Rates of obesity in persons with serious mental illness are nearly twice those in the general population (
1–
3), contributing to reduced life expectancy in this group largely as a result of cardiovascular disease (
4–
6). Persons with serious mental illness face numerous challenges to achieving and sustaining fitness and weight loss, including the metabolic effects of psychoactive medications, the impact of symptoms on motivation, poor diet, difficulty affording healthy foods, physical inactivity, and inadequate access to safe, affordable, and supported options for physical exercise. Systematic reviews of health promotion interventions for persons with serious mental illness have identified at least 10 randomized trials reporting statistically significant overall weight loss (
7,
8), yet few studies have reported clinically significant outcomes (
9–
12). None of these clinically significant trials have been replicated to determine whether similar outcomes are achieved when the intervention is provided by routine community mental health organizations serving ethnically diverse populations or whether improved outcomes are sustained after the active intervention has been withdrawn.
In a previous randomized controlled trial in a mental health center in New Hampshire, we demonstrated the effectiveness of In SHAPE (
13), a 12-month program consisting of individual weekly meetings in the community with a health promotion coach, a fitness club (YMCA) membership, and nutrition education adapted for persons with serious mental illness (
14). We found that relative to an active comparison condition consisting of a fitness club membership alone, the In SHAPE intervention contributed to clinically significant reduction in cardiovascular risk (either clinically significant weight loss or improved fitness) in 49% of overweight/obese adults with serious mental illness.
Here we present the results of a pragmatic clinical trial of In SHAPE. A pragmatic or effectiveness trial assesses the effectiveness of the intervention as delivered in its usual clinical setting to the full range of patients for whom it is intended (
15). This trial was conducted to determine whether the primary outcomes of weight loss and improved fitness are replicated when the intervention is delivered by health promotion coaches employed by routine mental health provider organizations serving an ethnically diverse population of overweight/obese adults with serious mental illness. We also evaluated the secondary outcomes of body mass index (BMI), waist circumference, physical activity, diet, blood pressure, and serum lipid levels. Finally, we evaluated whether our primary outcomes of weight loss and improved fitness persisted after withdrawal of the active intervention. We hypothesized that the In SHAPE program contributes to greater reduction in weight and improvements in cardiorespiratory fitness when compared with a fitness club membership alone, and that these improvements are maintained at 18-month follow-up.
Method
Participants
Inclusion criteria were age 21 years or older; serious mental illness, defined as an axis I diagnosis of major depression, bipolar disorder, schizoaffective disorder, or schizophrenia (based on the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition [SCID;
16]) and persistent impairment in multiple areas of functioning (e.g., work, school, self-care); BMI >25; and provision of informed consent for participation. Participants were on stable pharmacological treatment, defined as having received the same psychiatric medications over the previous 2 months. Exclusion criteria were residence in a nursing home or other institution; a primary diagnosis of dementia; presence of significant cognitive impairment, defined as a score <24 on the Mini-Mental State Examination (
17); inability to walk one city block; pregnant or planning to become pregnant within the next 18 months; inability to speak English; terminal illness with mortality expected within 1 year; or a current diagnosis of an active substance dependence disorder (based on the substance abuse module of the SCID). The sample size was chosen to obtain 80% power for comparisons of the repeated time points at a significance level of 0.05 (two-sided) while assuming up to 20% attrition from baseline to 12 months. Pilot findings on waist circumference and fitness were used to anticipate effect size in these calculations (
14).
Study Procedures
Recruitment occurred between 2007 and 2011 from three nonprofit community mental health providers in the Boston area: Vinfen, Massachusetts Mental Health Center, and Bay Cove Human Services. Randomization between In SHAPE and the comparison condition was stratified by age (21 to 44 years versus 45 years and older) and psychiatric diagnosis (mood disorders versus schizophrenia spectrum disorders). Each combination of stratification categories had its own randomization schedule that was blocked on every fourth assignment to ensure balance between treatment arms. Randomization was conducted sequentially across all sites (not within sites).
Committees for the Protection of Human Subjects at Dartmouth College and the Department of Mental Health in Massachusetts approved the study procedures. Informed consent was obtained from all participants. Participants were paid for completing assessments, but not for attending In SHAPE sessions. Blinded assessments were conducted at baseline and at 3, 6, 9, 12, and 18 months for weight, BMI, waist circumference, and physical activity, and at baseline and at 6, 12, and 18 months for fitness, diet, blood pressure, and serum lipid levels.
Intervention
In SHAPE is a health promotion intervention consisting of a fitness club membership and a health promotion coach with basic certification as a fitness trainer who had received instruction on healthy eating and nutrition and training in tailoring individual wellness plans to the needs of persons with serious mental illness (
13,
14). Prior to enrollment, participants obtain medical clearance from their primary care provider. After conducting lifestyle and fitness evaluations, the health promotion coach develops a personalized fitness plan for each participant, using shared goal setting. Thereafter, coaches meet with participants individually each week for 45–60 minutes at a local fitness club (YMCA) and provide fitness coaching, support, and reinforcement for physical activity. The nutrition component consists of individualized instruction during each meeting, emphasizing healthy eating.
In SHAPE was delivered by four health promotion coaches who were either mental health case managers with basic certification in fitness training or certified fitness trainers interested in working with individuals with disabilities. All coaches also completed a 1-week In SHAPE training consisting of instruction in motivational interviewing, fitness goal setting, healthy nutrition, strategies for health behavior change, and tracking eating and physical activity behaviors. To ensure fidelity to the In SHAPE intervention, the health promotion coaches participated in two 60-minute supervision calls each week with an experienced certified fitness trainer, a clinical psychologist with expertise in behavior change and motivational interviewing, and a dietitian.
Comparison Condition
The comparison condition consisted of a fitness club membership to the same local fitness clubs (YMCAs) with an introductory session on safe use of the exercise equipment.
Primary Outcome Measures
Weight.
Weight (lb) was measured as the change in body weight over time.
Cardiorespiratory fitness.
Fitness was assessed with the 6-minute walk test (
18), which measures the distance an individual can walk in 6 minutes. In obese adults, the test is a reliable and valid measure of fitness, with favorable test-retest and discriminant validity (
19,
20), and it has been used in adults with a variety of chronic health conditions (
21–
30). An increase in distance of >50 meters (164 feet) is associated with a clinically significant reduction in risk for cardiovascular disease (
31,
32).
Secondary Outcome Measures
BMI.
BMI was calculated by dividing weight in kilograms by the square of height in meters.
Physical activity.
Physical activity was measured using the short-form International Physical Activity Questionnaire (
33). Summary scores were calculated for vigorous activities to obtain an estimate of weekly metabolic-equivalent-expenditure minutes of vigorous physical activity. The questionnaire is reliable and valid for use in persons with serious mental illness (
33). Health promotion coaches also collected self-report data on total exercise time per week. Frequency of fitness club visits was tracked using electronic records of membership card swipes at the YMCA.
Diet.
Readiness to change eating behaviors was assessed with a scale adapted from the Stages of Change Modified Motivational Interviewing instrument (
34), which focuses on dietary behaviors. Higher scores indicate greater readiness. We calculated an overall dietary behavior score consisting of the mean for the items related to portion control, consumption of fat, and intake of fruits and vegetables. Dietary intake was assessed using the Brief Block Food Frequency Questionnaire (
35), which yields estimates of daily consumption of calories and servings of fruits and vegetables. Its validity is comparable to that of other measures of diet, and it is sensitive to dietary intake over time (
36).
Blood pressure.
Blood pressure was measured before (resting heart rate) and after the 6-minute walk test.
Serum lipid levels.
Lipid levels were measured using the CardioChek PA Analyzer (Polymer Technology Systems, Indianapolis), a portable testing system that produces reliable values for total cholesterol, low- and high-density lipoproteins (LDL and HDL), and triglycerides using a multipanel test strip and a single drop of blood obtained by finger prick.
Statistical Analysis
The groups were compared for demographic characteristics, psychiatric history, and outcome measures at baseline using two-tailed t tests and chi-square tests. The primary outcome measures were changes in weight and fitness from baseline to 12 months and maintenance of outcomes from 12 to 18 months. Treatment effects were evaluated by intent-to-treat analyses, with total values for outcome measures as the dependent measures. To test our main hypotheses, we conducted analyses in two steps. In the first step, we examined group difference in outcome change for treatment period (baseline to 12 months). Rather than fitting parametric curves with random effects, we included baseline as a covariate and fitted baseline-adjusted mean response profile models (
37), also referred to as covariance pattern models (
38). Within-subject correlation over time was modeled by selecting unstructured covariance structures, and missing data were accommodated with maximum likelihood estimation (
39). The model was also adjusted for by including diagnosis and the interaction of group and diagnosis. Given that the outcomes were adjusted for baseline levels, treatment effects were evaluated by group main effects (i.e., differences in group mean response profiles during the treatment period). In the second step, we fitted models with group, time (12 to 18 months), and group-by-time interaction effect. We tested whether the primary and secondary outcomes were maintained after discontinuation of the 12-month intervention by examining the effect of the group-by-time interaction at 18 months. Generalized estimating equations were used to compare the percentages of participants in the two groups who met clinically significant weight loss and fitness criteria at 12 and 18 months. We computed Pearson’s correlation coefficients (r) to examine relationships between number of fitness trainer visits and weight loss and fitness.
Results
A total of 210 eligible participants were randomly assigned to the 12-month In SHAPE program (N=104) or to fitness club membership alone (N=106) (see the CONSORT diagram in the
data supplement that accompanies the online edition of this article). As shown in
Table 1, the study participants’ mean age was 43.9 years, and their mean BMI was 36.8; about half (51%) were female, and 46% were nonwhite (see the
data supplement for additional baseline characteristics). The In SHAPE group did not differ significantly from the comparison group in any baseline measures. Comparable 12-month and 18-month retention rates were observed across both groups (84% at 12 months and 77% at 18 months for the In SHAPE group, and 77% at 12 months and 78% at 18 months for the comparison group).
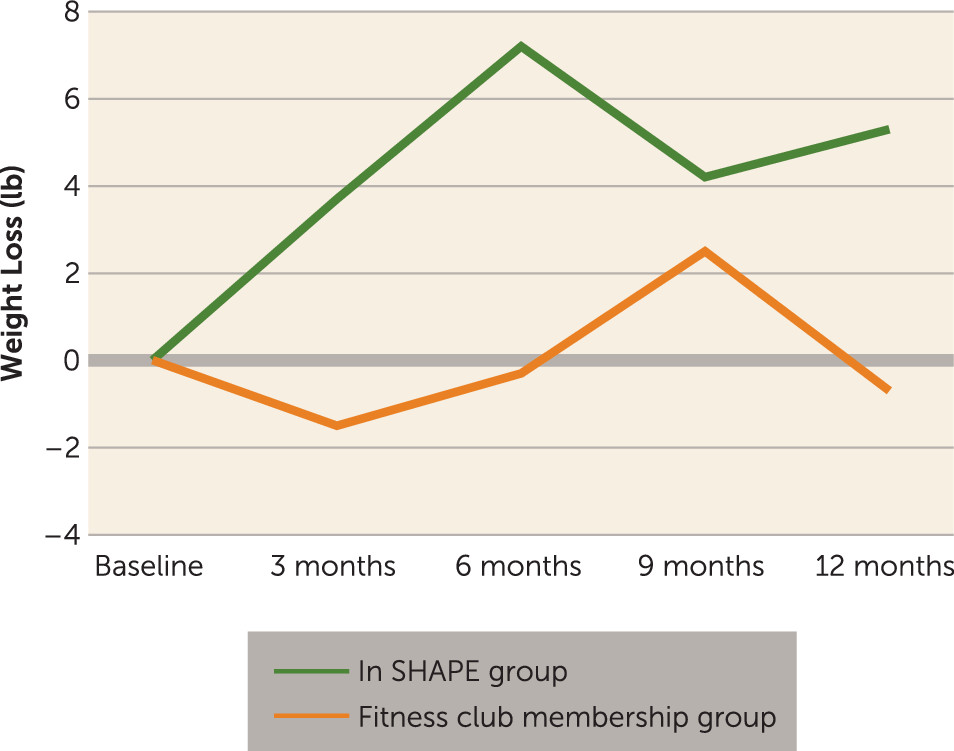
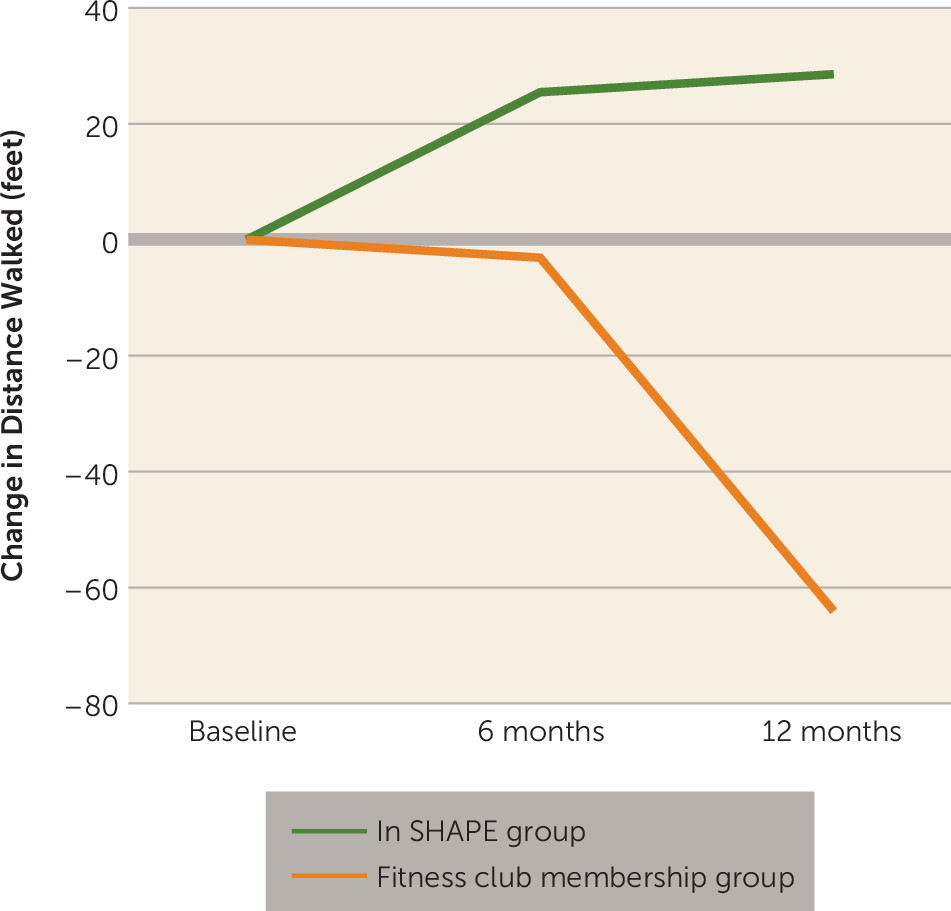
Results of intent-to-treat analyses at 3, 6, 9, and 12 months for the primary and secondary outcome measures are summarized in
Table 2. The In SHAPE intervention was associated with a significantly greater reduction in weight compared with fitness club membership alone (
Figure 1). The In SHAPE group also evidenced an increase in fitness as measured by the 6-minute walk test, compared with a small decrease in fitness in the fitness club membership only group (
Figure 2) (significant difference between groups). For the secondary outcome measures, the In SHAPE group achieved greater reductions in BMI and waist circumference and more minutes of physical activity. Diet, blood pressure, and serum lipid outcomes are summarized in
Table 3. There were greater self-reported improvements in eating behaviors, but no between-group differences in total calorie consumption, calories from fat or sweets, and consumption of fruits and vegetables. No between-group differences were observed in blood pressure or lipid values for the total sample, nor for the subgroup with abnormal lipid values at baseline (data not shown). No differences in outcomes were found with respect to age, gender, psychiatric diagnosis, or use of high- versus low-weight-gain-propensity psychiatric medications.
In addition to observed differences between groups, both the In SHAPE and comparison groups evidenced decreased weight and BMI and increased physical activity over time. For the total sample, there were decreases in total calorie consumption, calories from fat or sweets, and consumption of fruits and vegetables. The subgroup of participants across both groups with abnormal baseline lipid values showed significant reductions at 12 months for triglyceride levels (F=5.88, df=1, 64, p=0.018) and at 18 months for HDL levels (F=3.93, df=1, 101, p=0.050) and LDL levels (F=10.55, df=1, 18, p=0.004).
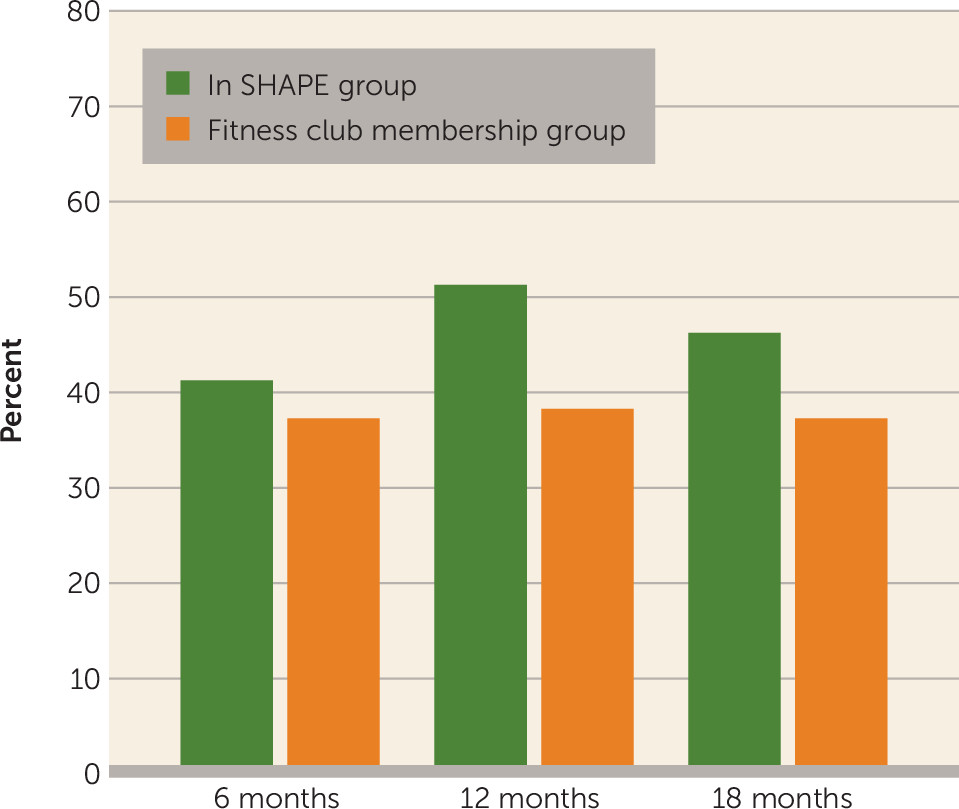
Primary weight and fitness outcomes and secondary outcomes were maintained from 12 to 18 months, as indicated by no group-by-time interactions, with the exception of decreases in readiness to change eating behaviors and increases in systolic blood pressure in the In SHAPE group relative to the comparison group (see the online
data supplement for outcomes from 12 to 18 months). At 12 months, over half (51%) of In SHAPE participants achieved clinically significant reduction in overall cardiovascular risk (either a weight loss ≥5% or an increase of >50 m [164 feet] on the 6-minute walk test), compared with 38% of those in the comparison group. Similar rates were observed at 18 months: 46% of In SHAPE participants compared with 37% of those in the comparison group (
Figure 3).
Frequency of visits to the gym was associated with weight loss at 12 months across both groups (r=0.28, p<0.01). The mean number of gym visits was more than two and a half times greater for the In SHAPE group relative to the comparison group (28.5 [SD=36.9] compared with 10.7 [SD=2.4]; t=−4.1, p<0.0001). In SHAPE participants attended a mean of 21.3 sessions (SD=12.6) with their health promotion coach (median=22.5 sessions), out of a possible 50 sessions. Attendance at sessions with the health promotion coach was correlated with weight loss (r=0.34, p=0.002) but not with improvement in fitness.
At 12 months, the gym membership was discontinued for both groups and regularly scheduled sessions with the health promotion coach ended for In SHAPE participants. A transitional support option to facilitate transitioning to community-based fitness activities was provided on request to In SHAPE participants at the end of the 12-month intervention. About half of the In SHAPE participants (N=44, 46%) had at least one additional contact in the first month after the end of the intervention (most consisting of a brief office visit, a telephone call, or going for a walk with the coach). At the 18-month follow-up, fewer than 16% (N=15) of participants were in contact with their health promotion coach. No differences were observed in the primary and secondary outcome measures at 12 and 18 months between In SHAPE participants who elected to have transitional support and those who did not.
Discussion
The In SHAPE intervention, compared with a fitness club membership alone, was associated with greater weight loss and improved fitness at 12 months, as well as sustained outcomes at 18 months. This study replicated our previous finding that about half of individuals receiving the In SHAPE intervention (49% in the first randomized trial and 51% in the present study) achieved a reduction in cardiovascular risk, defined as either clinically significant weight loss (≥5%) or clinically significant improvement in fitness (an increase of >50 meters [164 feet] on the 6-minute walk test).
We employed a pragmatic randomized clinical trial design (
15) to determine whether the effectiveness demonstrated in our previous trial (
13) would be replicated when delivering the In SHAPE program using health promotion coaches working at multiple urban community mental health organizations serving an ethnically and diagnostically diverse population. Our first randomized study was conducted with an ethnically homogeneous population (92% white) in a single mental health center in New Hampshire with access to a fitness club on the same block, and was intensively supervised by our research team, located in offices less than 1 mile away (
13). In contrast, this second study achieved similar effectiveness with remote supervision by our staff in a different state, involving ethnically diverse participants (46% nonwhite), in an urban setting (Boston), involving three different mental health organizations, and using multiple YMCA fitness clubs dispersed across the city. The results from this pragmatic trial confirm that comparable outcomes for the In SHAPE program can be achieved among individuals receiving services in community mental health organizations across diverse real-world settings.
To our knowledge, this is the first replication study confirming the effectiveness of a health coaching intervention in achieving clinically significant reductions in cardiovascular risk for overweight and obese persons with serious mental illness, and the first study to demonstrate persistent reduction in cardiovascular risk after the active intervention has been withdrawn. Half (51%) of In SHAPE participants achieved clinically significant reduction in cardiovascular risk when the intervention was completed at 12 months, and a similar reduction in risk persisted 6 months later (46%). Participants also continued to demonstrate improved health behaviors, including engaging in three times the amount of exercise at 18 months compared with baseline. We found an overall improvement in eating behaviors, although we did not find between-group differences in calorie intake (consumption of specific foods and categories of foods). This may reflect the focus of the health promotion coach, emphasizing consumption of healthier foods in contrast to focusing on portion control. Almost half of In SHAPE participants made use of optional transitional support to independent health promotion activities in the first month after completion of the intervention, but only a small subgroup (16%) continued to seek transitional support at 18 months, and no differential benefit was observed between those who received transitional support and those who did not.
By comparing In SHAPE to an active comparison condition (a fitness club membership), we were able to test the specific contribution of having a health promotion coach. Having a health promotion coach was associated with more than two and a half times the mean amount of fitness club attendance, which in turn was associated with greater weight loss and improved fitness. Our finding of no difference in reduction in lipid values between groups (despite overall improvements in HDL and LDL levels at 18 months for the total sample) may reflect the benefits of either intervention in risk reduction. Alternatively, the overall improvement in lipid values may be due to factors external to our study, although we did not detect any change in prescribing practices of antipsychotics or lipid-lowering agents during the period of follow-up assessments.
We replicated findings from our previous trial (
13) as well as the finding of clinically significant reduction in cardiovascular risk demonstrated in two other randomized trials of lifestyle interventions of a similar duration, sample size, and design: the Achieving Healthy Lifestyles in Psychiatric Rehabilitation (ACHIEVE) (
11) and STRIDE trials (
12). The ACHIEVE trial evaluated the effectiveness of an intensive 18-month group intervention conducted within psychiatric rehabilitation day treatment programs. The program consisted of two to three weekly intensive group exercise sessions and a weekly group weight management session, and it provided two meals a day emphasizing healthy food offerings. ACHIEVE was associated with clinically significant weight loss for 32.5% of participants at 12 months and 37.8% at 18 months (
11).
The STRIDE trial also evaluated a group-based weight loss intervention, but in contrast to ACHIEVE (which was provided as a component of a day treatment program), participants traveled to stand-alone group sessions focused on dietary changes in weekly 2-hour sessions, complemented by moderate physical activity (primarily consisting of walking). STRIDE resulted in clinically significant weight reduction for 40% of participants at 6 months and 47% at 12 months (
12).
In contrast to ACHIEVE and STRIDE, In SHAPE focused on improving overall physical fitness through individually tailored coached exercise in local YMCAs, coupled with individual coaching on healthy food choices. Results from these three studies confirm the effectiveness of lifestyle interventions for overweight and obese persons with serious mental illness in achieving clinically significant reduction in cardiovascular risk either through group or individual coaching, and for different degrees of intensity of dietary and exercise programming. It is likely that maximum benefit would be achieved through a multipronged approach combining intensive dietary modification and supported exercise, along with encouraging switching to psychiatric medications with low propensities for weight gain (
40,
41). In addition, the effectiveness of lifestyle interventions might be enhanced with pharmacological agents associated with weight loss, such as metformin (
42).
Several limitations warrant consideration when interpreting our results. First, we did not evaluate the effectiveness of In SHAPE or fitness club membership compared with usual care. However, this allowed us to specifically evaluate the impact of the health promotion coach on weight loss and improvement in fitness. Second, while the diagnostically and ethnically heterogeneous nature of our sample has the strength of broad clinical application, our sample size did not allow for evaluation of potential differences in outcomes that might be associated with psychiatric diagnosis or racial/ethnic subgroups. Finally, although we demonstrated persistence of outcomes 6 months after the end of the intervention, a longer follow-up period may be necessary to assess long-term cardiovascular risk reduction and to determine whether the intervention is associated with reduced health care service use and costs.
Despite these limitations, this study confirms that In SHAPE is associated with weight loss and improved fitness when offered by routine community-based provider organizations serving ethnically diverse participants with serious mental illness. However, there are numerous barriers to broad dissemination of health promotion as a component of community mental health services. Providing health promotion coaches and access to exercise facilities and affordable, healthy food will require significant changes in the way we finance and prioritize community mental health services.
Current efforts to increase life expectancy for persons with serious mental illness are focused on improving the quality and delivery of primary health care by integrating “health homes” within mental health care (
43). These initiatives address the inadequate access to and poor quality of health care experienced by persons with mental illness (
44). However, only 10%–15% of preventable mortality is estimated to be due to health care access and quality factors (
45), in contrast to health behaviors, which are estimated to account for the majority (57%) of a population’s health status and 40% of early deaths (
46). By also providing health promotion as a core service, it may be possible to further reduce early mortality while improving both the psychological and physical wellness of the whole person (
47).