Markers of social disadvantage, such as lack of health insurance, low income, unemployment, lower educational attainment, and single parenthood, have been linked to higher rates of major depression and anxiety disorders in the general population (
1–
4). Markers of poverty are also associated with more persistent depression (
5–
8). Lack of health care insurance and the low payment rates provided for mental health services by public insurers in many states likely limit access to evidence-based mental health services (
9). Also, the chronic stressors that socially disadvantaged women face, such as lack of transportation, housing problems, and lack of day care services, may be barriers to initiating or continuing mental health care (
1,
7–
9).
Little is known about the impact of women’s health insurance status on the effectiveness of evidence-based depression or anxiety care models and response to treatment. Lack of health insurance or reliance on publicly funded health insurance is often a proxy for socioeconomic disadvantage and greater psychosocial vulnerability. Several research groups have emphasized the need to conduct extensive outreach and patient engagement in order to successfully recruit and maintain low-income minority women who lack health insurance or rely on public insurance in treatment (
10,
11). Two trials have found that the incremental effect of collaborative care compared with usual primary care in improvement in mental health symptoms was as great in low-income patients as in middle- to high-income patients (
12,
13). However, both of these studies also found that low-income patients started with greater mental and physical health impairments and that low-income patients treated with collaborative care had higher levels of psychological distress at 12 months than did middle-income patients treated with collaborative care.
Many women with limited income and limited or no health insurance utilize obstetrics-gynecology (OB/GYN) clinics or women’s clinics affiliated with university or county hospitals as their main source of primary care (
14). However, several studies have found that OB/GYN physicians have less confidence than other primary care physicians in their ability to recognize depression and their skills in treating it (
15). The Depression Attention for Women Now (DAWN) study conducted by our research team found that integrating collaborative depression care in two university-affiliated OB/GYN clinics improved quality of depression care as well as depressive and functional outcomes compared with usual care (
16).
The purpose of the present analysis from the DAWN study (
16) was to determine whether a collaborative depression care program designed to treat women with major depression in OB/GYN settings was as effective in treating socially disadvantaged women with either no health insurance or public coverage (Washington state, Medicaid, or Medicare) as it was in treating women with commercial insurance.
Method
In a randomized controlled trial with blinded assessments, we evaluated the effectiveness of a collaborative depression care program compared with usual care for patients in OB/GYN clinics. Women were randomly assigned either to a 12-month intervention program or to usual care, with blinded assessments at 6, 12, and 18 months. The University of Washington Institutional Review Board approved the study, all participants gave written informed consent, and a data monitoring safety board reviewed initial protocols and safety issues over the course of the trial.
Participants
Participants were recruited from November 2009 through December 2011 at two academic OB/GYN clinics: a university hospital clinic serving women from mixed socioeconomic backgrounds (N=136, of whom 59 [43.4%] were uninsured or insured by public insurers, including Medicaid, Medicare, and the state) and a county hospital serving an underserved, racially diverse population (N=69, of whom 61 (88.4%) were uninsured or insured by public insurers). Both sites were staffed by resident and attending OB/GYN physicians and nurse practitioners.
Patients were screened for depression with the Patient Health Questionnaire–9 (PHQ-9) (
17) while waiting for their physician appointments. Screen-positive women (PHQ-9 score ≥10) were eligible if they met criteria for major depression or dysthymia on a structured psychiatric interview (the Mini International Neuropsychiatric Interview, version 5.0 [
18]), had telephone access, were English speaking, and were at least 18 years of age. Exclusions included substance abuse in the previous 3 months, homelessness, current domestic violence, bipolar disorder or schizophrenia, high suicide risk, two or more suicide attempts, or currently seeing a psychiatrist. Women currently taking an antidepressant or seeing a nonphysician mental health specialist were eligible. All interested, eligible women were scheduled for a baseline assessment, after which the informed consent and randomization procedures were completed.
Randomization
To ensure that the numbers of pregnant women and patients from the two clinics were similar in the intervention and usual-care groups, women were block-randomized by computer off-site (by clinic site, pregnant versus nonpregnant) to the intervention or to usual care. We used blocks with sizes 2 and 4 (alternating randomly) for pregnant women and blocks with sizes 4 and 6 (alternating randomly) for nonpregnant women to ensure balance and to blind the research staff to the pattern of assignment to treatment groups.
Intervention
The collaborative care model designed for the OB/GYN population included an initial engagement session with the care manager (
10), choice of initial treatment (psychotherapy or medication), proactive outreach for patients who did not follow through with appointments, help for uninsured patients with charity care for medications, choice of in-person or telephone visits, and use of social workers as care managers to help alleviate barriers to care. Two depression care managers with master’s degrees in social work who had at least 5 years of experience working with socially disadvantaged populations were hired and provided training on issues related to women’s mental health, such as domestic violence and sexual assault.
Women in the intervention arm received an initial engagement session to elicit health concerns and potential barriers to treatment, provide education about depression, and enhance participation in depression treatment. This engagement intervention has been found to increase participation in psychotherapy in socially disadvantaged minority women (
10). During follow-up sessions, depression care managers obtained a clinical history with a semistructured interview, reviewed educational materials, and elicited patient preferences for either starting with problem-solving therapy (Problem Solving Treatment for Primary Care) (
19,
20) or antidepressant medications. Depression care managers provided help with social interventions such as charity care for medications and financial assistance programs for housing. All women received depression educational materials (
21).
The care managers followed patients in-person and by telephone every 1–2 weeks for up to 12 months. They monitored treatment response at each contact with the PHQ-9 and used a spreadsheet-based tracking system for weekly systematic case review sessions. Medication and behavioral treatment recommendations were made each week at team meetings attended by the care manager, the psychiatrist, and the OB/GYN physician. Physician-recommended medication changes were communicated by the care manager to OB/GYN physicians, who prescribed all medications. Participants were followed until they either reached remission, which was defined as a PHQ-9 score <5, or responded, which was defined as at least a 50% decrease from baseline in depressive symptom severity on the PHQ-9. Once a patient reached one of these goals, she was followed by monthly telephone calls.
Patients who had not responded by 4–8 weeks of treatment received a revised treatment plan based on weekly systematic case reviews. For patients receiving problem-solving therapy, treatment could be augmented with, or switched to, an antidepressant medication. Women on antidepressant medication could receive an increase in dosage, a change of medication, and/or augmentation with problem-solving therapy. Women whose symptoms persisted despite multiple changes in treatments could be referred to mental health specialty care.
Problem-solving therapy has been shown to be as effective as antidepressant medication in treating major depression in several primary care-based trials (
19). The intervention was designed to treat depressive symptoms by helping patients develop skills to alleviate problems and stressors that provoke or maintain depression (
19,
20). The seven key steps in problem-solving therapy are to clarify and define a problem, set a realistic goal, generate multiple possible solutions, evaluate and compare solutions, select a feasible solution, implement that solution, and evaluate the outcome (
19,
20). Antidepressant medications (a selective serotonin reuptake inhibitor was the usual first choice) were chosen based on a clinical algorithm that took into account the patient’s prior treatment experiences with medications. All patients in the intervention arm were counseled regarding increasing positive activities, such as exercise and visiting friends whom they had stopped seeing because of their depression.
Training for care managers included 1 week of instruction in problem-solving therapy and antidepressant medication, use of a standardized depression care management treatment manual (
20), and training in issues specific to women’s health, such as infertility and domestic conflict. Each care manager was required to audiotape an introductory session and at least one problem-solving therapy session with a practice patient before being certified as competent in this treatment model. In addition, for each care manager, the team psychologist (E.L.) reviewed at least one audiotaped session with a study participant, using fidelity rating forms for quality assurance (
20). Feedback on intervention fidelity was also given during weekly supervision to minimize drift from the intervention model.
Enhanced Usual Care
Patients assigned to usual care were informed of their depression diagnosis by the research assistant and received an educational depression pamphlet (
21). All patients had an opportunity for referral to social work and psychiatric consultations. They were asked for consent to notify their provider of their depression diagnosis.
Blinded Outcomes
Data on outcomes were collected at 6, 12, and 18 months by telephone using standardized questionnaires administered by a research assistant blind to intervention status. The Hopkins Symptom Checklist 20-item depression scale (HSCL-20) (
22) was used to measure changes in depressive symptoms over time, including change from baseline to 18 months, as well as percent of participants with at least a 50% decrease in depressive symptom severity from baseline. Each item on the HSCL-20 is rated from 0 to 4 on a Likert scale, and a mean score for the 20 items is computed (range, 0 to 4). This scale has been shown to be as sensitive to change as other commonly used depression scales and to have high reliability and validity (
22–
24). Other outcome measures included the Patient Global Improvement Scale (patient-rated improvement on the Clinical Global Impressions Scale) (
25) and satisfaction with depression care (
26). The Patient Global Improvement Scale has patients rate their change in depression on a 7-item scale (“very much worse” to “very much improved”) and has been shown to have high reliability and validity (
25). Satisfaction with treatment was rated on a 7-item scale ranging from “very dissatisfied” to “very satisfied” that has been extensively used in primary care depression trials (
26,
27). Quality of mental health care was assessed with standardized questions about medication use at baseline and each follow-up assessment, and counseling frequency in each 6-month period (
26,
27).
Insurance Status
Data on insurance status was collected from the medical record at baseline. Categories included no insurance, Washington state coverage, Medicare, Medicaid, and commercial insurance. Women were then grouped into two categories: commercial insurance or no insurance/public coverage.
Demographic and Mental Health Comorbidity Variables
Demographic information collected at baseline included age, education level, marital status, and race/ethnicity. Variables potentially linked to insurance status included measures assessing posttraumatic stress disorder (PTSD), dysthymia, panic disorder, social support, and medical comorbidity. PTSD was measured using the 17-item PTSD Checklist–Civilian Version (
28). A positive screen for PTSD was defined as a score ≥45 on this measure; it has the highest sensitivity and specificity for a diagnosis of PTSD based on structured psychiatric interview (
28). Dysthymia and panic disorder were diagnosed with modules from a structured psychiatric interview (the Mini International Neuropsychiatric Interview, version 5.0). Four items from the Medical Outcome Study’s Social Support Survey were used to assess quality of social support (
29). The medical comorbidity scale from the Medical Outcomes Study was used to measure medical comorbidity (
30).
Statistical Analysis
We used independent t tests and chi-square analyses to compare the baseline characteristics of women in the no-insurance/public-coverage group to those in the commercial insurance group. To evaluate quality of depression care in the intervention arm, we compared the number of in-person and telephone visits by insurance group using data from the registry maintained by the depression care managers. Because visits and telephone calls are count data, we used Poisson regression models to examine differences in the intervention arm by insurance group.
For the primary analysis, generalized estimating equations were used to determine whether insurance status had an effect on the pattern of changes in depression symptoms between intervention groups over time. Generalized estimating equations are intent-to-treat longitudinal regression models that allow for the inclusion of all participants in the analyses, regardless of missing outcomes. We employed an unstructured covariance model. Using HSCL-20 depression scores as the outcome measure at baseline and at 6, 12, and 18 months, an insurance status effect was demonstrated by a significant three-way interaction of intervention group, time, and insurance status. In the event of a significant insurance status effect, additional generalized estimating equation models were planned to test for differences between the intervention and usual-care groups on HSCL-20 scores for the insurance groups individually.
In addition, for each of the insurance groups, we used logistic regression models to estimate odds ratios and 95% confidence intervals for categorical variable secondary outcomes (percent with at least a 50% decrease in depressive symptom severity, Patient Global Improvement score, satisfaction with care, adherence to antidepressants, and four or more mental health visits). These odds ratios are presented to illustrate differences in time frames of recovery from depression between the intervention and usual-care groups, as well as quality of care across insurance groups.
Because comorbid PTSD and dysthymia may be associated with worse outcomes of depression treatment, we used the continuous PTSD score on the PTSD Checklist–Civilian Version and the dysthymia diagnosis by structured interview to evaluate effects of PTSD score and dysthymia by testing a three-way interaction by group, time, and PTSD severity or dysthymia diagnosis. We performed a sensitivity analysis including clinic site in the primary model. Lastly, we estimated intervention effect sizes (intervention minus usual-care group differences in change in depression score divided by the standard deviation of the depression scale), based on HSCL-20 depression scores at 12- and 18-month follow-up for the insurance groups, using Cohen’s d with a pooled variance estimate.
Results
A total of 120 (58.5%) patients had no insurance or relied on public coverage (63 with no insurance, 39 relying on Medicaid, 12 on Medicare, and six on Washington state) and 85 (41.5%) had commercial insurance. Patients in the no-insurance/public-coverage group were older on average; were less likely to be married or living with a partner, or to be white; had less social support, a greater number of medical disorders, and more PTSD symptoms; and were more likely to have comorbid dysthymia (
Table 1).
All women in the intervention arm received a similar number of in-person visits with depression care managers (no insurance/public coverage, mean=9.4 [SD=7.3]; commercial insurance, mean=9.9 [SD=6.9]). There was a nonsignificant difference between insurance-status groups in the number of telephone visits (no insurance/public coverage, mean=7.7 [SD=6.0]; commercial insurance, mean=5.5 [SD=6.3]).
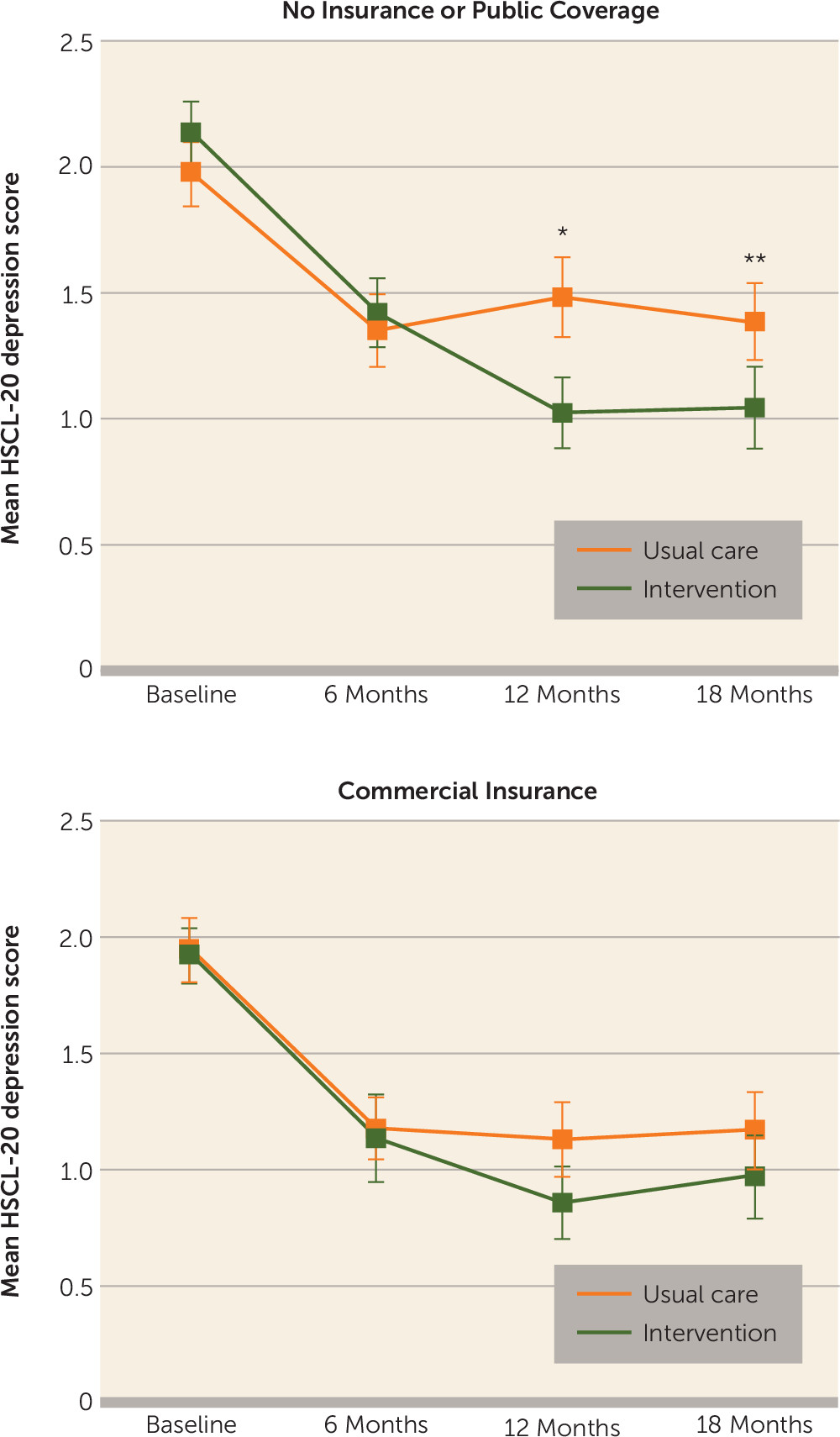
The treatment effect was significantly associated with insurance status (Wald χ
2=7.75, df=3, p=0.05). Patients with no insurance or with public coverage had greater recovery from depressive symptoms over the 18-month follow-up with the intervention than with usual care (Wald χ
2=27.63, df=3, p<0.0001), compared with those with commercial insurance (Wald χ
2=2.96, df=3, p=0.40) (
Table 2,
Figure 1). The effect size for depression improvement with the intervention compared with usual care was greater for women in the no-insurance/public-coverage group than for those in the commercial insurance group (at 12 months, d=0.81, 95% CI=0.41, 0.95, compared with d=0.39, 95% CI=–0.08, 0.84; at 18 months, d=0.59, 95% CI=0.43, 0.76, compared with d=0.23, 95% CI=0.07, 0.40).
There was no evidence that the treatment effect was associated with either comorbid PTSD or dysthymia (data not shown). Sensitivity analyses containing an indicator variable for clinic site did not change these results (data not shown).
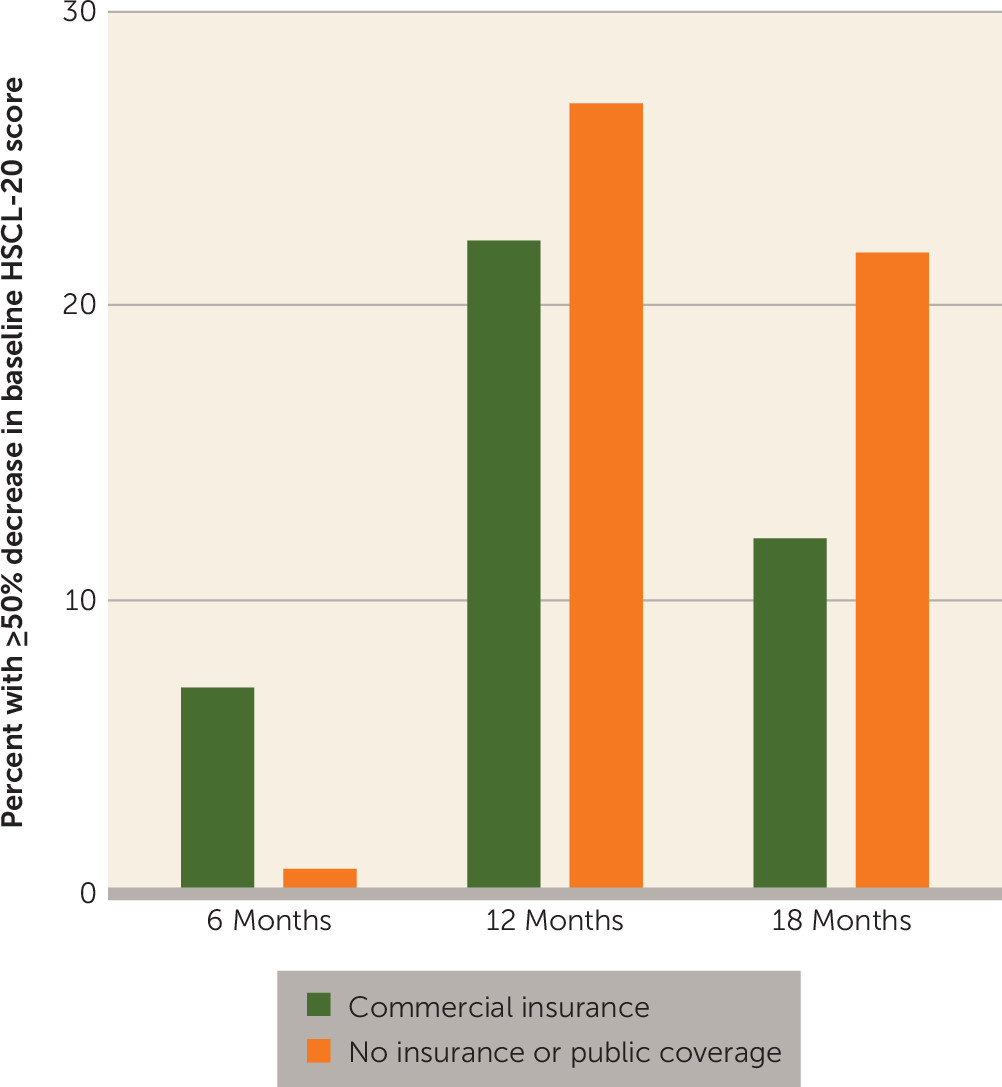
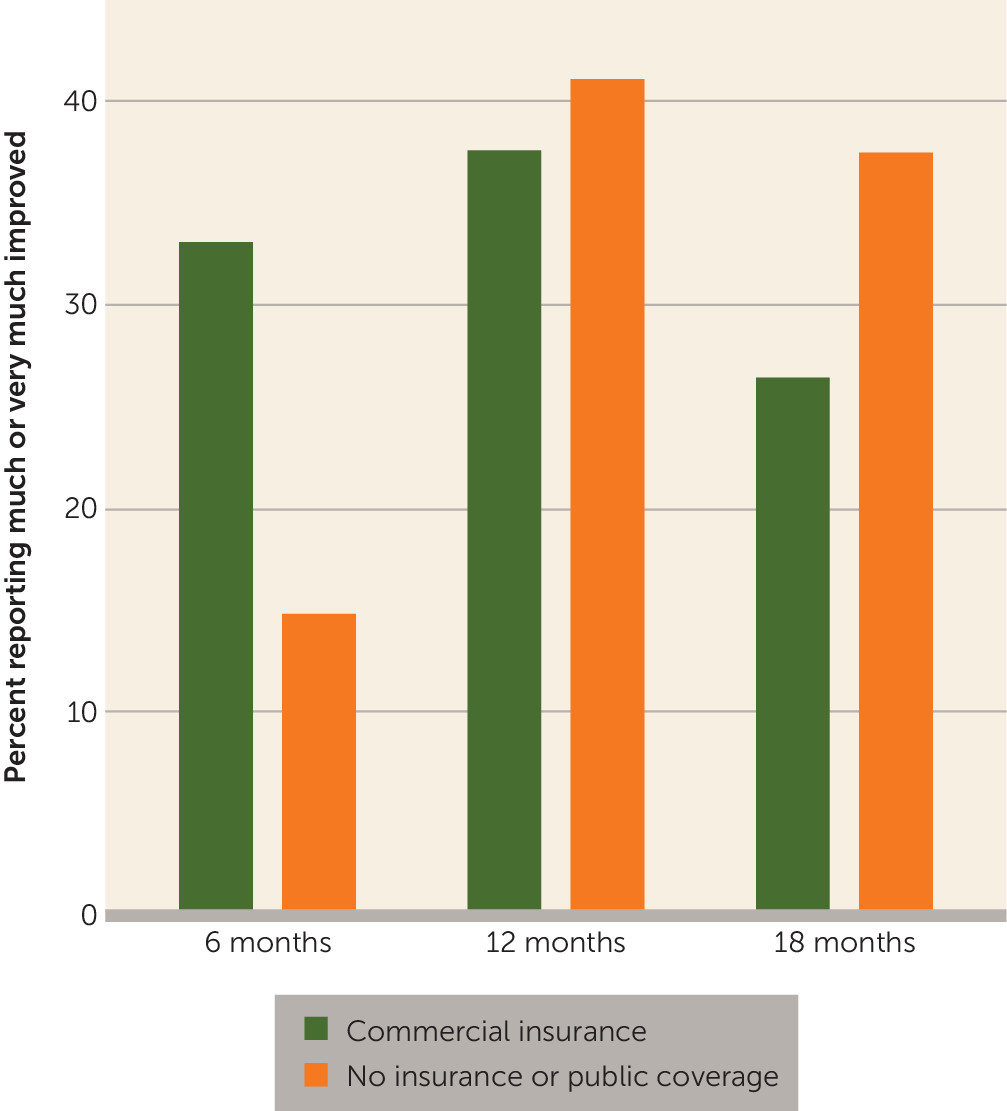
As shown in
Figures 2 and
3, based on clinical response (a decrease of at least 50% in depressive symptom severity and improvement on the Patient Global Improvement Scale), women with commercial insurance tended to improve sooner (at the 6-month follow-up) with the intervention than with usual care compared with women with no insurance or with public coverage. However, patients with no insurance or with public coverage tended to have greater improvements with the intervention than with usual care at 12 and 18 months on these measures compared with patients with commercial insurance.
For both insurance groups, the intervention was associated with a higher percentage of patients receiving four or more mental health visits compared with usual care (
Table 2). Similarly, for both insurance groups, patients receiving the intervention were more satisfied with the quality of depression care than usual-care patients; the greatest differences in satisfaction were in the commercially insured group. For the two antidepressant quality-of-care measures (percent taking an antidepressant for at least 25 of the past 30 days and percent taking an antidepressant for at least 3 of the past 6 months), the differences at 6 and 12 months between those receiving the intervention and those receiving usual care were more consistently significant among patients with no insurance or with public coverage than among those with commercial insurance.
Discussion
The DAWN intervention was found to be more effective than usual care at 12 and 18 months in treating women with no health insurance or with public coverage compared with women who had commercial insurance. With either insurance status, women who received the intervention had better quality of depression care than those who received usual care. The effect sizes observed for the DAWN intervention model (compared with usual care) at 12 months—0.39 for the insured women and 0.81 for those with no insurance or with public coverage—are both greater than the 0.27 effect size reported for collaborative depression care (compared with usual care) at 12 months in a recent meta-analysis of 79 studies of collaborative depression care provided in primary care (
31).
Clearly, having no insurance or relying on public coverage is a proxy for greater biopsychosocial vulnerability. In our sample, the women in the no-insurance/public-coverage group were older on average, were less likely to be white or living with a partner, had less social support, had a higher number of medical conditions, were more likely to meet criteria for comorbid dysthymia, and had more PTSD symptoms. Moreover, women with no insurance or with public coverage are less likely to be able to access specialty mental health services, which may contribute to a worsening of physical and mental health. The collaborative care intervention provided similar, and in some cases (such as antidepressant adherence) better, quality of care to this underserved, racially diverse population, and they experienced more benefit from the collaborative care intervention than did the commercially insured women.
The descriptive data on the effect of the intervention compared with usual care on percentage of women with at least a 50% decrease in depressive symptom severity and percentage rating themselves as “much” to “very much” improved on the Patient Global Impression Scale suggest that there was a lag in improvement at 6 months for the patients with no insurance or with public coverage compared with the commercially insured group. The greater likelihood of comorbid psychiatric and medical conditions and lower levels of social support among women in the no-insurance/public-coverage group may have delayed early recovery for this population. This more vulnerable group of patients is also likely to need more social interventions, such as help with securing charity care to pay for medications and housing, which may have delayed their initiation of or engagement in evidence-based treatments. However, as seen in the longitudinal data on depressive symptom severity and Patient Global Improvement scores, the difference between women receiving the intervention and those receiving usual care tended to be greater in the no-insurance/public-coverage group at 12 and 18 months. This may be explained in part by the better naturalistic recovery among the commercially insured women treated in usual care, as seen in
Table 2 and
Figure 1. Commercially insured women may improve more in usual care because they have fewer chronic social stressors, greater social support, less medical comorbidity, and more effective coping skills to work effectively with their physician to get effective treatment.
We tested whether higher levels of PTSD symptoms or chronicity of depression in the no-insurance/public-coverage group could have explained the difference in outcomes by insurance status. Socially disadvantaged women have higher rates of exposure to both childhood adversity and adult trauma, both of which are risk factors for the development and persistence of adult depressive and anxiety disorders (
7,
32,
33). As many as half of women with major depression have comorbid anxiety disorders, including PTSD, and studies suggest that comorbid anxiety is often associated with an incomplete response to depression treatment alone (
33,
34). Dysthymia has also been found to predict persistence of depression in primary care patients (
32). However, we did not find that either probable comorbid PTSD or dysthymia was associated with less response to the intervention compared with usual care.
Among the limitations of the study are that patients were recruited from university-affiliated OB/GYN clinics, which potentially limits generalizability to other OB/GYN populations; non-English speaking women were not included; and antidepressant adherence was based on self-report data. However, self-report questions on antidepressant adherence have shown high correlation with automated pharmacy refill data (
35). Women covered by Medicare were included in the no-insurance/public-coverage group because reimbursement for mental health visits is relatively low, and 10 of these 12 women were under age 65, which suggests chronic disability and limited fixed incomes. In addition, the limited sample size precluded any definitive study of the effect of insurance status on other important quality-of-care and clinical outcomes, such as the percentage with improvements of at least 50% in depressive symptom severity, Patient Global Improvement score, and use of antidepressants.
Previous data have shown that social disadvantage in women is associated with a higher risk of development of medical and psychiatric disorders, as well as more persistent depression (
1–
3,
5–
7), but the effect of insurance status on treatment outcomes is a relatively new finding. Gaps in accuracy of diagnosis of depression and quality of mental health treatment in OB/GYN clinics have been extensively documented, as well as lack of confidence by OB/GYN providers in delivering depression care (
15,
17). Our data show that collaborative depression care adapted to OB/GYN settings is effective in improving quality of mental health care and depression outcomes in socially disadvantaged populations who are uninsured or rely on public coverage. This is a relatively exciting and optimistic finding, in contrast to a belief that depression in socially disadvantaged women is recurrent, recalcitrant, and difficult to manage in any setting.
Acknowledgments
The authors thank Mr. Eddie Edmonton, Ms. Erin McCoy, Ms. Anna Harrington, Ms. Leiszle Ziemba, Ms. Virginia Eader for assistance with data collection and tracking, and Dr. Lee Cohen for chairing the data safety and monitoring board. They acknowledge Ms. Michal Inspektor and Ms. Julie Walwick (posthumously) for depression care management, and Dr. Nancy Grote for training depression care managers in the engagement session.