Only a small number of epidemiological studies have examined possible predisposing factors to functional limb weakness (
2–
4) or hyperkinetic functional movement disorders (
5–
8). In previous studies, we reported on the frequency, clinical features, comorbid psychiatric disorders and somatic symptoms, physical disability, and illness beliefs of a prospective cohort of 107 patients with functional limb weakness (
9), as well as factors at illness onset, including physical precipitating events (
10), and illness perceptions among family members (
11). In the present study, we report additional data from the same sample covering a range of possible predisposing or antecedent risk factors for functional limb weakness on the basis of existing etiological models of FND (
12).
We aimed to test whether there were differences in hypothesized predisposing factors between a patient group with functional limb weakness and a control group comprising individuals with recent-onset limb weakness attributed to neurological disease and healthy persons. To do this, we gathered data on family structure, frequency of adverse childhood experiences, personality traits, medical and surgical illness, and exposure to a symptom model. On the basis of the literature available, we hypothesized that compared with control subjects, case patients with functional limb weakness would be overrepresented as the youngest among siblings and have a higher frequency of adverse childhood experiences, altered personality traits (especially neuroticism), a higher frequency of other previous functional disorders and surgical procedures, and a higher exposure to a model for their symptoms.
Discussion
FNDs have been linked historically to a variety of presumed predisposing etiological factors, but there has been relatively little empirical testing of these hypotheses. Since Freud and Breuer in 1895 (
16), psychological stressors, and particularly adverse childhood events, have been enshrined for most of the last century in the term “conversion hysteria” and then “conversion disorder” in DSM-IV. In DSM-5 conversion disorder no longer requires a recent stressor as a diagnostic criterion, recognizing that for two patients with identical functional motor symptoms, one may have a stressor and one may not (
17).
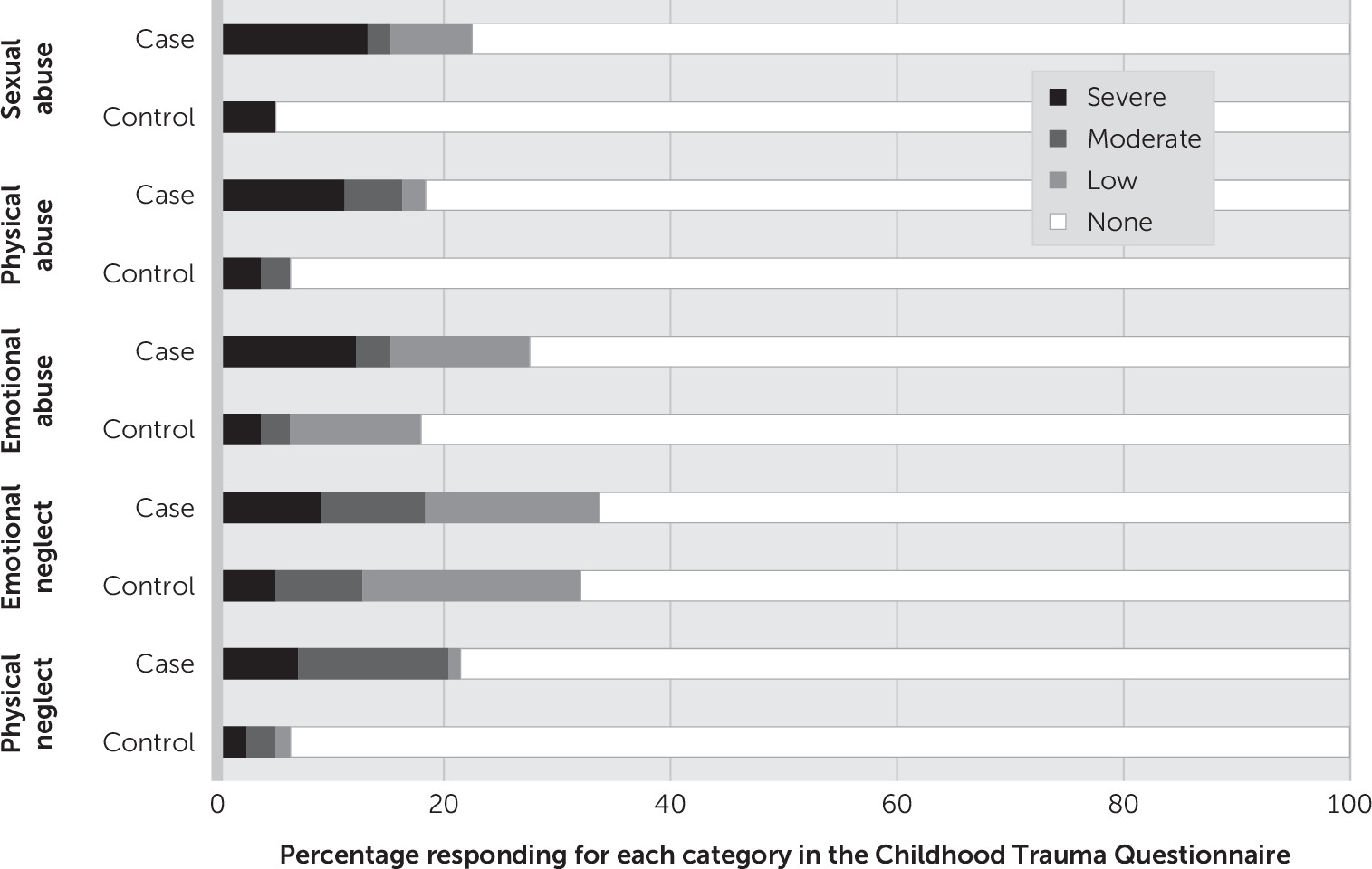
In our study, one of the largest reported controlled studies of functional motor disorders, there was indeed a higher frequency of adverse childhood and adult experience in the patients with functional limb weakness compared with control subjects. However, more than half of the participants reported no experience of abuse; sexual abuse, in particular, was relatively infrequent. Adverse child and adult experiences, even when inquired about in broader terms, were found in three or four in 10 case patients and two in 10 control subjects. Similar frequencies were obtained by interview question and by questionnaire assessment.
Other studies from neurological settings looking specifically at functional motor disorders have failed to show as much difference as might be expected in rates of childhood abuse between case patients and control subjects with neurological conditions (for further details, see Table S2 in the
online supplement). For example, a study of 30 patients with acute functional limb weakness in Sweden found that only 3% had a history of childhood sexual abuse, versus none in the control group (
2,
3). A study of 64 patients with functional movement disorder with a duration of 6 years also failed to demonstrate a difference from healthy control subjects with respect to sexual abuse, although there were differences for physical and emotional abuse (
5). In contrast, a large study of 322 patients with functional motor disorders (50% of whom had functional limb weakness, with an average duration of 14 years) found high rates of adverse childhood experience and traumatic life events but with no difference from psychiatric control subjects (
4).
This rate of childhood abuse is consistent with the results of a systematic review and meta-analysis of 34 controlled studies of stressful life events and childhood maltreatment in FND in 1,405 patients, with 65% of the data coming from patients with dissociative (nonepileptic) seizures (
18). A summary of this review in context with the present study and another large cohort study is presented in Tables S2 in the
online supplement. The review found the highest odds ratios for emotional neglect (case patients, 49% versus control subjects, 20%, odds ratio=5.6, 95% CI=2.4–13.1) with smaller values for sexual abuse (24% versus 10%, odds ratio=3.3, 95% CI=2.2–4.8) and physical abuse (30% versus 12%, odds ratio=3.9, 95% CI=2.2–7.2). The overall picture is one in which adverse childhood experience emerges as a clear risk factor for functional motor disorders, but one that varies considerably according to setting and duration of symptoms and is not present in a majority of patients. These experiences appear to occur at a frequency similar to that found in people with psychiatric disorders and other conditions, including other functional disorders and migraine (
19). Frequency of antecedent abuse appeared to increase with the mean duration of symptoms, which raises the question of whether adverse experiences are sometimes as important in creating the conditions for more prolonged symptoms rather than the initial symptoms themselves (for further details, see Table S2 in the
online supplement). Similar conclusions are emerging in studies of migraine (
20).
Birth order has been mooted as a predisposing factor for FNDs. Kraepelin (
21) proposed that first-born children might be more vulnerable, a concept that arose more because of considerations about perinatal injury than emotional development. Conversely, last-born children have been hypothesized to be more vulnerable to functional disorders because of being the baby of the family. However, the data do not support these suggestions. In 1957, Ljungberg (
21), in his large study of 381 patients with hysteria, found no differences in birth order. Neither did a study conducted in Libya (
22) or a controlled study of 30 patients with acute functional motor disorder (
2). In the presents study, we also found no difference, an observation that should encourage clinicians to be circumspect about considering this to be a predisposing factor.
Certain personality traits also have a long historical association with functional motor disorders. Since the origin of the concept of hysteria, the diagnosis has often been confused with the idea of the hysterical or histrionic personality. Studies of personality in people with FND have generally focused on personality disorder (especially cluster B disorders). This, like adverse experience, is more common in people with FND but still only present in a minority and with large variations in reported frequency (
2,
6,
7,
23). Neuroticism has historically been suggested as an important vulnerability, although few studies have examined the distribution of normal personality traits, rather than personality disorder, in patients with FND (
24). The differences we found for both traits, higher neuroticism and lower openness, in FND were small to medium in effect size, the former in keeping with higher frequencies of depression and anxiety in FND (
9). Previous studies of the NEO domains in functional motor disorders have found lower conscientiousness (
5) (64 patients with functional movement disorder versus 39 healthy control subjects), lower extraversion and openness (
6) (39 patients with functional dystonia versus 30 patients with primary dystonia) and no difference (
8) (59 patients with functional movement disorder versus 26 healthy control subjects). Personality traits have been shown to correlate with resilience in functional motor disorders, but this is also likely to be the case with control subjects (
25). Taking into account the modest effect sizes seen in this study and the variable results from studies reported thus far, we conclude that there are no consistently found personality traits in patients with functional motor disorders compared with control subjects.
The data on medical and surgical comorbid conditions produces a clearer pattern, consistent with the published literature. There were high rates of surgical procedures, a useful variable to measure since it tends to be verifiable and binary. These data were collected at a time when hysterectomy for menorrhagia and dysmenorrhea was more common. We were not able to establish to what extent surgery was carried out for proven pathological disease. A history of neurological and other disease diagnoses is common in FND and has long been recognized as an important risk factor (
26–
28). Excess surgery could have arisen from comorbid conditions or from surgery carried out for symptom complaints in the absence of pathophysiological disease. The high rate of sterilization is interesting, given that the samples were comparable in gender. This might suggest more willingness to undergo surgical procedures. We excluded comorbid neurological disease, but this should not have influenced data on comorbid functional disorders.
Data from 3,781 neurology outpatients in Scotland showed that patients with a primary functional disorder diagnosis tended to have more physical symptoms than patients with a recognized neurological disease (
29). Studies of dissociative (nonepileptic) seizures have shown consistently high rates of physical symptom comorbid condition. For example, a study of 158 patients with dissociative seizures showed that 66% had one or more of fibromyalgia, chronic fatigue syndrome, chronic pain, or irritable bowel syndrome, compared with 27% of patients with epilepsy (
30). In patients with functional motor disorders, several studies have shown higher rates of physical symptoms (
6,
7). Clinically there are areas such as complex regional pain syndrome (
31) and scan-negative cauda equina syndrome (
32) where pain disorders and functional motor disorders clearly overlap. Several papers have explored the overlap between FND and migraine (
33,
34), but we are not aware of similar data on specific comorbid functional disorder diagnoses, migraine, or surgical history in another descriptive series of functional motor disorder.
The idea that patients with functional motor disorders might develop their symptoms partly because of exposure to a symptom model in their environment also goes back a long way in the literature, at least as far as Janet’s idée fixe (
35). It is a difficult problem to study and arguably an unfalsifiable hypothesis, if modeling includes sources as diverse as seeing a television advertisement about stroke or having a close relative with a neurological disorder. In one of the largest studies of modeling, 132 patients with functional movement disorders were found to have the same proportion of health care workers as 148 control subjects (
13), going against a commonly promoted stereotype. In a study of 322 patients with functional motor disorder, 19% were employed or had been employed in caring roles compared with 8% of psychiatric control subjects. A study of 29 patients with functional movement disorder found that 55% had exposure to a neurological disease compared with 24% of 50 control subjects (
36). This study was carried out retrospectively using chart review by a team who considered that modeling might be a diagnostic feature, and so may have been affected by measurement bias. Disease modeling was recorded in 58% versus 31% of 31 patients with functional versus 31 with structural motor disorder (
7). In our study we found statistically significant differences in some of the analyses, but the multiple comparisons and the high frequency in control subjects makes it clear that modeling is not a clinical feature of diagnostic use. As an etiological factor its measurement is heavily prone to bias and its relevance remains uncertain.
Limitations
Our study benefits from a prospectively collected sample of patients with functional limb weakness that is a representative sample of outpatient and inpatient neurological practice and symptoms of short duration. We also had serendipitous matching of age and sex with our control subjects. However, case-control studies are notoriously subject to bias and confounding: the issues of representativeness, misdiagnosis, and selection of controls are explored in another paper (
9). Additionally, our sample was small enough to risk a high chance of type 2 false negative errors. The interviewer (JS) was not blinded to diagnosis, leaving open the possibility of measurement bias, especially in interview ratings of adverse experience. We have not corrected for multiple comparisons in this paper and suggest that differences with a significance between a p value >0.01 and <0.05 should be treated with caution. We have not carried out correlations between variables reported in this paper and other published data from this study (
9) to investigate confounding, for example by psychiatric disorder.