Longitudinal studies in adults have shown that bipolar disorder is a lifelong illness manifested by recurrent mood episodes, but the length of asymptomatic periods is highly variable, and some adults with bipolar disorder may have extended periods without recurrences (
1–
4). In fact, Kraepelin, at a time when pharmacological treatments for bipolar disorder were not available, reported cases in which remission lasted for several decades (
4). Contemporary longitudinal studies of adults and youths with bipolar disorder have reported periods of euthymia lasting up to 60% of the follow-up time and rates of complete recovery between 15% and 30% (
1–
9). An analysis of two large epidemiological studies in adults with bipolar disorder (
10), one of which had a single 3-year follow-up, found a lower prevalence of episodes of mania or hypomania in patients whose onset of mood symptoms was during late adolescence or early adulthood, particularly in those diagnosed with a less restrictive bipolar disorder category. These findings were not accounted for by several confounding factors, leading the authors to suggest that there may be a developmentally limited subtype of bipolar disorder.
These studies have helped to advance our understanding of the longitudinal course of bipolar disorder. However, most of the evidence that supports bipolar disorder as a chronic illness has been derived from adults who already had a prolonged duration of illness, potentially biasing the results (
1–
3,
8,
9). Despite these and other potential methodological limitations (e.g., reporting only syndromal and not subsyndromal recurrences, using small samples, and not evaluating the effects of potential confounders), the existing literature and numerous anecdotal cases give us reason to question the notion that every person with bipolar disorder has a lifelong illness with multiple recurrences (
8,
10). This is especially relevant for younger patients, since a diagnosis of bipolar disorder early in life may mean unnecessarily extended exposure to interventions with undesirable potential side effects, time investment, and cost.
Therefore, it is important to evaluate youths with bipolar disorder and follow them prospectively to shed light on the factors that identify patients who have persistent euthymia. Such factors might then be fostered to promote persistent mood stability. In the present study, we sought to identify and evaluate the longitudinal mood trajectories of youths with bipolar disorder, with an emphasis on those who showed persistent euthymia during the follow-up period, and the effects of demographic and clinical variables ascertained at baseline and lifetime family psychiatric history ascertained over the course of the study.
Method
The methods for the Course and Outcome of Bipolar Youth (COBY) study have been described previously (
5). Briefly, the study enrolled 413 youths 7–17 years of age with DSM-IV bipolar I or II disorder or with bipolar disorder not otherwise specified as defined operationally by COBY (
11). Participants were mainly recruited from outpatient clinics (67.6%) at four university centers. The study excluded patients with schizophrenia, mental retardation, autism, and mood disorders secondary to medical conditions or substance use.
At baseline, youths and parents or primary caretakers were interviewed for psychiatric disorders and treatment with the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version (K-SADS-PL) (
12). Severity of mood symptoms was ascertained with the K-SADS Mania Rating Scale (
13) and Depression Rating Scale. Week-by-week longitudinal change in psychiatric symptoms was assessed using the Longitudinal Interval Follow-Up Evaluation and the Psychiatric Status Rating Scales (
14). The Psychiatric Status Rating Scales use numeric values linked to DSM-IV criteria; for mood disorders, scores ≤2 indicate euthymia, scores of 3–4 subsyndromal symptoms, and scores ≥5 syndromal symptoms. The consensus scores obtained after interviewing parents and their children were used for analyses.
Puberty was assessed with the Petersen Pubertal Development Scale (
15). Socioeconomic status was ascertained using the Hollingshead Scale (
16). Current and most severe past global functioning was assessed using the Children’s Global Assessment Scale (
17).
Parents or primary caretakers were evaluated using the Structured Clinical Interview for DSM-IV (
18) and the Global Assessment of Functioning Scale (
19). First- and second-degree family psychiatric history was assessed using the Family History Screen (
20). Family psychiatric history and parental psychiatric treatment analyzed here represent the summary of data collected during the full length of the study. Family functioning was evaluated using the child and parent versions of the Conflict Behavior Questionnaire (
21) and the Family Adaptability and Cohesion Evaluation Scale–II (
22).
Assessments were conducted by research staff trained to reliability on the interviews. Child psychiatrists or psychologists confirmed all diagnoses. The kappa values for psychiatric disorders on the K-SADS were ≥0.8. The intraclass correlation coefficients for the K-SADS Mania Rating Scale, the K-SADS Depression Rating Scale, and syndromal/subsyndromal mood disorders ascertained through the Psychiatric Status Rating Scales were ≥0.75.
Each university’s institutional review board approved the study, and consent or assent was obtained from participating youths and their parents.
Statistical Analysis
First, weekly Psychiatric Status Rating Scale scores were aggregated over 6-month intervals, and the percentage of weeks when participants were euthymic (Psychiatric Status Rating Scale scores ≤2) was calculated for each interval. Second, using latent class growth analysis (
23), youths were clustered into various classes based on their illness trajectories of percentage of time euthymic during each of the 6-month intervals over the follow-up period. Using the SAS Trajectory procedure (TRAJ) (
24), the number of classes was determined by selecting the model with a minimum value of Bayesian information criterion, a minimum of 20 subjects per class, and clinical interpretability of the classes obtained. (For further information regarding the analysis of the latent class analyses, see Table S1 and Figures S1–S8 in the
data supplement that accompanies the online edition of this article. For clinical validation of the latent class analyses, see Figures S9 and S10.) Third, univariate analyses using analyses of variance and chi-square tests were performed to compare the demographic, clinical, and family variables between latent class growth analysis classes. All pairwise analyses were corrected for multiple comparisons using the Bonferroni correction. Fourth, multiple regression analyses incorporating variables with p values <0.10 in the univariate comparisons were conducted using a generalized linear model. Odds ratios and confidence intervals were compared between latent class growth analysis classes for variables that remained significant after the multiple regression. All p values are based on two-tailed tests with alpha set at 0.05.
Results
The latent class growth analysis results are based on the prospective evaluation of 367 youths with bipolar disorder (bipolar I disorder, N=218; bipolar II disorder, N=26; bipolar disorder not otherwise specified, N=123) who had at least 4 years of follow-up assessments and up to 96 months of follow-up (
Table 1). After intake, participants were interviewed a mean of 10.0 times (SD=3.2), on average every 8.7 months (SD=5.2). The mean duration of follow-up was 93 months (SD=8.3), and 80% of participants (N=292) completed all 96 months of follow-up. The mean age at baseline was 12.6 years (SD=3.3); 46.6% of participants were female, 82.6% were Caucasian, 42.0% lived with both biological parents, and the average socioeconomic status score was 3.4 (SD=1.2), or Hollingshead class III, which corresponds to middle class.
Latent Class Growth Analysis
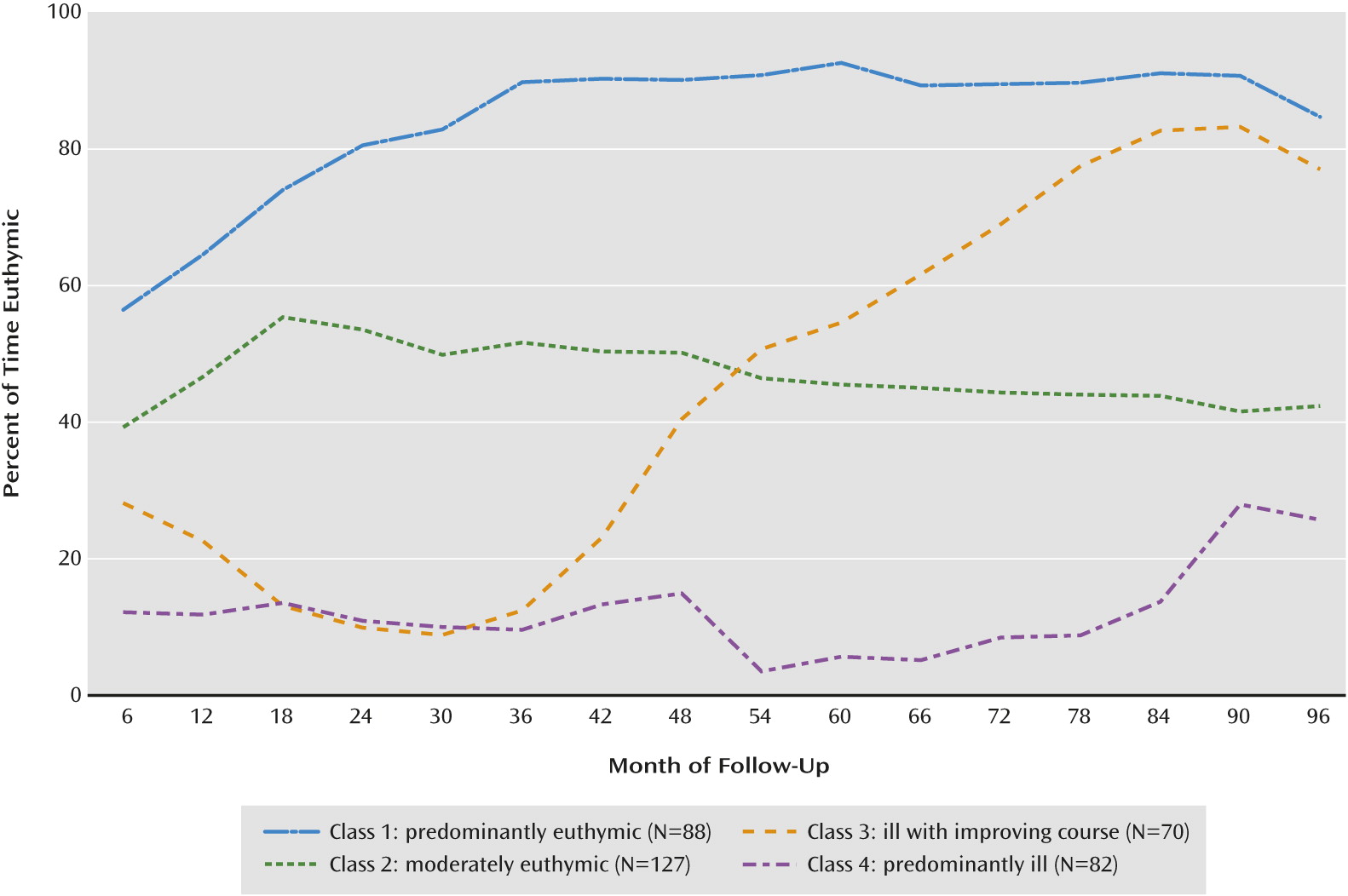
Latent class growth analysis identified four mood trajectory classes based on Psychiatric Status Rating Scale scores ≤2 (Figure 1): class 1, “predominantly euthymic” (N=88; 24.0%); class 2, “moderately euthymic” (N=127; 34.6%); class 3, “ill with improving course” (N=70; 19.1%); and class 4, “predominantly ill” (N=82; 22.3%). Within these classes, youths were euthymic on average 84.4%, 47.3%, 42.8%, and 11.5% of the follow-up time, respectively. As illustrated in Figure 1, youths in classes 1, 3, and 4 showed significant changes in their trajectories toward improvement at 6, 36, and 84 months, respectively (all p values <0.001). As shown in
Table 1, there were no between-class differences in the duration of follow-up or number of interviews. With the exception of the mean highest Psychiatric Status Rating Scale score for mania, youths in class 1 had a significantly higher percentage of time and maximum number of consecutive weeks in euthymia, and regardless of polarity, had a lower percentage of time with syndromal mood symptoms (Psychiatric Status Rating Scale scores ≥5), lower mean Psychiatric Status Rating Scale scores, and lower mean highest Psychiatric Status Rating Scale scores when compared with youths in class 4 (p values <0.001). With the exception of youths in class 3 having significantly more maximum consecutive weeks in euthymia than those in class 2, there were no other differences between these two classes. Also, in general, the Psychiatric Status Rating Scale scores of youths in these two classes were between those of youths in classes 1 and 4.
The variability of the Psychiatric Status Rating Scale scores over the follow-up period was evaluated by comparing the mean standard deviations of Psychiatric Status Rating Scale scores among the four classes. Scores in class 3 had significantly more variability than those in class 2, and scores in both of these classes showed more variability than those in classes 1 and 4 (p values <0.001). There were no variability differences between classes 1 and 4.
Demographic Variables
As shown in
Table 2, youths in class 1 were significantly older than those in classes 3 and 4, had higher socioeconomic status than those in the other three classes, and were more frequently living with both biological parents than those in class 4 (p values <0.03).
Clinical Variables
As shown in
Table 2, youths in class 1 had a significantly higher age at onset of mood symptoms, higher age at onset of first depressive episode, shorter duration of previous mood symptoms, lower depression severity, and lower incidences of suicidal ideation, and comorbid anxiety disorders at baseline. In addition, youths in class 1 had more prospectively ascertained syndromal mood episodes than youths in the other three classes, as shown in
Table 1. At baseline, those in class 1 also were more likely to have had a manic or hypomanic presentation and less likely to have a history of more than one subsyndromal episode than youths in classes 2 and 3; were less likely to have subsyndromal mood symptoms, childhood onset of mood symptoms, and a history of attention deficit hyperactivity disorder (ADHD) than youths in classes 3 and 4; were less likely to have a history of syndromal episodes than youths in class 2; and had lower mania severity than youths in class 3 and higher age at onset of manic episodes than youths in class 4.
Finally, youths in class 1 were less likely to have a baseline history of self-injurious behaviors than those in classes 2 and 4, less likely to have a history of suicide attempt than those in class 2, and less likely to have had physical and sexual abuse than those in classes 2 and 4. Youths in class 2 had a significantly higher age at onset of mood symptoms than those in class 4 and lower mania scores than those in class 3 (p values <0.05). There were no other clinical differences among the four classes, including bipolar disorder subtypes. Youths in all four classes had a history of poor functioning without significant differences among them.
Treatment History
Across all classes, history of exposure to psychiatric services beginning at an early age was common (
Table 3). About half of the sample had a history of at least one inpatient admission, and most had been exposed to several medications, particularly mood stabilizers and antipsychotics. Youths in class 1 were less likely to have been treated with stimulants than those in the other three classes, were older at the time of first outpatient and inpatient treatments than those in classes 3 and 4, and were older and had fewer hospitalizations than those in class 4 (p values <0.03).
Family Psychiatric History, Functioning, and Treatment
Data were available for 701 biological parents, 49.8% of whom were biological mothers. For 327 of them (46.6%), the information was obtained by direct interview, and for 374 of them (53.3%), it was obtained indirectly through the family history. The results of the first- and second-degree family history were combined because separate analyses yielded similar results.
As shown in
Table 4, youths in class 1 were significantly less likely to have a family history of ADHD and suicide attempt than those in the other three classes. They were less likely to have a family history of bipolar disorder, depression, and anxiety disorders than those in classes 2 and 4, and less likely to have a family history of conduct disorder and substance use disorders than those in class 4. Youths in class 2 were less likely to have familial ADHD, conduct disorder, and substance use disorders than those in class 4. Youths in class 1 were less likely to have mothers with depression than those in classes 2 and 4, and less likely to have mothers with bipolar disorder, anxiety disorders, ADHD, or substance use disorders than those in class 4. Youths in class 1 were less likely to have fathers with substance use disorders than those in classes 3 and 4, and less likely to have fathers with bipolar disorder, anxiety, ADHD, or conduct disorder than those in class 4. Finally, youths in class 2 were less likely to have fathers with conduct disorder and substance use disorders than those in class 4.
Overall Functioning in Parents or Primary Caretakers
The parents or primary caretakers of youths in class 1 had significantly higher current, most severe past, and highest past Global Assessment of Functioning scores than those of youths in class 4 (see Table S2 in the online
data supplement). Also, parents or primary caretakers of youths in class 2 had significantly higher current Global Assessment of Functioning scores than those of youths in class 4 (p values ≤0.03).
Parental Psychiatric Treatment
Mother of youths in class 1 were less likely to have a history of treatment than those of youths in classes 3 and 4 and less likely to have had psychiatric hospitalizations than those of youths in class 4 (see Table S2 in the online
data supplement). Mothers of youths in class 2 were less likely to have had hospitalizations than those of youths in class 4, and fathers of youths in class 1 were less likely to have a history of outpatient treatment than those of youths in class 3 (p values <0.04).
Family Functioning and Conflicts
Parents of youths in classes 1 and 2 reported less conflict than parents of those in class 3. There were no other between-class differences in family functioning and conflicts as reported by the parents and youths (see Table S2 in the online
data supplement).
Multivariate Analyses
After multivariate analyses, eight variables were associated as follows with better course: higher age at onset of mood symptoms (χ2=25.57, p=0.001), less lifetime family history of bipolar and substance use disorders (χ2=13.02, p=0.005 and χ2=11.73, p=0.008, respectively), and less history at baseline of severe depression (χ2=9.84, p=0.02) or manic or hypomanic symptoms (χ2=10.46, p=0.02), fewer subsyndromal episodes (χ2=10.36, p=0.02), less history of suicide attempt (χ2=8.05, p=0.05), and less history of sexual abuse (χ2=8.16, p=0.04). Higher socioeconomic status was associated with better illness course, but the association fell short of significance (χ2=7.17, p=0.07). There were also significant interactions between age at onset of mood symptoms and severity of depression and socioeconomic status. The effects of age at onset became nonsignificant in youths with lower socioeconomic status (Hollingshead classes I and II). Also, the effects of depression severity diminished and were nonsignificant in youths with higher socioeconomic status (Hollingshead class V). There were no other significant interactions.
For each of these eight variables, odd ratios were compared among the four trajectory classes (
Table 5). The variables were associated as follows with a greater likelihood of class 1 membership: higher age at onset of mood symptoms and less severe depression compared with classes 2, 3, and 4; fewer subsyndromal episodes compared with classes 2 and 3; less sexual abuse and lifetime family history of bipolar disorder and suicide attempt compared with classes 2 and 4; less severe manic symptoms compared with class 3; and less family substance abuse compared with class 4. Less severe manic symptoms and higher age at onset and less family substance abuse were associated with a greater likelihood of belonging to class 2 compared with classes 3 and 4, respectively. Finally, less family substance abuse was associated with a greater likelihood of belonging to class 3 compared with class 4 (p values ≤0.03).
Discussion
To our knowledge, this is the first study to prospectively characterize long-term mood trajectories in youths with bipolar disorder with an emphasis on patients with a predominantly euthymic course. After approximately 8 years of follow-up, four different mood trajectories were identified. At one extreme, 24.0% of the youths were “predominantly euthymic,” being euthymic 84.4% of the follow-up time (class 1). At the other extreme, 22.3% of the sample was “predominantly ill,” being euthymic only 11.5% of the follow-up time (class 4). Between these two classes, 34.6% of the youths were “moderately euthymic,” being euthymic 47.3% of the follow-up time (class 2), and 19.1% were mostly ill during the first months of the follow-up and then steadily improved (“ill with improving course”), being euthymic on average 42.8% of the follow-up time (class 3). Youths in classes 1 and 4 showed significantly more stable scores on the Psychiatric Status Rating Scales than those in classes 2 and 3.
At baseline, rates of bipolar disorder subtypes and history of poor functioning were similar across all four classes, and all classes (particularly class 4) had high rates of comorbid psychopathology, psychosocial and pharmacological treatments, history of physical or sexual abuse, poor individual and family functioning, and familial psychopathology. Of all these variables, six that were related to the youths and two that were related to the family remained significantly associated with better longitudinal course in the multivariate analyses: higher age at onset of mood symptoms, less severe depression, less severe manic or hypomanic symptoms, fewer subsyndromal episodes, fewer suicide attempts, less history of sexual abuse, and less family history of bipolar disorder or substance use disorders.
Youths with higher socioeconomic status had a better course, but this association did not reach significance. The effect of socioeconomic status was more notable in its role of moderating the effects of age at onset of mood symptoms and severity of depression. The effects of age at onset were not significant in youths with lower socioeconomic status, and there were no effects of depression severity in youths with higher socioeconomic status.
Before discussing these findings, it is important to note the limitations of this study. The data collected through the Longitudinal Interval Follow-Up Evaluation are subject to recall bias. The study included few participants with bipolar II disorder (7%). Also, the generalizability of the observations to other populations remains uncertain because most participants were Caucasian, and they were recruited primarily from outpatient settings. Nevertheless, course and morbidity in non-clinically referred adolescents with bipolar disorder have been shown to be similar to those in referred populations (
25).
The results of this study present a more optimistic perspective on what has been thought to be a universally chronic illness. Although some 22% of the sample was persistently ill, when we combine class 1 (predominantly euthymic) and class 3 (ill with improving course), by the end of follow-up, 43% of the sample was euthymic most of the time. Nevertheless, it is important to note that despite being predominantly euthymic, over 50% of the youths in class 1 continued to experience new syndromal manic or depressive episodes, indicating that they continued to have active, clinically meaningful bipolar symptoms and the need for maintenance treatment. Our results extend the findings of clinically referred studies that followed bipolar youths (
6,
7,
26–
28) and adults (
1–
3,
8,
9). Reports including nonreferred samples of adults (
10) and a small study of adolescents (
25) with bipolar disorder have also suggested that a subgroup of patients may achieve remission over time. However, we cannot directly compare our results with these studies because they did not indicate the prevalence or duration of persistent periods of euthymia.
Youths in class 4 (predominantly ill) had chronic mood symptoms and had significantly higher rates of ADHD and anxiety disorders at baseline than those in class 1, raising the question of whether these youths had other disorders and not bipolar disorder. However, in the multivariate analyses, the effects of the comorbid disorders disappeared, and youths in class 4 had significantly more family history of mania and earlier onset of mood disorders than those in class 1, significantly more prospectively ascertained syndromal mood episodes than the other three classes, and a prevalence of bipolar subtypes and history of exposure to mood stabilizers similar to the other three classes, suggesting that youths in class 4 indeed had a more severe and treatment-resistant bipolar disorder.
Consistent with other studies, early age at onset of mood symptoms was associated with poor longitudinal course (e.g.,
1,
5,
6,
8,
29–
32). We extended these findings by noting that the effects of age at onset were not accounted for by duration of the illness. Thus, early-onset bipolar disorder may be a more severe type of bipolar disorder, or having a mood disorder early in life may interfere with normal psychosocial development and thus set the stage for a more chronic course (e.g.,
1,
5,
6,
8,
29–
32). However, the effects of age at onset were less relevant in youths with lower socioeconomic status, emphasizing the well-documented association between low socioeconomic status and greater psychopathology and worse longitudinal outcome (e.g.,
1,
7,
33,
34).
Several longitudinal studies have also shown that severity of depression, suicide attempt, recurrent subsyndromal mood episodes, and history of sexual abuse are predominant features of bipolar disorder and are associated with poor longitudinal outcome, underscoring the need for successful management and prevention of these factors in bipolar youths (e.g.,
1,
5,
7,
8,
29,
35–
37).
The few studies that have evaluated the effects of family history on the longitudinal course in bipolar adults have also shown that family histories of manic episodes and substance use disorder were associated with poor outcome (
36,
38–
40). There are no reports on the effects of family history on the course of illness in youths with bipolar disorder, but a high-risk study reported that the severity of psychopathology in the offspring of parents with bipolar disorder was related to the number of manic or mixed episodes, but not to depression (
41). The presence of parental bipolar disorder and parental substance use disorder may be a marker for more severe bipolar disorder in offspring, or perhaps these factors are associated with less parental monitoring and poorer family functioning and consequently more severe psychopathology in offspring. In fact, in our sample, parents with substance use disorder had significantly more psychopathology, lower socioeconomic status, and poorer family functioning than parents without substance use disorders (data not shown).
In summary, a substantial proportion of youths with bipolar disorder, especially those whose illness started later in adolescence and who at baseline had less severe depression and manic or hypomanic symptoms, had less history of subsyndromal episodes, suicide attempt, and sexual abuse, and had less lifetime family history of bipolar disorder, are more likely to be euthymic over extended periods. However, these youths, and particularly those in the other classes, continued to present syndromal and subsyndromal mood symptoms, indicating the need to optimize treatment or develop new treatments. In addition to identifying classes that may be amenable to neurobiological research, this line of research also underscores the importance of acknowledging that good outcomes are not uncommon in bipolar disorder.