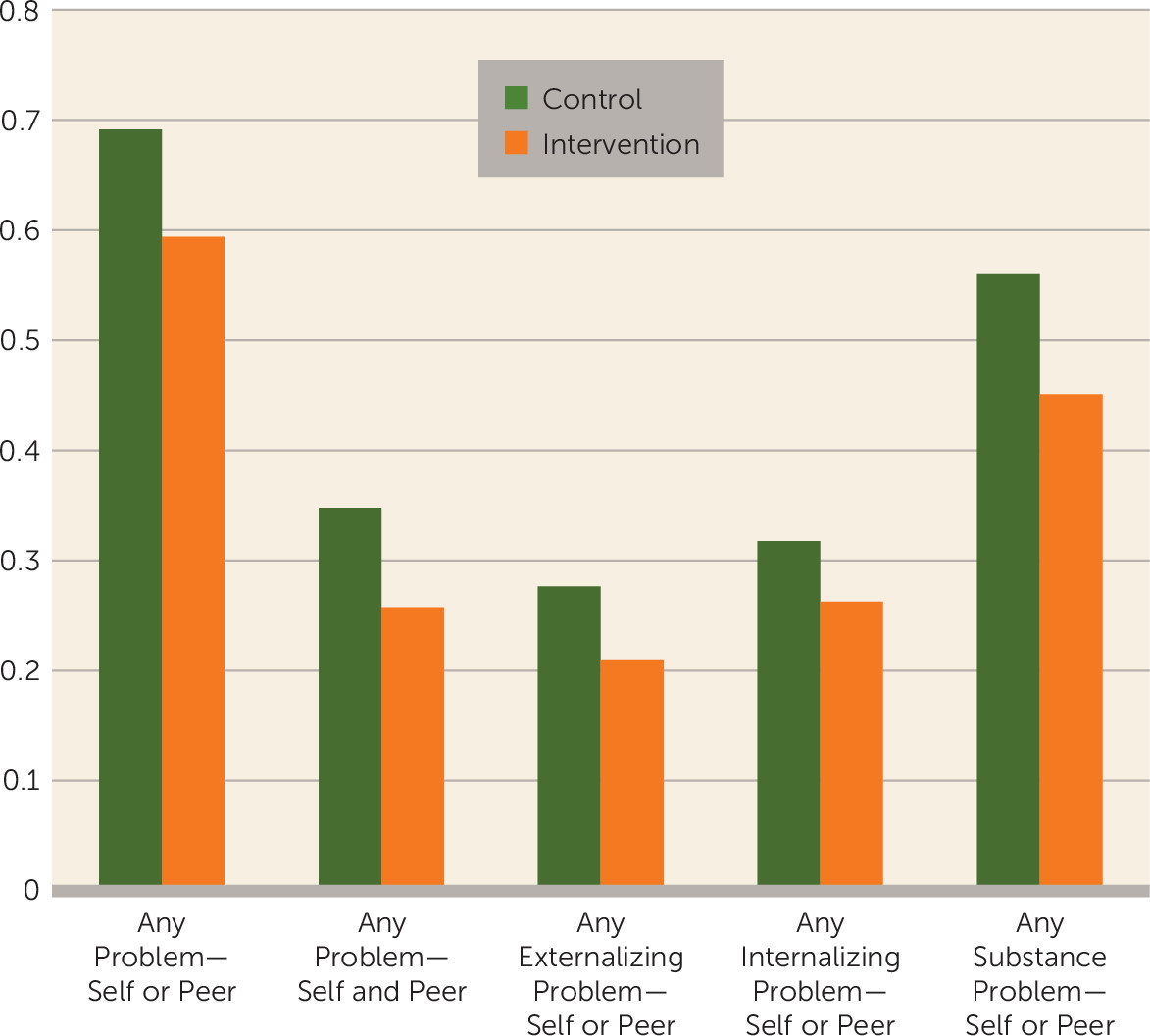
Any Psychiatric Problem
Children assigned to intervention were significantly less likely than children in the control group to exhibit any externalizing, internalizing, or substance use problem (
Figure 1).
Table 5 provides evidence that the intervention-control difference was consistent for each of 13 subgroups, which included the highest-risk group, the moderate-risk group, male participants, female participants, African Americans, European Americans, cohorts 1, 2, and 3, and sites in Durham, N.C., Nashville, Tenn., Seattle, and rural Pennsylvania.
Scores from self-report only, peer-report only, and the use of an “and” rule instead of an “or” rule yielded similar significant effects. Intervention and control rates, respectively, were 0.48 compared with 0.57 for self-report (p<0.02); 0.41 compared with 0.51 for peer-report (p<0.01); and 0.26 compared with 0.35 for combined self- and peer-report (p<0.02).
Externalizing, Internalizing, and Substance Use Problems
Children assigned to intervention had significantly lower externalizing t scores (effect size calculated as Cohen’s d [{intervention mean–control mean}/standard deviation]=0.15); lower internalizing t scores (effect size=0.20); and a significantly lower probability of substance use problems.
Children assigned to intervention had significantly lower probability of meeting criteria for antisocial personality disorder, a marginally significant lower probability of ADHD, and significantly lower probability of avoidant personality. Intervention effects were not significant for somatic problems, anxiety, and depression.
Assignment to intervention significantly decreased the probability of alcohol abuse, marginally decreased binge drinking, did not affect heavy marijuana use, and significantly decreased serious substance use.
Crime
Assignment to intervention significantly decreased the expected severity-weighted violent crime conviction index by 31% and drug conviction index by 35%. Significant moderation of the violent crime index by cohort indicated favorable intervention-control differences in cohorts 1 and 2 but a nonsignificant opposite effect in cohort 3. Intervention did not affect property/public order crime.
Well-Being
Assignment to intervention increased the overall well-being and happiness scores but had no significant effect on general health index and personal strength scores.
Educational Attainment and Employment
Assignment to intervention did not affect the probability of graduating from high school or of being employed full-time or of higher education at age 25.
Sexual Experiences and Aggression in Romantic Relationships
Assignment to intervention decreased the lifetime number of sexual partners (effect size=0.17) and risky sexual behavior in the past 12 months (effect size=0.24). Among participants who maintained a romantic relationship in the past year, the intervention effect on violent acts against romantic partners was not significant.
Parenting
Assignment to intervention significantly decreased spanking of participants’ offspring (effect size=0.22). The effect was significantly moderated by gender, with a stronger effect among male participants than female participants. Intervention had no effect on coercive parenting, marginally increased parenting efficacy (effect size=0.20), and had no effect on parenting satisfaction.
Discussion
We found evidence that early psychosocial intervention can be efficacious in preventing costly adult psychopathology and crime in a group of early-starting conduct-problem children. Nineteen years after identification and 8 years after intervention ended, relative to control subjects, individuals randomly assigned to intervention displayed lower prevalence of externalizing problems, internalizing problems, substance use problems, violent and drug crime convictions, risky sexual behavior, and spanking of participants' offspring, as well as higher well-being. Intervention did not have an impact on education or employment. Previous reports of outcomes in elementary school (
19–
21) and high school (
22,
23) suggest that intervention impact cumulates so that the effect grows in adulthood.
These findings were robust across self- and peer raters and across decision metrics that applied “or” and “and” rules. Using a conservative “and” rule, intervention lowered the prevalence of any problem from 30% to 21%. Clinical interviews with the participant to obtain self-report measures are standard practice and typically accepted as valid (
37), but they can be subject to bias by an intent to please program officials. Because peers had not participated in the intervention at all, they had little reason to bias their responses and thus bring an independent source of validity to the findings.
Fast Track’s efficacy did not differ across diverse subgroups of participants. Twelve “mini-replications” indicated that the direction of intervention effects held for each of the four sites and three cohorts, as well as for both male and female participants, African Americans, European Americans, moderate-risk children, and high-risk children. Of 150 moderation tests, only 10 were significant, and just two indicated nonsignificant reversal of direction for subgroups. These analyses did not test whether the intervention effect was statistically significant within each subgroup because of limited power, but we conclude that this intervention is appropriately targeted toward diverse groups of children.
These findings contribute to our understanding of the developmental antecedents of adult psychopathology. Most models acknowledge the role of biological predispositions, through temperament and still-underidentified genetic factors (
1,
12). Models of development that incorporate the role of environmental experiences with parents, peers, and school have relied largely on correlational evidence subject to selection biases (
11,
12). Even gene-by-environment interaction models utilize environmental evidence that is correlational. The present study contributes experimental evidence about the contribution of environmental experience: random assignment to a psychosocial intervention that attempted to change a child’s environmental experiences did indeed lead to changes in adult psychopathology outcomes. The findings are consistent with a developmental cascade model (
46) in which changes in skills and social experiences early in life cascade into changes in broader outcomes many years later. Future studies will examine mediators of impact on adult outcomes to test developmental models more directly.
Future analyses will evaluate the degree to which the Fast Track intervention is financially cost beneficial. The intervention is a 10-year investment at a cost of $58,000 per child. The present findings indicate a modest reduction by 9 percentage points in prevalence of externalizing, internalizing, and substance problems as a result of intervention. The number of children needed to treat in order to reduce expected outcome “caseness” by one is 8, suggesting that the intervention would be cost beneficial if the cost of a single case of adult psychopathology exceeds $644,444 (calculated as $58,000/0.09). The cost to society of one case of adult psychopathology is not yet known precisely. The cost of chronic criminality has been estimated at up to $5.3 million per case (
7), suggesting that the Fast Track intervention might well yield high dividends and exceed conservative benefit-cost tests. Additional benefits likely accrue from the impact of Fast Track on reducing risky sexual behavior and improving parenting and well-being. The benefit-cost ratio of this intervention should be compared with that of other approaches, such as prenatal home visiting to families selected based on demographic risk (
47). However, even if the Fast Track intervention proves to be cost beneficial, other factors might well make it difficult to implement at scale, including the absolute cost and the length of commitment required by the intervention program.
Future data collection and analyses will monitor other life outcomes. We note that, although not statistically significant, the death rate was 2.5% for the intervention group and 1.6% for the control group, and the incarceration rate was 6.3% for the intervention group and 5.0% for the control group.
One limitation of this study is that the active ingredients of the intervention are not clear. The multicomponent intervention was designed based on a developmental science model that stipulated multiple factors in the development of antisocial behavior. No attempt was made experimentally to deliver partial treatments to determine which components were critical to impact, nor was any attempt made to encourage or block families from receiving outside interventions.
The most important conclusion from this study is that a comprehensive, multicomponent developmental science-based intervention targeted toward early-starting conduct-problem children can significantly reduce adult psychopathology and violent crime. The findings run counter to claims that prevention fails, made by advocates of cuts to federal funding for prevention (
10), which are already only 3% of total health care spending. This finding should encourage policies and programs that acknowledge both the risk and the malleability of early-starting conduct-problem children.
Acknowledgments
The authors thank the Durham Public Schools, the Metropolitan Nashville Public Schools, the Bellefonte Area Schools, the Tyrone Area Schools, the Mifflin County Schools, the Highline Public Schools, and the Seattle Public Schools. The authors also thank the staff members who implemented the project, collected the evaluation data, and assisted with data management and analyses.