Given that children who experience psychiatric problems at a young age are at an increased risk for impaired functioning and continued psychopathology later in life (
1,
2), characterization of any associated neurodevelopmental features is crucial. Neuroimaging offers a unique window on in vivo brain development and the associated features of mental illness (
3,
4). As the maturation of morphological (
5) and white matter microstructural (
6) features has been demonstrated with neuroimaging during childhood, the importance of examining emerging psychopathology in the context of typical brain development has been highlighted (
7). However, information is limited on the exact interplay between the emergence of psychiatric problems and corresponding trajectories of macro- and microstructural neurodevelopment.
There is a vast literature on structural neuroimaging studies of psychopathology. Broadly speaking, externalizing disorders, such as attention deficit hyperactivity disorder (ADHD), have frequently been tied to anomalies in fronto-striatal/fronto-cerebellar circuitry (
8,
9), and mood and anxiety disorders have been associated with anomalies in cortico-limbic circuitry (
10). However, findings have been inconsistent, and multiple psychiatric disorders have been found to exhibit spatial overlap in alterations across a broad range of anatomical areas, including those with cortico-limbic and cortico-striatal components. While previous work has been highly informative, much of it is characterized by two notable limitations. First, most studies are cross-sectional, limiting the inferences that can be drawn about developmental processes. Specifically, it is unclear whether early neural anomalies are associated with later psychopathology, or if the reverse relationship also holds (i.e., early psychopathology is tied to later neural anomalies). Longitudinal research, which combines the collection of clinical and imaging data at baseline and follow-up, can help disentangle the temporality of this relationship (
11). A second major limitation is that most studies have examined clinical samples, comparing cases and controls. However, many psychiatric symptoms exist on a continuum in the general population (
12). Larger, population-based studies have demonstrated that symptoms, when considered dimensionally, vary with neurobiological features, providing further support for this framework (
13,
14). However, to date, few studies have examined child psychiatric symptoms along a continuum in relation to longitudinal brain development (
15,
16).
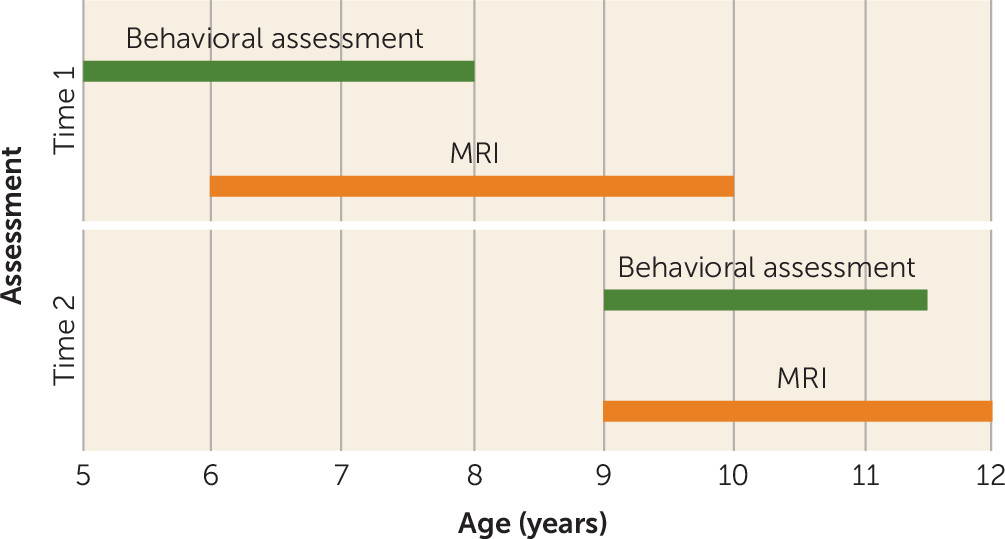
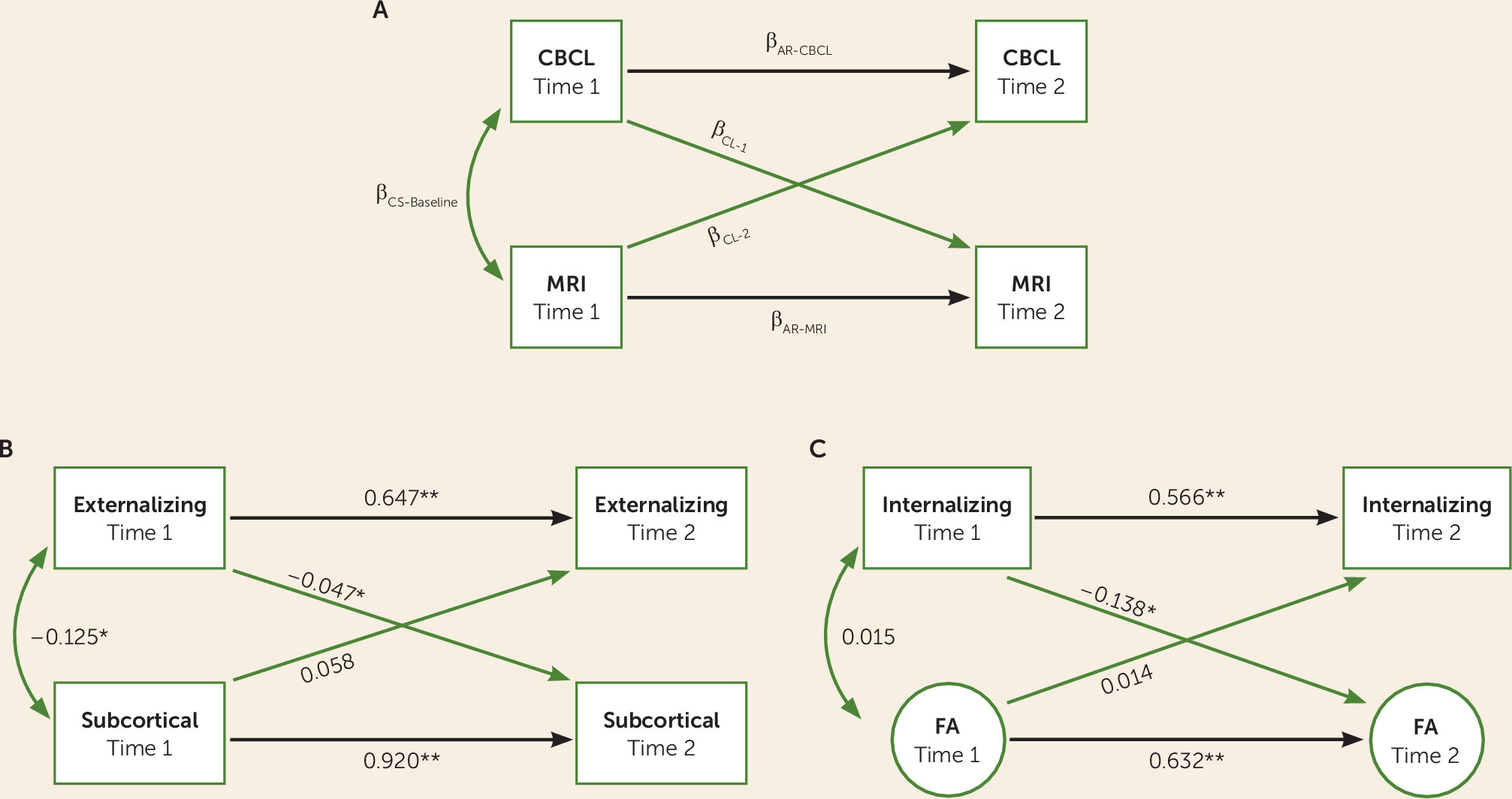
In the present study, we examined the bidirectional association of psychiatric problems with longitudinal gray and white matter microstructural development in a large sample of children from the general population. A dimensional approach was applied in the quantification of internalizing and externalizing problems, along with continuous measures of DSM symptom classes. We hypothesized that psychiatric problems along a continuum would be associated with altered anatomic and white matter microstructural development. In order to parse the precise direction of this relationship between brain and behavior over time, we used a cross-lagged panel model.
Discussion
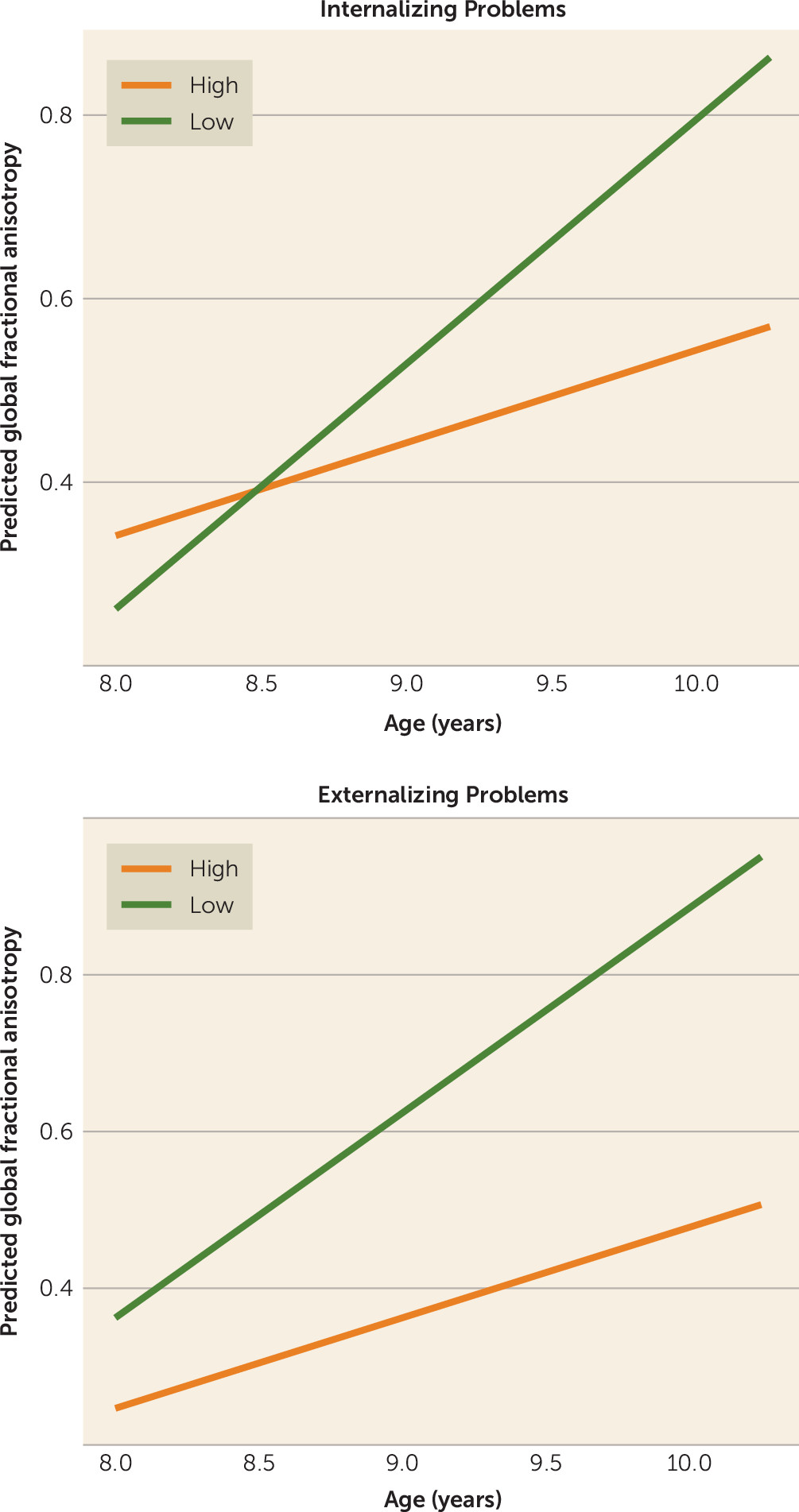
In this large population imaging study of children, we demonstrate a link between psychiatric problems along a continuum and a differential pattern of brain changes over time. Even in the general population, psychiatric problems were related to altered trajectories of both macro- and microstructural brain development. Interestingly, baseline brain metrics measured during childhood did not predict changes in psychiatric symptom ratings over time; instead, psychiatric problems at a young age predicted an altered pattern of brain changes over a 2½-year interval.
Consistent with the literature, this study shows that facets of psychopathology are related to smaller subcortical volumes and lower fractional anisotropy. The subcortex has been implicated to some degree in nearly all psychiatric disorders, and brain imaging studies have revealed evidence for its involvement in, for example, depression, ADHD, and obsessive-compulsive disorder (
8,
35,
36). Similarly, numerous studies have demonstrated the potential role of white matter microstructure in psychopathology (
10,
37). The present study expands on this literature by demonstrating that dimensionally assessed psychiatric problems are related to smaller changes in brain volume and fractional anisotropy over time. Most subcortical structures show increases in volume that peak during late childhood and into adolescence, followed by decreases in volume into adulthood (
38). Within the relatively narrow age range of the present sample, we show associations that are consistent with this previously reported pattern, and additionally show attenuated increases in subcortical volume that are related to both externalizing and internalizing problems. Fractional anisotropy in white matter has shown largely linear increases over time within this restricted age range (
6). Data from the present study fit with the literature, again additionally showing that these trajectories are potentially modified by the presence of psychiatric symptoms at an early age. Fractional anisotropy, but not mean diffusivity, showed a differential pattern of change. This could suggest differences in, for example, myelination or axonal packing.
Limited specificity was observed, as both externalizing and internalizing symptoms were associated with differential macro- and microstructural changes over time. Furthermore, three of the four DSM scales were associated with changes in white matter microstructure. As the two broadband domains are relatively highly correlated (
20), it is possible that the overlapping variance in these scales best explains the differential changes in the brain. Alternatively, given the relatively young age of the sample, it is also possible that domain-specific patterns of development become more apparent at older ages. In terms of symptom assessment, this study used parent reports of children’s psychiatric symptoms. It is likely that combining data from multiple informants (parents, teachers, and the children themselves) would provide a more robust and accurate picture of their symptom profile, which might in turn help to elucidate more specific correlates with neuroimaging features (
39). Along similar lines, although this study used high-resolution anatomical data and diffusion tensor imaging data, the two modalities were examined separately. It is possible that a multimodal approach in which both pieces of information were elegantly combined into a single analysis could help to disentangle unique neurobiological features in both categories of disorders (
40).
In the context of psychopathology, the most widely applied model in the field of neuroimaging has focused on identifying associated underlying neurobiological substrates of potential etiological significance. However, we did not find that early brain metrics predicted changes in psychiatric problems over time. There are several potential explanations for this. As this is not a clinical sample, it is possible that such processes are not part of a continuum and are not present in subclinical presentations of psychiatric constructs in the general population. It is thus a priority to determine whether these findings hold in large cohorts that are enriched for psychiatric disorders. Alternatively, the underlying neurobiological predictors of the emergence and development of psychopathology may be spatially or temporally heterogeneous, particularly during brain development, and more sophisticated image analysis methods may be needed to better characterize them (e.g., machine learning) (
41). It is also possible that the responsible underlying brain features are detectable at higher spatial resolution or perhaps using alternative imaging modalities (e.g., MR spectroscopy, MR perfusion, task-based or resting-state functional MRI).
The bulk of the findings in this study consisted of early measures of psychiatric problems predicting differential patterns of both macro- and microstructural brain development. This suggests that, in addition to the standard model of the brain shaping behavior discussed above, perhaps behaviors also shape the brain (
42). While there are undoubtedly underlying neurobiological explanations for the emergence of psychopathology in children, the data in this study suggest that psychiatric symptoms in children may also
contribute to some of the macro- and microstructural abnormalities reported in the literature—a potentially cascading interaction between psychopathology and the brain. Take the example of obsessive-compulsive disorder, where the symptomatology originates in a particular set of brain areas (e.g., fronto-striatal circuitry), but over time the symptoms themselves could modulate structural brain development (e.g., repetitive motor behaviors leading to alterations in the motor cortex) (
42). A similar extension can be drawn, in anxiety disorders, for example, to the potential effect of increased hypothalamic-pituitary-adrenal axis activity on the brain through downstream hormonal exposure (
43). A child with psychopathology may also experience his or her environment differently as a result of the disorder, which could consequently influence how the brain is shaped during development (e.g., reduced novelty seeking). The confounding effect of psychiatric treatment could also play a role (i.e., children with more psychiatric symptoms seek treatment, which subsequently influences brain development over time), although additional analyses in this study did not show that psychiatric medication status explained the association (see the
data supplement). Future studies should not rule out the possibility that, in addition to a preceding causal factor, observed neuroimaging associations with a given disorder could also be a downstream effect of the disorder.
Despite the large population-based sample, longitudinal design, and dimensional assessment of psychiatric symptoms, this study has important limitations. First, although the data for this study are part of a larger population-based study, representativeness is important to discuss. While many features of this sample are representative of the catchment area (e.g., ethnicity), some potentially are less so. For example, the mean nonverbal IQ in this sample was a few points above the population average. Although models adjusted for IQ proved to be similar to unadjusted models (see the data supplement), IQ remains an important consideration in child psychiatric studies, as it is often intertwined with clinical diagnosis and is related to many neuroimaging features. Next, as a hierarchical approach was implemented, some associations at a more focal level could have been missed; future work will benefit from analyzing brain and behavior at a more focal level. Regarding data acquisition, imaging data were acquired on two different MRI scanners, possibly introducing problems with the longitudinal interpretation of results. However, acquisitions were made as similarly as possible (e.g., gradient table, head coil, etc.), and a number of steps were introduced to mitigate such problems, including within-scanner normalization of MRI metrics (e.g., latent factor modeling within scanner, and Z-score standardization), which should attenuate the effects of scanner difference. Additionally, the statistical models used in this study to test the association between psychiatric problems and change in macro- and microstructural brain features operate on a relative rather than an absolute scale, further mitigating concerns about the effect of scanner. Lastly, only linear models were tested, as data were acquired at only two points in time. Gray matter morphological studies have shown the importance of nonlinear trajectories, and future work with additional time points should address this in more detail.
In conclusion, we demonstrate that internalizing and externalizing problems are related to altered macro- and microstructural changes in a large sample of children from the general population. Tracking the emergence of psychopathology in children, both in terms of symptomatology and neurobiology, may not only help guide diagnosticians but also improve the selection and timing of treatments. It is important to appreciate that this study does not challenge the causal role of neural changes in the pathogenesis of psychiatric disorders. Nonetheless, our findings raise the intriguing possibility that some emergent neuroimaging features of psychopathology may be partly a consequence of the disorder.